Abstract
Background
Colorectal cancer (CRC) is the third most common diagnosed cancer and the third leading cause of all cancer deaths in the USA. Some evidences are shown that aspirin can reduce the morbidity and mortality of different cancers, including CRC. Aspirin has become a new focus of cancer prevention and treatment research so far; clinical studies, however, found conflicting conclusions of its anti-cancer characteristics. This study is to summarize the latest evidence of correlation between aspirin use and CRC and/or colorectal adenomas.
Methods
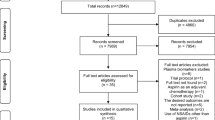
Databases were searched to identify randomized controlled trials (RCTs) in the salvage setting. The pooled relative risk (RR) with 95% confidence interval (CI) was used to estimate the effect of aspirin on colorectal cancer and/or colorectal adenomas. Subgroup analysis and sensitivity analysis were also conducted.
Results
The result showed that aspirin use was not associated with incidence of CRC (RR 0.97; 95% CI 0.84–1.12; P = 0.66; I2 = 34%), aspirin use was found to be associated with reduced recurrence of colorectal adenomas (RR 0.83; 95% CI 0.72–0.95; P = 0.006; I2 = 63%) and reduced mortality of CRC (RR 0.79; 95% CI 0.64–0.97; P = 0.02; I2 = 14%). Subgroup analysis found a statistically significant association in low dose with a pooled RR of 0.85 (95% CI 0.74–0.99; P = 0.03; I2 = 31%).
Conclusions
This meta-analysis of randomized controlled trial data indicates that aspirin reduces the overall risk of recurrence and mortality of CRC and/or colorectal adenomas. Incidence of CRC was also reduced with low-dose aspirin. The emerging evidence on aspirin’s cancer protection role highlights an exciting time for cancer prevention through low-cost interventions.
Trial registration
Clinicaltrials.gov no: CRD42020208852; August 18, 2020; https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42020208852).



Similar content being viewed by others
References
Siegel RL, Miller KD, Jemal A (2018) Cancer statistics, 2018. CA Cancer J Clin 68(1):7–30. https://doi.org/10.3322/caac.21442
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68(6):394–424. https://doi.org/10.3322/caac.21492
Baron JA (2003) Epidemiology of non-steroidal anti-inflammatory drugs and cancer. Prog Exp Tumor Res 37:1–24. https://doi.org/10.1159/000071364
Flossmann E, Rothwell PM, British Doctors Aspirin Trial and the UK-TIA Aspirin Trial (2007) Effect of aspirin on long-term risk of colorectal cancer: consistent evidence from randomised and observational studies. Lancet 369(9573):1603–1613. https://doi.org/10.1016/S0140-6736(07)60747-8
Bibbins-Domingo K, U.S. Preventive Services Task Force (2016) Aspirin use for the primary prevention of cardiovascular disease and colorectal cancer: U.S. Preventive Services Task Force Recommendation Statement. Ann Intern Med 164(12):836–845. https://doi.org/10.7326/M16-0577
Cardwell CR, Kunzmann AT, Cantwell MM et al (2014) Low-dose aspirin use after diagnosis of colorectal cancer does not increase survival: a case-control analysis of a population-based cohort. Gastroenterology 146(3):700–708.e2. https://doi.org/10.1053/j.gastro.2013.11.005
Steering Committee of the Physicians’ Health Study Research Group (1989) Final report on the aspirin component of the ongoing Physicians’ Health Study. N Engl J Med 321(3):129–135. https://doi.org/10.1056/NEJM198907203210301
Pommergaard HC, Burcharth J, Rosenberg J et al (2016) Aspirin, calcitriol, and calcium do not prevent adenoma recurrence in a randomized controlled trial. Gastroenterology 150(1):114–122.e4. https://doi.org/10.1053/j.gastro.2015.09.010
Rothwell PM, Wilson M, Elwin CE, Norrving B, Algra A, Warlow CP, Meade TW (2010) Long-term effect of aspirin on colorectal cancer incidence and mortality: 20-year follow-up of five randomised trials. Lancet 376(9754):1741–1750. https://doi.org/10.1016/S0140-6736(10)61543-7
Chan AT, Giovannucci EL, Schernhammer ES, Colditz GA, Hunter DJ, Willett WC, Fuchs CS (2004) A prospective study of aspirin use and the risk for colorectal adenoma. Ann Intern Med 140(3):157–166. https://doi.org/10.7326/0003-4819-140-3-200402030-00006
Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 339:b2535. https://doi.org/10.1136/bmj.b2535
Higgins JP, Altman DG, Gøtzsche PC et al (2011) The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 343:d5928. https://doi.org/10.1136/bmj.d5928
Higgins JPT, Green S [webpage on the Internet]. Cochrane handbook for systematic reviews of interventions version 5.1.0 [Updated March 2011]. The Cochrane Collaboration; 2011. Available from: http:// handbook.cochrane.org/. Accessed December 15, 2016.
Dubé C, Rostom A, Lewin G, Tsertsvadze A, Barrowman N, Code C, Sampson M, Moher D, U.S. Preventive Services Task Force (2007) The use of aspirin for primary prevention of colorectal cancer: a systematic review prepared for the U.S. Preventive Services Task Force. Ann Intern Med 146(5):365–375. https://doi.org/10.7326/0003-4819-146-5-200703060-00009
Stare J, Maucort-Boulch D (2016) Odds ratio, hazard ratio and relative risk. Metodoloski Zvezki 13(1):59–67
A glossary of EBM terms. BMJ Best Practice https://bestpractice.bmj.com/info/us/toolkit/ebm-tools/a-glossary-of-ebm-terms/. Accessed 24 Aug 2020
Ronksley PE, Brien SE, Turner BJ, Mukamal KJ, Ghali WA (2011) Association of alcohol consumption with selected cardiovascular disease outcomes: a systematic review and meta-analysis. BMJ 342:479. https://doi.org/10.1136/bmj.d671
Zhang JYK (1998) What’s the relative risk ? A method of correcting the odds ratio in cohort studies of common outcomes. JAMA 280:1690–1691. https://doi.org/10.1001/jama.280.19.1690
Tufanaru C, Munn Z, Stephenson M, Aromataris E (2015) Fixed or random effects meta-analysis? Common methodological issues in systematic reviews of effectiveness. Int J Evid Based Healthc 13(3):196–207. https://doi.org/10.1097/XEB.0000000000000065
Haidich AB (2010) Meta-analysis in medical research. Hippokratia 14(Suppl 1):29–37
Egger M, Davey Smith G, Schneider M et al (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ 315(7109):629–634. https://doi.org/10.1136/bmj.315.7109.629
Sandler RS, Halabi S, Baron JA, Budinger S, Paskett E, Keresztes R, Petrelli N, Pipas JM, Karp DD, Loprinzi CL, Steinbach G, Schilsky R (2003) A randomized trial of aspirin to prevent colorectal adenomas in patients with previous colorectal cancer. N Engl J Med 348(10):883–890. https://doi.org/10.1056/NEJMoa021633
Baron JA, Cole BF, Sandler RS, Haile RW, Ahnen D, Bresalier R, McKeown-Eyssen G, Summers RW, Rothstein R, Burke CA, Snover DC, Church TR, Allen JI, Beach M, Beck GJ, Bond JH, Byers T, Greenberg ER, Mandel JS, Marcon N, Mott LA, Pearson L, Saibil F, van Stolk RU (2003) A randomized trial of aspirin to prevent colorectal adenomas. N Engl J Med 348(10):891–899. https://doi.org/10.1056/NEJMoa021735
Ishikawa H, Mutoh M, Suzuki S, Tokudome S, Saida Y, Abe T, Okamura S, Tajika M, Joh T, Tanaka S, Kudo SE, Matsuda T, Iimuro M, Yukawa T, Takayama T, Sato Y, Lee K, Kitamura S, Mizuno M, Sano Y, Gondo N, Sugimoto K, Kusunoki M, Goto C, Matsuura N, Sakai T, Wakabayashi K (2014) The preventive effects of low-dose enteric-coated aspirin tablets on the development of colorectal tumours in Asian patients: a randomised trial. Gut 63(11):1755–1759. https://doi.org/10.1136/gutjnl-2013-305827
Benamouzig R, Uzzan B, Deyra J, Martin A, Girard B, Little J, Chaussade S, for the Association pour la Prévention par l'Aspirine du Cancer Colorectal Study Group (APACC)* (2012) Prevention by daily soluble aspirin of colorectal adenoma recurrence: 4-year results of the APACC randomised trial. Gut 61(2):255–261. https://doi.org/10.1136/gutjnl-2011-300113
Logan RF, Grainge MJ, Shepherd VC, Armitage NC, Muir KR, ukCAP Trial Group (2008) Aspirin and folic acid for the prevention of recurrent colorectal adenomas. Gastroenterology 134(1):29–38. https://doi.org/10.1053/j.gastro.2007.10.014
Benamouzig R, Deyra J, Martin A, Girard B, Jullian E, Piednoir B, Couturier D, Coste T, Little J, Chaussade S (2003) Daily soluble aspirin and prevention of colorectal adenoma recurrence: one-year results of the APACC trial. Gastroenterology 125(2):328–336. https://doi.org/10.1016/s0016-5085(03)00887-4
Hull MA, Sprange K, Hepburn T, Tan W, Shafayat A, Rees CJ, Clifford G, Logan RF, Loadman PM, Williams EA, Whitham D, Montgomery AA, seAFOod Collaborative Group (2018) Eicosapentaenoic acid and aspirin, alone and in combination, for the prevention of colorectal adenomas (seAFOod Polyp Prevention trial): a multicentre, randomised, double-blind, placebo-controlled, 2 × 2 factorial trial. Lancet 392(10164):2583–2594. https://doi.org/10.1016/S0140-6736(18)31775-6
Moayyedi P, Eikelboom JW, Bosch J et al (2019) Pantoprazole to prevent gastroduodenal events in patients receiving rivaroxaban and/or aspirin in a randomized, double-blind, placebo-controlled trial. Gastroenterology 157(2):403–412.e5. https://doi.org/10.1053/j.gastro.2019.04.041
Farrell B, Godwin J, Richards S, Warlow C (1991) The United Kingdom transient ischaemic attack (UK-TIA) aspirin trial: final results. J Neurol Neurosurg Psychiatry 54(12):1044–1054. https://doi.org/10.1136/jnnp.54.12.1044
Peto R, Gray R, Collins R, Wheatley K, Hennekens C, Jamrozik K, Warlow C, Hafner B, Thompson E, Norton S, Gilliland J, Doll R (1988) Randomised trial of prophylactic daily aspirin in British male doctors. Br Med J (Clin Res Ed) 296(6618):313–316. https://doi.org/10.1136/bmj.296.6618.313
The SALT Collaborative Group (1991) Swedish Aspirin Low-Dose Trial (SALT) of 75 mg aspirin as secondary prophylaxis after cerebrovascular ischaemic events. Lancet 338(8779):1345–1349
The Medical Research Council’s General Practice Research Framework (1998) Thrombosis prevention trial: randomised trial of low-intensity oral anticoagulation with warfarin and low-dose aspirin in the primary prevention of ischaemic heart disease in men at increased risk. Lancet 351(9098):233–241
Cook NR, Lee IM, Zhang SM, Moorthy MV, Buring JE (2013) Alternate-day, low-dose aspirin and cancer risk: long-term observational follow-up of a randomized trial. Ann Intern Med 159(2):77–85. https://doi.org/10.7326/0003-4819-159-2-201307160-00002
Gann PH, Manson JE, Glynn RJ, Buring JE, Hennekens CH (1993) Low-dose aspirin and incidence of colorectal tumors in a randomized trial. J Natl Cancer Inst 85(15):1220–1224. https://doi.org/10.1093/jnci/85.15.1220
Stürmer T, Glynn RJ, Lee IM, Manson JE, Buring JE, Hennekens CH (1998) Aspirin use and colorectal cancer: post-trial follow-up data from the Physicians’ Health Study. Ann Intern Med 128(9):713–720. https://doi.org/10.7326/0003-4819-128-9-199805010-00003
Yokoyama K, Ishizuka N, Uemura N, Mizokami Y, Hiraishi H, Murata M, Uchiyama S, Teramoto T, Shimada K, Yamazaki T, Oikawa S, Sugawara M, Ando K, Ikeda Y, the JPPP study group (2018) Effects of daily aspirin on cancer incidence and mortality in the elderly Japanese. Res Pract Thromb Haemost 2(2):274–281. https://doi.org/10.1002/rth2.12097
Boku S, Watanabe M, Sukeno M, Yaoi T, Hirota K, Iizuka-Ohashi M, Itoh K, Sakai T (2020) Deactivation of glutaminolysis sensitizes PIK3CA-mutated colorectal cancer cells to aspirin-induced growth inhibition. Cancers (Basel) 12(5):1097. https://doi.org/10.3390/cancers12051097
Rodríguez-Miguel A, García-Rodríguez LA, Gil M et al (2019) Clopidogrel and Low-Dose Aspirin, Alone or Together, Reduce Risk of Colorectal Cancer. Clin Gastroenterol Hepatol 17(10):2024–2033.e2. https://doi.org/10.1016/j.cgh.2018.12.012
Park SY, Wilkens LR, Kolonel LN, Monroe KR, Haiman CA, Marchand LL (2017) Exploring differences in the aspirin-colorectal cancer association by sex and race/ethnicity: the multiethnic cohort study. Cancer Epidemiol Biomark Prev 26(2):162–169. https://doi.org/10.1158/1055-9965.EPI-16-0560
Hankey GJ, Eikelboom JW (2006) Aspirin resistance. Lancet 367(9510):606–617. https://doi.org/10.1016/S0140-6736(06)68040-9
Mirkhel A, Peyster E, Sundeen J, Greene L, Michelson AD, Hasan A, Domanski M (2006) Frequency of aspirin resistance in a community hospital. Am J Cardiol 98(5):577–579. https://doi.org/10.1016/j.amjcard.2006.03.029
Levine PH (1973) An acute effect of cigarette smoking on platelet function. A possible link between smoking and arterial thrombosis. Circulation 48(3):619–623. https://doi.org/10.1161/01.cir.48.3.619
Norat T, Bingham S, Ferrari P, Slimani N, Jenab M, Mazuir M, Overvad K, Olsen A, Tjønneland A, Clavel F, Boutron-Ruault MC, Kesse E, Boeing H, Bergmann MM, Nieters A, Linseisen J, Trichopoulou A, Trichopoulos D, Tountas Y, Berrino F, Palli D, Panico S, Tumino R, Vineis P, Bueno-de-Mesquita HB, Peeters PHM, Engeset D, Lund E, Skeie G, Ardanaz E, González C, Navarro C, Quirós JR, Sanchez MJ, Berglund G, Mattisson I, Hallmans G, Palmqvist R, Day NE, Khaw KT, Key TJ, San Joaquin M, Hémon B, Saracci R, Kaaks R, Riboli E (2005) Meat, fish, and colorectal cancer risk: the European Prospective Investigation into cancer and nutrition. J Natl Cancer Inst 97(12):906–916. https://doi.org/10.1093/jnci/dji164
Devereaux PJ, Beattie WS, Choi PT et al (2005) How strong is the evidence for the use of perioperative beta blockers in non-cardiac surgery? Systematic review and meta-analysis of randomised controlled trials. BMJ 331(7512):313–321. https://doi.org/10.1136/bmj.38503.623646.8F
Bangalore S, Wetterslev J, Pranesh S, Sawhney S, Gluud C, Messerli FH (2008) Perioperative beta blockers in patients having non-cardiac surgery: a meta-analysis. Lancet 372(9654):1962–1976. https://doi.org/10.1016/S0140-6736(08)61560-3
Serebruany VL, Steinhubl SR, Berger PB, Malinin AI, Baggish JS, Bhatt DL, Topol EJ (2005) Analysis of risk of bleeding complications after different doses of aspirin in 192,036 patients enrolled in 31 randomized controlled trials. Am J Cardiol 95(10):1218–1222. https://doi.org/10.1016/j.amjcard.2005.01.049
Ying P, Sun N (2010) Correct understanding of the adverse reactions of aspirin and corresponding countermeasures [in Chinese]. Chin J Int Med 2010(11):915–917. https://doi.org/10.3760/cma.j.issn.0578-1426.2010.11.006
Khan SU, Khan MZ, Asad ZUA, Valavoor S, Khan MU, Khan MS, Krupica T, Alkhouli M, Kaluski E (2020) Efficacy and safety of low dose rivaroxaban in patients with coronary heart disease: a systematic review and meta-analysis. J Thromb Thrombolysis 50(4):913–920. https://doi.org/10.1007/s11239-020-02114-7
Patrono C, Ciabattoni G, Patrignani P, Pugliese F, Filabozzi P, Catella F, Davì G, Forni L (1985) Clinical pharmacology of platelet cyclooxygenase inhibition. Circulation 72(6):1177–1184. https://doi.org/10.1161/01.cir.72.6.1177
Taoxian Z, Weidong L, Guo Y et al (2012) One of the Meta-analysis series: types of meta-analysis [in Chinese]. Chin J Evid-Based Cardiovasc Med 4(01):3–5. https://doi.org/10.3969/j.issn.1674-4055.2012.01.002
Acknowledgements
We appreciate all authors for their contributions, and support from AMITA Health Saint Joseph Hospital Chicago and Anhui Medical University.
Availability of data and materials
All data generated or analyzed during this study was taken from published RCTs and are included in this published article (and its supplementary information files).
Author information
Authors and Affiliations
Contributions
Shaodi Ma and Dr. Chenyu Sun designed research; Shaodi Ma, Tiantian Han, and Huimei Zhang conducted literature search; Shaodi Ma, Guangbo Qu, and Dr. Chenyu Sun analyzed data; and Shaodi Ma and Dr. Chenyu Sun wrote the paper. Dr. Chenyu Sun, Dr. Ce Cheng, Dr. Chandur Bhan, and Dr. Qin Zhou provided critical opinion. Dr. Chenyu Sun, Dr. Ce Cheng, Hongru Yang, Zhichun Guo, Yue Yan, Chenyu Cao, Ziwei Ji, and Dr. Qin Zhou revised the paper. Shaodi Ma and Tiantian Han had primary responsibility for final content. Dr. Chenyu Sun is the corresponding author. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This article does not contain any studies with human participants or animals performed by any of the authors. We did not use individual data but published data. These data have been widely utilized in research and are generally available. Therefore, we confirm that any aspect of the work covered in this manuscript has been conducted with ethical approval. And this study has been registered (registration number: CRD42015025849) with the PROSPERO (International Prospective Register of Systematic Reviews) and was conducted according to the Preferred Reporting Items for Systemic Reviews and Meta-Analysis (PRISMA) statement.
Consent for publication
All individuals gave written informed consent for publication. The authors are responsible for the reported research, and have participated in the concept and design, analysis and interpretation of data, drafting or revising of the manuscript, and have approved the manuscript as submitted.
Conflict of interest
The authors declare that there are no conflicts of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(PDF 500 kb)
Rights and permissions
About this article
Cite this article
Ma, S., Han, T., Sun, C. et al. Does aspirin reduce the incidence, recurrence, and mortality of colorectal cancer? A meta-analysis of randomized clinical trials. Int J Colorectal Dis 36, 1653–1666 (2021). https://doi.org/10.1007/s00384-021-03889-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-021-03889-8