Abstract
Background
Colon cancer is the second most common cause of cancer-related death and an important cause of morbidity. The natural history of carcinogenesis, via the adenoma-carcinoma sequence, permits screening, which reduces the relative risk of mortality by up to 16%. The efficacy of a screening programme is limited by the growth of interval colorectal cancers between screening examinations. Quantifying the rate of interval cancers and delineating contributing endoscopic factors are crucial to maximise the benefit of a screening program.
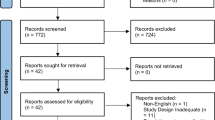
Methods
A systematic review was performed in accordance with PRISMA principles. Electronic databases were interrogated with a considered search strategy, and reference lists of retrieved papers were surveyed. For inclusion, studies included the rate of interval cancer (stated or calculated) and reported at least one of a predefined list of endoscopy characteristics. The primary outcome was to establish the rate of interval cancers. The secondary outcome was to determine the association between endoscopy quality measures and interval cancers.
Results
The search yielded 2067 papers. Seventy-six full text papers were reviewed. Fifteen papers met the inclusion criteria. In total, there were 117,793 colon cancers, 7281 of which were interval lesions, giving an overall rate of 6.2%. The adenoma detection rate (ADR) of the endoscopist performing the index operation was the most consistent endoscopy factor associated with development of interval cancers. The impact of setting, volume and bowel preparation varied between papers.
Conclusion
Interval cancers reduce the efficacy of colorectal screening programmes. Ensuring the quality of the endoscopy process, specifically by increasing the ADR of practitioners, is crucial to the reduction of the rate of interval cancers.



Similar content being viewed by others
References
Ito E, Yoshida M, Suzuki N, Imakita T, Tsutsui N, Ohdaira H, Kitajima M, Suzuki Y (2018) Prophylactic retention suture for surgical site infection: a retrospective cohort study. J Surg Res 221:58–63
Hewitson P, Glasziou P, Irwig L, Towler B, Watson E (2007) Screening for colorectal cancer using the faecal occult blood test, Hemoccult. Cochrane Database Syst Rev (1):Cd001216
Zauber AG, Winawer SJ, O'Brien MJ, Lansdorp-Vogelaar I, van Ballegooijen M, Hankey BF, Shi W, Bond JH, Schapiro M, Panish JF, Stewart ET, Waye JD (2012) Colonoscopic polypectomy and long-term prevention of colorectal-cancer deaths. N Engl J Med 366(8):687–696
Hewitson P, Glasziou P, Watson E, Towler B, Irwig L (2008) Cochrane systematic review of colorectal cancer screening using the fecal occult blood test (hemoccult): an update. Am J Gastroenterol 103(6):1541–1549
Sanduleanu S, le Clercq CM, Dekker E, Meijer GA, Rabeneck L, Rutter MD et al (2015) Definition and taxonomy of interval colorectal cancers: a proposal for standardising nomenclature. Gut 64(8):1257–1267
Singh S, Singh PP, Murad MH, Singh H, Samadder NJ (2014) Prevalence, risk factors, and outcomes of interval colorectal cancers: a systematic review and meta-analysis. Am J Gastroenterol 109(9):1375–1389
Adler J, Robertson DJ (2015) Interval colorectal Cancer after colonoscopy: exploring explanations and solutions. Am J Gastroenterol 110(12):1657–1664 quiz 65
van Rijn JC, Reitsma JB, Stoker J, Bossuyt PM, van Deventer SJ, Dekker E (2006) Polyp miss rate determined by tandem colonoscopy: a systematic review. Am J Gastroenterol 101(2):343–350
Rex DK, Cutler CS, Lemmel GT, Rahmani EY, Clark DW, Helper DJ, Lehman GA, Mark DG (1997) Colonoscopic miss rates of adenomas determined by back-to-back colonoscopies. Gastroenterology 112(1):24–28
Pohl H, Srivastava A, Bensen SP, Anderson P, Rothstein RI, Gordon SR et al (2013) Incomplete Polyp Resection During Colonoscopy—Results of the Complete Adenoma Resection (CARE) Study. Gastroenterology 144(1):74–80.e1
Govindarajan A, Rabeneck L, Yun L, Tinmouth J, Paszat LF, Baxter NN (2016) Population-based assessment of the outcomes in patients with postcolonoscopy colorectal cancers. Gut 65(6):971–976
Rees CJ, Thomas Gibson S, Rutter MD, Baragwanath P, Pullan R, Feeney M, Haslam N (2016) UK key performance indicators and quality assurance standards for colonoscopy. Gut 65(12):1923–1929
Rex DK, Boland CR, Dominitz JA, Giardiello FM, Johnson DA, Kaltenbach T, Levin TR, Lieberman D, Robertson DJ (2017) Colorectal Cancer screening: recommendations for physicians and patients from the U.S. multi-society task force on colorectal Cancer. Gastroenterology 153(1):307–323
Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6(7):e1000097
Stang A (2010) Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 25(9):603–605
Tsai CE, Wu KL, Chiu YC, Chuah SK, Tai WC, Hu ML, et al. (2018) The incidence and clinical associated factors of interval colorectal cancers in Southern Taiwan. J Formos Med Assoc 117(3):185–90
Gotfried J, Bernstein M, Ehrlich AC, Friedenberg FK (2015) Administrative database research overestimates the rate of interval Colon Cancer. J Clin Gastroenterol 49(6):483–490
Corley DA, Jensen CD, Marks AR, Zhao WK, Lee JK, Doubeni CA, Zauber AG, de Boer J, Fireman BH, Schottinger JE, Quinn VP, Ghai NR, Levin TR, Quesenberry CP (2014) Adenoma detection rate and risk of colorectal cancer and death. N Engl J Med 370(14):1298–1306
Bressler B, Paszat LF, Chen Z, Rothwell DM, Vinden C, Rabeneck L (2007) Rates of new or missed colorectal cancers after colonoscopy and their risk factors: a population-based analysis. Gastroenterology 132(1):96–102
Singh H, Nugent Z, Demers AA, Bernstein CN (2010) Rate and predictors of early/missed colorectal cancers after colonoscopy in Manitoba: a population-based study. Am J Gastroenterol 105(12):2588–2596
Cooper GS, Xu F, Barnholtz Sloan JS, Schluchter MD, Koroukian SM (2012) Prevalence and predictors of interval colorectal cancers in medicare beneficiaries. Cancer 118(12):3044–3052
Baxter NN, Sutradhar R, Forbes SS, Paszat LF, Saskin R, Rabeneck L (2011) Analysis of administrative data finds endoscopist quality measures associated with postcolonoscopy colorectal cancer. Gastroenterology 140(1):65–72
Haseman JH, Lemmel GT, Rahmani EY, Rex DK (1997) Failure of colonoscopy to detect colorectal cancer: evaluation of 47 cases in 20 hospitals. Gastrointest Endosc 45(6):451–455
Samadder NJ, Curtin K, Tuohy TM, Pappas L, Boucher K, Provenzale D et al (2014) Characteristics of missed or interval colorectal cancer and patient survival: a population-based study. Gastroenterology 146(4):950–960
Farrar WD, Sawhney MS, Nelson DB, Lederle FA, Bond JH (2006) Colorectal cancers found after a complete colonoscopy. Clin Gastroenterol Hepatol 4(10):1259–1264
Nayor J, Saltzman JR, Campbell EJ, Perencevich ML, Jajoo K, Richter JM (2017) Impact of physician compliance with colonoscopy surveillance guidelines on interval colorectal cancer. Gastrointest Endosc 85(6):1263–1270
Richter JM, Campbell EJ, Chung DC (2015) Interval colorectal cancer after colonoscopy. Clin Colorectal Cancer 14(1):46–51
le Clercq CM, Bouwens MW, Rondagh EJ, Bakker CM, Keulen ET, de Ridder RJ et al (2014) Postcolonoscopy colorectal cancers are preventable: a population-based study. Gut 63(6):957–963
Kaminski MF, Regula J, Kraszewska E, Polkowski M, Wojciechowska U, Didkowska J, Zwierko M, Rupinski M, Nowacki MP, Butruk E (2010) Quality indicators for colonoscopy and the risk of interval cancer. N Engl J Med 362(19):1795–1803
Shergill AK, Conners EE, McQuaid KR, Epstein S, Ryan JC, Shah JN et al (2015) Protective association of colonoscopy against proximal and distal colon cancer and patterns in interval cancer. Gastrointest Endosc 82(3):529–37.e1
Duarte RB, Bernardo WM, Sakai CM, Silva GL, Guedes HG, Kuga R et al (2018) Computed tomography colonography versus colonoscopy for the diagnosis of colorectal cancer: a systematic review and meta-analysis. Ther Clin Risk Manag 14:349–360
Garborg K, de Lange T, Bretthauer M (2017) Quality indicators in colonoscopy. Curr Treat Options Gastroenterol 15(3):416–428
Morris EJA, Rutter MD, Finan PJ, Thomas JD, Valori R (2015) Post-colonoscopy colorectal cancer (PCCRC) rates vary considerably depending on the method used to calculate them: a retrospective observational population-based study of PCCRC in the English National Health Service. Gut 64(8):1248–1256
Chen SC, Rex DK (2007) Endoscopist can be more powerful than age and male gender in predicting adenoma detection at colonoscopy. Am J Gastroenterol 102(4):856–861
Kaminski MF, Wieszczy P, Rupinski M, Wojciechowska U, Didkowska J, Kraszewska E, Kobiela J, Franczyk R, Rupinska M, Kocot B, Chaber-Ciopinska A, Pachlewski J, Polkowski M, Regula J (2017) Increased rate of adenoma detection associates with reduced risk of colorectal Cancer and death. Gastroenterology 153(1):98–105
Wieszczy P, Regula J, Kaminski MF (2017) Adenoma detection rate and risk of colorectal cancer. Best Pract Res Clin Gastroenterol 31(4):441–446
Denis B, Sauleau EA, Gendre I, Exbrayat C, Piette C, Dancourt V, Foll Y, Hadad HA, Bailly L, Perrin P (2014) The mean number of adenomas per procedure should become the gold standard to measure the neoplasia yield of colonoscopy: a population-based cohort study. Dig Liver Dis 46(2):176–181
Williams JE, Holub JL, Faigel DO (2012) Polypectomy rate is a valid quality measure for colonoscopy: results from a national endoscopy database. Gastrointest Endosc 75(3):576–582
Fedewa SA, Flanders WD, Ward KC, Lin CC, Jemal A, Goding Sauer A, Doubeni CA, Goodman M (2017) Racial and ethnic disparities in interval colorectal Cancer incidence: a population-based cohort study. Ann Intern Med 166(12):857–866
Sawhney MS, Farrar WD, Gudiseva S, Nelson DB, Lederle FA, Rector TS, Bond JH (2006) Microsatellite instability in interval Colon cancers. Gastroenterology 131(6):1700–1705
Parikh MP, Muthukuru S, Jobanputra Y, Naha K, Gupta NM, Wadhwa V et al (2017) Proximal sessile serrated adenomas are more prevalent in Caucasians, and gastroenterologists are better than nongastroenterologists at their detection. Gastroenterol Res Pract 2017:6710931
Shaukat A, Rector TS, Church TR, Lederle FA, Kim AS, Rank JM, Allen JI (2015) Longer withdrawal time is associated with a reduced incidence of interval Cancer after screening colonoscopy. Gastroenterology 149(4):952–957
Rex DK (2017) Polyp detection at colonoscopy: Endoscopist and technical factors. Best Pract Res Clin Gastroenterol 31(4):425–433
Rex DK (2000) Colonoscopic withdrawal technique is associated with adenoma miss rates. Gastrointest Endosc 51(1):33–36
Arain MA, Sawhney M, Sheikh S, Anway R, Thyagarajan B, Bond JH, Shaukat A (2010) CIMP status of interval colon cancers: another piece to the puzzle. Am J Gastroenterol 105(5):1189–1195
Shaukat A, Arain M, Anway R, Manaktala S, Pohlman L, Thyagarajan B (2012) Is KRAS mutation associated with interval colorectal cancers? Dig Dis Sci 57(4):913–917
Acknowledgements
Paul J Murphy, Information Specialist, RCSI Library.
Funding statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Appendix
Appendix
Rights and permissions
About this article
Cite this article
Nally, D.M., Ballester, A.W., Valentelyte, G. et al. The contribution of endoscopy quality measures to the development of interval colorectal cancers in the screening population: a systematic review. Int J Colorectal Dis 34, 123–140 (2019). https://doi.org/10.1007/s00384-018-3182-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-018-3182-8