Abstract
Purpose
The study examined whether urgency of surgical intervention affects postoperative outcomes in patients with Crohn’s disease (CD) undergoing bowel resection.
Method
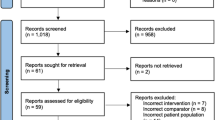
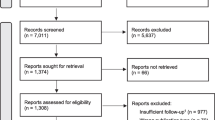
The review was conducted according to a predefined, published study protocol in Prospero which is an international database of prospectively registered systematic reviews in health. The study reported according to PRIMSMA guidelines. We searched Embase and Pubmed for articles reporting postoperative outcome after urgent and elective surgery in patients with CD undergoing bowel resection. Primary outcome variable was 30-day overall postoperative complications while secondary outcome variables were intraabdominal septic complications (IASCs), mortality, reoperation, and readmission. Assessment of bias was performed using Newcastle-Ottawa score. Two authors independently extracted data on each study, patients, and outcome measures.
Results
The search identified 22 studies in which 955 patients underwent urgent surgeries while 6518 patients underwent elective surgeries. Based on the quality assessment, 19 studies were classified as having high risk of bias, one study as having a medium risk of bias and 2 studies as having low risk of bias (≥ 8 stars). Random-effect metaanalysis showed urgent surgery was associated with ~ 40% increase in overall complications compared to elective surgery (RR = 1.43, 95% CI [1.09; 1.87], p = 0.010). IASCs also increased in patients who had urgent surgery (RR = 1.44, 95% CI [1.08; 1.92], p = 0.013). No significant difference was shown in mortality and readmission rates.
Conclusion
Urgent bowel resection in patients with CD is associated with higher risk of overall postoperative complications and IASCs.





Similar content being viewed by others
References
Frolkis AD, Dykeman J, Negrón ME, Debruyn J, Jette N, Fiest KM et al (2013) Risk of surgery for inflammatory bowel diseases has decreased over time: a systematic review and meta-analysis of population-based studies. Gastroenterology. 145(5):996–1006
Taxonera C, Rodrigo L, Casellas F, Calvet X, Gómez-Camacho F, Ginard D, Castro M, Castro L, Ponce M, Martínez-Montiel P, Ricart E, Gisbert JP, Román ALS, Morales JM, Casado MÁ (2009) Infliximab maintenance therapy is associated with decreases in direct resource use in patients with luminal or fistulizing Crohnʼs disease. J Clin Gastroenterol 43(10):950–956
Ramadas AV, Gunesh S, Thomas GAO, Williams GT, Hawthorne AB (2010) Natural history of Crohn’s disease in a population-based cohort from Cardiff (1986-2003): a study of changes in medical treatment and surgical resection rates. Gut. 59(9):1200–1206
Schnitzler F, Fidder H, Ferrante M, Noman M, Arijs I, Van Assche G et al (2009) Long-term outcome of treatment with infliximab in 614 patients with Crohn’s disease: results from a single-centre cohort. Gut. 58(4):492–500
Cosnes J, Nion-Larmurier I, Beaugerie L, Afchain P, Tiret E, Gendre J-P (2005) Impact of the increasing use of immunosuppressants in Crohn’s disease on the need for intestinal surgery. Gut. 54(2):237–241
Lazarev M, Ullman T, Schraut WH, Kip KE, Saul M, Regueiro M (2010) Small bowel resection rates in Crohn’s disease and the indication for surgery over time: experience from a large tertiary care center. Inflamm Bowel Dis 16(5):830–835
Tzivanakis A, Singh JC, Guy RJ, Travis SPL, Mortensen NJ, George BD (2012) Influence of risk factors on the safety of ileocolic anastomosis in crohn’s disease surgery. Dis Colon Rectum 55:558–562
Riss S, Schuster I, Papay P, Mittlböck M, Stift A (2013) Repeat intestinal resections increase the risk of recurrence of Crohnʼs disease. Dis Colon Rectum 56(7):881–887
Moftah M, Nazour F, Cunningham M, Cahill RA (2014) Single port laparoscopic surgery for patients with complex and recurrent Crohn’s disease. J Crohn's Colitis 8(9):1055–1061
Freeman HJ (2014) Spontaneous free perforation of the small intestine in adults. World Journal of Gastroenterology 20:9990–9997
El-Hussuna A, Pinkney T, Zmora O, Frasson M, Bhangu A, Battersby N et al (2018) Risk factors for unfavourable postoperative outcome in patients with Crohn’s disease undergoing right hemicolectomy or ileocaecal resection. An international audit by ESCP and S-ECCO. Color Dis 20(3):219–227
Lorenz D, Lorenz U, Hagmüller E, Saeger HD (1993) Crohn disease: resection therapy over the course of two decades. Zentralbl Chir 118(3):127–133 discussion 133-4
Yamamoto T, Keighley MRB (1999) Long-term outcome of total colectomy and ileostomy for Crohn disease. Scand J Gastroenterol 34(3):280–286
Serradori T, Germain A, Scherrer ML, Ayav C, Perez M, Romain B et al (2013) The effect of immune therapy on surgical site infection following Crohn’s disease resection. Br J Surg 100(8):1089–1093
Morar PS, Hodgkinson JD, Thalayasingam S, Koysombat K, Purcell M, Hart AL, Warusavitarne J, Faiz O (2015) Determining predictors for intra-abdominal septic complications following ileocolonic resection for Crohn’s disease—considerations in pre-operative and peri-operative optimisation techniques to improve outcome. J Crohn's Colitis 9(6):483–491. https://doi.org/10.1093/ecco-jcc/jjv051
Lee J-S, Kim H-J, Cho H-M, Lee K-M, Kye B-H (2016) The importance of the Crohn’s disease activity index in surgery for small bowel Crohn’s disease. J Visc Surg 153(5):339–345
El-Hussuna A, Hadi S II, El-Hussuna A, Hadi S, Iesalnieks I, Laurberg S, Srensen HT et al (2016) No difference in postoperative outcome after acute surgery whether the patients presented for first time or are known with Crohn’s disease. Int J Surg Open 6:1–4
Panteleimonitis S, Ahmed J, Parker T, Qureshi T, Parvaiz A (2017) Laparoscopic resection for primary and recurrent Crohn’s disease: a case series of over 100 consecutive cases. Int J Surg 47:69–76
Aydinli HH, Aytac E, Remzi FH, Bernstein M, Grucela AL (2018) Factors associated with short-term morbidity in patients undergoing colon resection for Crohn’s disease. J Gastrointest Surg 22(8):1434–1441
Iesalnieks I, Spinelli A, Frasson M, Di Candido F, Scheef B, Horesh N et al (2018) Risk of postoperative morbidity in patients having bowel resection for colonic Crohn’s disease. Tech Coloproctol. 22(12):947–953
Yu CS, Jung SW, Lee JL, Lim SB, Park IJ, Yoon YS, Kim CW, Ynag SK, Ye BD, Park SH, Han M, Kim JC (2019) The influence of preoperative medications on postoperative complications in patients after intestinal surgery for Crohn’s disease. Inflamm Bowel Dis 25(9):1559–1568
Celentano V, O’Leary DP, Caiazzo A, Flashman KG, Sagias F, Conti J, Senapati A, Khan J (2019) Longer small bowel segments are resected in emergency surgery for ileocaecal Crohn’s disease with a higher ileostomy and complication rate. Tech Coloproctol 23(11):1085–1091
Colombel JF, Loftus EV, Tremaine WJ, Pemberton JH, Wolff BG, Young-Fadok T, Harmsen WS, Schleck CD, Sandborn WJ (2004) Early postoperative complications are not increased in patients with Crohn’s disease treated perioperatively with infliximab or immunosuppressive therapy. Am J Gastroenterol 99(5):878–883
Alves A, Panis Y, Bouhnik Y, Pocard M, Vicaut E, Valleur P (2007) Risk factors for intra-abdominal septic complications after a first ileocecal resection for Crohn’s disease: a multivariate analysis in 161 consecutive patients. Dis Colon Rectum 50(3):331–336
Iesalnieks I, Kilger A, Glaß H, Glass H, Müller-Wille R, Klebl F et al (2008) Intraabdominal septic complications following bowel resection for Crohn’s disease: detrimental influence on long-term outcome. Int J Color Dis 23(12):1167–1174
Kono T, Ashida T, Ebisawa Y, Chisato N, Okamoto K, Katsuno H, Maeda K, Fujiya M, Kohgo Y, Furukawa H (2011) A new antimesenteric functional end-to-end handsewn anastomosis: surgical prevention of anastomotic recurrence in Crohn’s disease. Dis Colon Rectum 54(5):586–592
Riss S, Bittermann C, Schwameis K, Kristo I, Mittlböck M, Herbst F, Stift A (2012) Determinants for postoperative complications after laparoscopic intestinal resection for Crohn’s disease. Surg Endosc 26(4):933–938
Shental O, Tulchinsky H, Greenberg R, Klausner JM, Avital S (2012) Positive histological inflammatory margins are associated with increased risk for intra-abdominal septic complications in patients undergoing ileocolic resection for crohn’s disease. Dis Colon Rectum 55(11):1125–1130
El-Hussuna A, Andersen J, Bisgaard T, Jess P, Henriksen M, Oehlenschlager J et al (2012) Biologic treatment or immunomodulation is not associated with postoperative anastomotic complications in abdominal surgery for Crohn’s disease. Scand J Gastroenterol 47(6):662–668
Kanazawa A, Yamana T, Okamoto K, Sahara R (2012) Risk factors for postoperative intra-abdominal septic complications after bowel resection in patients with Crohn’s disease. Dis Colon Rectum 55(9):957–962
Fumery M, Seksik P, Auzolle C, Munoz-Bongrand N, Gornet JM, Boschetti G, Cotte E, Buisson A, Dubois A, Pariente B, Zerbib P, Chafai N, Stefanescu C, Panis Y, Marteau P, Pautrat K, Sabbagh C, Filippi J, Chevrier M, Houze P, Jouven X, Treton X, Allez M; REMIND study group investigators (2017) Postoperative complications after Ileocecal resection in Crohn’s disease: a prospective study from the REMIND Group. Am J Gastroenterol 112(2):337–345. https://doi.org/10.1038/ajg.2016.541
Brouquet A, Maggiori L, Zerbib P, Lefevre JH, Denost Q, Germain A et al (2016) Anti-TNF therapy is associated with an increased risk of postoperative morbidity after surgery for ileocolonic Crohn disease: results of a prospective nationwide cohort. Ann Surg 267(2):221–228
Yamamoto T, Keighley MR (1999) Factors affecting the incidence of postoperative septic complications and recurrence after strictureplasty for jejunoileal Crohn’s disease. Am J Surg 178(3):240–245. https://doi.org/10.1016/s0002-9610(99)00165-8
Singh S, Al-darmaki A, Frolkis AD, Seow CH, Leung Y, Novak KL et al (2015) Postoperative mortality among patients with inflammatory bowel diseases: a systematic review and meta-analysis of population-based studies. Gastroenterology. 149(4):928–937
Law CCY, Sasidharan S, Rodrigues R, Nguyen DD, Sauk J, Garber J et al (2016) Impact of specialized inpatient IBD care on outcomes of IBD hospitalizations : a cohort study. Inflamm Bowel Dis 22(9):2149–2157
de Groof EJ, Carbonnel F, Buskens CJ, Bemelman WA (2014) Abdominal abscess in Crohn’s disease: multidisciplinary management. Dig Dis 32(s1):103–109
Bennett JL, Ha CY, Efron JE, Gearhart SL, Lazarev MG, Wick EC (2015) Optimizing perioperative Crohn’s disease management: role of coordinated medical and surgical care. World J Gastroenterol 21(4):1182–1188
El-Hussuna A, Iesalnieks I, Horesh N, Hadi S, Dreznik Y, Zmora O (2017) The effect of pre-operative optimization on post-operative outcome in Crohn’s disease resections. Int J Color Dis 32(1):49–56
Zangenberg MS, Horesh N, Kopylov U, El-Hussuna A (2017) Preoperative optimization of patients with inflammatory bowel disease undergoing gastrointestinal surgery: a systematic review. International Journal of Colorectal Disease 32:1663–1676
Buskens CJ, Bemelman WA (2019) The surgeon and inflammatory bowel disease. British Journal of Surgery 106:1118–1119
Ponsioen CY, de Groof EJ, Eshuis EJ, Gardenbroek TJ, Bossuyt PMM, Hart A, Warusavitarne J, Buskens CJ, van Bodegraven AA, Brink MA, Consten ECJ, van Wagensveld BA, Rijk MCM, Crolla RMPH, Noomen CG, Houdijk APJ, Mallant RC, Boom M, Marsman WA, Stockmann HB, Mol B, de Groof AJ, Stokkers PC, D'Haens GR, Bemelman WA, Bruin K, Maring J, van Ditzhuijsen T, Prins H, van den Brande J, Kingma P, van Geloven A, de Boer N, van der Peet D, Jansen J, Gerhards M, van der Woude J, Schouten R, Oldenburg B, van Hillegersberg R, West R, Mannaerts G, Spanier M, Spillenaar Bilgen EJ, Lieverse R, van der Zaag E, Depla A, van de Laar A, Bolwerk C, Brouwer H, Mahmmod N, Hazebroek E, Vecht J, Pierik R, Dijkstra G, Hofker S, Uiterwaal T, Eijsbouts Q, Oostenbrug L, Sosef M, Cahen D, van der Werff S, Marinelli A, Peters J, Cense H, Talstra N, Morar P (2017) Laparoscopic ileocaecal resection versus infliximab for terminal ileitis in Crohn’s disease: a randomised controlled, open-label, multicentre trial. Lancet Gastroenterol Hepatol 2(11):785–792
Haider AH, Obirieze A, Velopulos CG, Richard P, Latif A, Scott VK, Zogg CK, Haut ER, Efron DT, Cornwell EE III, MacKenzie EJ, Gaskin DJ (2015) Incremental cost of emergency versus elective surgery. Ann Surg 262(2):260–266
El-Hussuna A, Myrelid P, Holubar SD, Kotze PG, Mackenzie G, Pellino G et al (2019) Biological treatment and the potential risk of adverse postoperative outcome in patients with inflammatory bowel disease: an open-source expert panel review of the current literature and future perspectives. Crohn’s Colitis 360 1(3):1–14
Author information
Authors and Affiliations
Contributions
A.E, T.M., and L.S.U designed the study and developed the PRISMA protocol. S.L.R and A.E conducted statistical analysis. All authors participated in literature reviewing, analysis and interpretation of data, drafting the paper and revising the manuscript. AE is the guarantor of the study.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Udholm, L.S., Rasmussen, S.L., Madsbøll, T.K. et al. A systemic review and metaanalysis of postoperative outcomes in urgent and elective bowel resection in patients with Crohn’s disease. Int J Colorectal Dis 36, 253–263 (2021). https://doi.org/10.1007/s00384-020-03786-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-020-03786-6