Abstract
Introduction
Acute gastrointestinal obstruction due to colorectal cancer occurs in 7–30% of cases and is an abdominal emergency that requires urgent decompression. The safety and oncological effect of self-expandable metal stents (SEMS) in these patients remains controversial. This study aimed to evaluate its impact on these variables and compare it with that of emergency surgery (ES).
Methods
Descriptive, retrospective and single-centre study, performed between 2008 and 2015, with follow-up until 2017. One hundred eleven patients with diagnosis of left malignant colonic obstruction were included and divided according to the treatment received: stent as bridge to surgery (SBTS group: 39), palliative stent (PS group: 30) and emergency surgery with curative (ECS group: 34) or palliative intent (EPS group: 8). Treatment was decided by the attending surgeon in charge.
Results
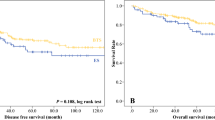
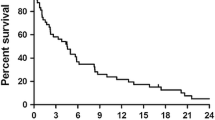
Technical and clinical general success rates for colorectal SEMS were 95.7% and 91.3%, respectively, with an associated morbimortality of 23.2%, which was higher in the PS group (p = 0.002). The SBTS group presented a higher laparoscopic approach and primary anastomosis (p < 0.001), as well as a lower colostomy rate than the ECS group (12.8% vs. 40%; p = 0.023). Postoperative morbidity and mortality were significantly lower in the SBTS group compared to the ECS group (41% vs. 67.6%; p = 0.025). Overall survival (OS) and disease-free survival (DFS) were similar between the analysed groups.
Conclusion
Colonic stent placement is a safe and effective therapeutic alternative to emergency surgery in the management of left-sided malignant colonic obstruction in both curative and palliative fields. It presents a lower postoperative morbimortality and a similar oncological prognosis.


Similar content being viewed by others
References
Kyllönen LE (1987) Obstruction and perforation complicating colorectal carcinoma. An epidemiologic and clinical study with special reference to incidence and survival. Acta Chir Scand 153(10):607–614 (PMID: 3434101)
Pavlidis TE, Marakis G, Ballas K, Rafailidis S, Psarras K, Pissas D, Sakantamis AK (2008) Does emergency surgery affect resectability of colorectal cancer?. Acta Chir Belg 108(2):219–225. https://doi.org/10.1080/00015458.2008.11680207 (PMID: 18557147)
Dohmoto M, Rupp KD, Hohlbach G (1990) Endoskopisch implantierte Prothese beim Rektumkarzinom [Endoscopically-implanted prosthesis in rectal carcinoma]. Dtsch Med Wochenschr 115(23):915. German. PMID: 2354663
Dauphine CE, Tan P, Beart RW Jr, Vukasin P, Cohen H, Corman ML (2002) Placement of self-expanding metal stents for acute malignant large-bowel obstruction: a collective review. Ann Surg Oncol 9(6):574–579. https://doi.org/10.1007/BF02573894 (PMID: 12095974)
Flor-Lorente B, Báguena G, Frasson M, García-Granero A, Cervantes A, Sanchiz V, Peña A, Espí A, Esclapez P, García-Granero E (2017) Self-expanding metallic stent as a bridge to surgery in the treatment of left colon cancer obstruction: cost-benefit analysis and oncologic results. Cir Esp 95(3):143–151. English, Spanish. https://doi.org/10.1016/j.ciresp.2016.12.014. Epub 2017 Mar 21. PMID: 28336185
Fernández-Esparrach G, Bordas JM, Giráldez MD, Ginès A, Pellisé M, Sendino O, Martínez-Pallí G, Castells A, Llach J (2010) Severe complications limit long-term clinical success of self-expanding metal stents in patients with obstructive colorectal cancer. Am J Gastroenterol 105(5):1087–1093. https://doi.org/10.1038/ajg.2009.660 (Epub 2009 Nov 24 PMID: 19935785)
Kim EJ, Kim YJ (2016) Stents for colorectal obstruction: past, present, and future. World J Gastroenterol 22(2):842–852. https://doi.org/10.3748/wjg.v22.i2.842.PMID:26811630;PMCID:PMC4716082
Lee YJ, Yoon JY, Park JJ, Park SJ, Kim JH, Youn YH, Kim TI, Park H, Kim WH, Cheon JH (2018) Clinical outcomes and factors related to colonic perforations in patients receiving self-expandable metal stent insertion for malignant colorectal obstruction. Gastrointest Endosc 87(6):1548–1557.e1. https://doi.org/10.1016/j.gie.2018.02.006 (Epub 2018 Feb 13 PMID: 29452077)
Maruthachalam K, Lash GE, Shenton BK, Horgan AF (2007) Tumour cell dissemination following endoscopic stent insertion. Br J Surg 94(9):1151–1154. https://doi.org/10.1002/bjs.5790 (PMID: 17541987)
Turnbull RB Jr, Kyle K, Watson FR, Spratt J (1967) Cancer of the colon: the influence of the no-touch isolation technic on survival rates. Ann Surg 166(3):420–427. https://doi.org/10.1097/00000658-196709000-00010.PMID:6039601;PMCID:PMC1477415
Kim SJ, Kim HW, Park SB, Kang DH, Choi CW, Song BJ, Hong JB, Kim DJ, Park BS, Son GM (2015) Colonic perforation either during or after stent insertion as a bridge to surgery for malignant colorectal obstruction increases the risk of peritoneal seeding. Surg Endosc 29(12):3499–3506. https://doi.org/10.1007/s00464-015-4100-6 (Epub 2015 Feb 13 PMID: 25676202)
Gorissen KJ, Tuynman JB, Fryer E, Wang L, Uberoi R, Jones OM, Cunningham C, Lindsey I (2013) Local recurrence after stenting for obstructing left-sided colonic cancer. Br J Surg 100(13):1805–1809. https://doi.org/10.1002/bjs.9297 (PMID: 24227368)
Knight AL, Trompetas V, Saunders MP, Anderson HJ (2012) Does stenting of left-sided colorectal cancer as a bridge to surgery adversely affect oncological outcomes? A comparison with non-obstructing elective left-sided colonic resections. Int J Colorectal Dis 27(11):1509–1514. https://doi.org/10.1007/s00384-012-1513-8 (Epub 2012 Jun 9 PMID: 22684548)
Sloothaak DA, van den Berg MW, Dijkgraaf MG, Fockens P, Tanis PJ, van Hooft JE, Bemelman WA, Collaborative Dutch Stent-In Study Group (2014) Oncological outcome of malignant colonic obstruction in the Dutch Stent-In 2 trial. Br J Surg 101(13):1751–1757. https://doi.org/10.1002/bjs.9645 (Epub 2014 Oct 9 PMID: 25298250)
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240(2):205–213. https://doi.org/10.1097/01.sla.0000133083.54934.ae (PMID:15273542;PMCID:PMC1360123)
World Medical Association Declaration of Helsinki (1997) Recommendations guiding physicians in biomedical research involving human subjects. JAMA 277(11):925–926 (PMID: 9062334)
Cennamo V, Luigiano C, Coccolini F, Fabbri C, Bassi M, De Caro G, Ceroni L, Maimone A, Ravelli P, Ansaloni L (2013) Meta-analysis of randomized trials comparing endoscopic stenting and surgical decompression for colorectal cancer obstruction. Int J Colorectal Dis 28(6):855–863. https://doi.org/10.1007/s00384-012-1599-z (Epub 2012 Nov 15 PMID: 23151813)
Tan CJ, Dasari BV, Gardiner K (2012) Systematic review and meta-analysis of randomized clinical trials of self-expanding metallic stents as a bridge to surgery versus emergency surgery for malignant left-sided large bowel obstruction. Br J Surg 99(4):469–476. https://doi.org/10.1002/bjs.8689 (Epub 2012 Jan 19 PMID: 22261931)
Ho KM, Chan KM, Kwok SY, Lau PY (2017) Colonic self-expanding metal stent (SEMS) as a bridge to surgery in left-sided malignant colonic obstruction: an 8-year review. Surg Endosc 31(5):2255–2262. https://doi.org/10.1007/s00464-016-5227-9 (Epub 2016 Sep 8 PMID: 27631312)
Matsuda A, Miyashita M, Matsumoto S, Matsutani T, Sakurazawa N, Takahashi G, Kishi T, Uchida E (2015) Comparison of long-term outcomes of colonic stent as bridge to surgery and emergency surgery for malignant large-bowel obstruction: a meta-analysis. Ann Surg Oncol 22(2):497–504. https://doi.org/10.1245/s10434-014-3997-7 (Epub 2014 Aug 14 PMID: 25120255)
Cao Y, Gu J, Deng S, Li J, Wu K, Cai K (2019) Long-term tumour outcomes of self-expanding metal stents as bridge to surgery for the treatment of colorectal cancer with malignant obstruction: a systematic review and meta-analysis. Int J Colorectal Dis 34(11):1827–1838. https://doi.org/10.1007/s00384-019-03372-5 (Epub 2019 Sep 12 PMID: 31515615)
Mege D, Sabbagh C, Manceau C, Bridoux V, Lakkis Z, Momar D, Sielezneff I, Karoui M, AFC (French Surgical Association) Working Group (2019) What is the best option between primary diverting stoma or endoscopic stent as a bridge to surgery with a curative intent for obstructed left colon cancer? Results from a propensity score analysis of the French surgical association multicenter cohort of 518 patients. Ann Surg Oncol 26(3):756–764. https://doi.org/10.1245/s10434-018-07139-0 (Epub 2019 Jan 8 PMID: 30623342)
Lara-Romero C, Vilches Á, Caunedo-Álvarez Á, Hergueta-Delgado P, Lavín-Castejón I, Andrade-Bellido R, Alcaín-Martínez G (2019) Better recurrence-free survival after stent bridge to surgery compared to emergency surgery for obstructive left-sided colonic cancer in patients with stage III status of the American Joint Committee on Cancer (AJCC): a bicentric retrospective study. Int J Colorectal Dis 34(7):1241–1250. https://doi.org/10.1007/s00384-019-03318-x (Epub 2019 May 25 PMID: 31129696)
Balciscueta I, Balciscueta Z, Uribe N, García-Granero E (2021) Perineural invasion is increased in patients receiving colonic stenting as a bridge to surgery: a systematic review and meta-analysis. Tech Coloproctol 25(2):167–176. https://doi.org/10.1007/s10151-020-02350-2 (Epub 2020 Nov 17 PMID: 33200308)
Yoon JY, Jung YS, Hong SP, Kim TI, Kim WH, Cheon JH (2011) Clinical outcomes and risk factors for technical and clinical failures of self-expandable metal stent insertion for malignant colorectal obstruction. Gastrointest Endosc 74(4):858–868. https://doi.org/10.1016/j.gie.2011.05.044 (Epub 2011 Aug 20 PMID: 21862005)
Genzor Ríos SJ, González-Nicolás Trebol MT, Aguirre Prat N, Cantalejo Díaz M, Rodríguez Artigas JM, Medrano Peña J, Zaragozano Guillén R, Miguelena Bobadilla JM (2019) Stent performance in obstructive left colon cancer. Unicentric and cross-sectional study. Cir Esp 97(7):397–404. English, Spanish. https://doi.org/10.1016/j.ciresp.2019.04.018. Epub 2019 Jun 2. PMID: 31167747
Neo VSQ, Jain SR, Yeo JW, Ng CH, Gan TRX, Tan E, Chong CS (2021) Controversies of colonic stenting in obstructive left colorectal cancer: a critical analysis with meta-analysis and meta-regression. Int J Colorectal Dis 36(4):689–700. https://doi.org/10.1007/s00384-021-03834-9 (Epub 2021 Jan 25 PMID: 33495871)
Crespí-Mir A, Romero-Marcos JM, de la Llave-Serralvo A, Dolz-Abadía C, Cifuentes-Ródenas JA (2018) Impact on surgical and oncological results of the use of colonic stents as a bridge to surgery for potentially curable occlusive colorectal neoplasms. Cir Esp 96(7):419–428. English, Spanish. https://doi.org/10.1016/j.ciresp.2018.03.005. Epub 2018 Apr 16. PMID: 29669684
Allievi N, Ceresoli M, Fugazzola P, Montori G, Coccolini F, Ansaloni L (2017) Endoscopic stenting as bridge to surgery versus emergency resection for left-sided malignant colorectal obstruction: an updated meta-analysis. Int J Surg Oncol 2017:2863272. https://doi.org/10.1155/2017/2863272. Epub 2017 Jul 5. PMID: 28761765; PMCID: PMC5516723
Arezzo A, Balague C, Targarona E, Borghi F, Giraudo G, Ghezzo L, Arroyo A, Sola-Vera J, De Paolis P, Bossotti M, Bannone E, Forcignanò E, Bonino MA, Passera R, Morino M (2017) Colonic stenting as a bridge to surgery versus emergency surgery for malignant colonic obstruction: results of a multicentre randomised controlled trial (ESCO trial). Surg Endosc 31(8):3297–3305. https://doi.org/10.1007/s00464-016-5362-3 (Epub 2016 Dec 6 PMID: 27924392)
Sabbagh C, Browet F, Diouf M, Cosse C, Brehant O, Bartoli E, Mauvais F, Chauffert B, Dupas JL, Nguyen-Khac E, Regimbeau JM (2013) Is stenting as “a bridge to surgery” an oncologically safe strategy for the management of acute, left-sided, malignant, colonic obstruction? A comparative study with a propensity score analysis. Ann Surg 258(1):107–115. https://doi.org/10.1097/SLA.0b013e31827e30ce (PMID: 23324856)
Cirocchi R, Rezongar A, Sapienza P, Crocetti D, Cavaliere D, Solaini L, Ercolani G, Sterpetti AV, Mingoli A, Fiori E (2021) Current status of the self-expandable metal stent as a bridge to surgery versus emergency surgery in colorectal cancer: results from an updated systematic review and meta-analysis of the literature. Medicina (Kaunas) 57(3):268. https://doi.org/10.3390/medicina57030268.PMID:33804232;PMCID:PMC7998540
Balciscueta I, Balciscueta Z, Uribe N, García-Granero E (2020) Long-term outcomes of stent-related perforation in malignant colon obstruction: a systematic review and meta-analysis. Int J Colorectal Dis 35(8):1439–1451. https://doi.org/10.1007/s00384-020-03664-1 (Epub 2020 Jun 22 PMID: 32572603)
Van Hooft JE, van Halsema EE, Vanbiervliet G, Beets-Tan RG RG, DeWitt JM, Donnellan F, Dumonceau JM, Glynne-Jones RG, Hassan C, Jiménez-Perez J, Meisner S, Muthusamy VR, Parker MC, Regimbeau JM, Sabbagh C, Sagar J, Tanis PJ PJ, Vandervoort J, Webster GJ, Manes G, Barthet MA, Repici A, European Society of Gastrointestinal Endoscopy (2014) Self-expandable metal stents for obstructing colonic and extracolonic cancer: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy 46(11):990–1053. https://doi.org/10.1055/s-0034-1390700 (Epub 2014 Oct 17 PMID: 25325682)
Van Hooft JE, Veld JV, Arnold D, Beets-Tan RGH, Everett S, Götz M, van Halsema EE, Hill J, Manes G, Meisner S, Rodrigues-Pinto E, Sabbagh C, Vandervoort J, Tanis PJ, Vanbiervliet G, Arezzo A (2020) Self-expandable metal stents for obstructing colonic and extracolonic cancer: European Society of Gastrointestinal Endoscopy (ESGE) Guideline - Update 2020. Endoscopy 52(5):389–407. https://doi.org/10.1055/a-1140-3017 (Epub 2020 Apr 7 PMID: 32259849)
Ribeiro IB, Bernardo WM, Martins BDC, de Moura DTH, Baba ER, Josino IR, Miyahima NT, Coronel Cordero MA, Visconti TAC, Ide E, Sakai P, de Moura EGH (2018) Colonic stent versus emergency surgery as treatment of malignant colonic obstruction in the palliative setting: a systematic review and meta-analysis. Endosc Int Open 6(5):E558-E567. https://doi.org/10.1055/a-0591-2883. Epub 2018 May 8. Erratum in: Endosc Int Open. 2018 May;6(5):C1. PMID: 29756013; PMCID: PMC5943694
Zhao XD, Cai BB, Cao RS, Shi RH (2013) Palliative treatment for incurable malignant colorectal obstructions: a meta-analysis. World J Gastroenterol 19(33):5565–5574. https://doi.org/10.3748/wjg.v19.i33.5565.PMID:24023502;PMCID:PMC3761112
Frago R, Kreisler E, Biondo S, Salazar R, Dominguez J, Escalante E (2010) Outcomes in the management of obstructive unresectable stage IV colorectal cancer. Eur J Surg Oncol 36(12):1187–1194. https://doi.org/10.1016/j.ejso.2010.09.005 (PMID: 20864304)
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Recuenco, C.B., Septiem, J.G., Díaz, J.A. et al. Effect of self-expandable metal stent on morbidity and mortality and oncological prognosis in malignant colonic obstruction: retrospective analysis of its use as curative and palliative treatment. Int J Colorectal Dis 37, 475–484 (2022). https://doi.org/10.1007/s00384-021-04081-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-021-04081-8