Abstract
Purpose
Ileal pouch prolapse is a rare complication after j-pouch formation with an incidence of about 0.3%. However, if a pouch prolapse occurs, it can be a debilitating complication for the patient. Full-thickness pouch prolapse usually warrants surgical repair as reported by Sagar and Pemberton (Br J Surg 99(4):454–468, 2012) and Sherman et al. (Inflamm Bowel Dis 20(9):1678–1685, 2014). This report presents our first experience with laparoscopic ventral pouch pexy with acellular dermal matrix (ADM).
Methods
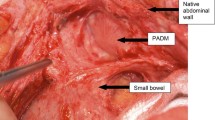
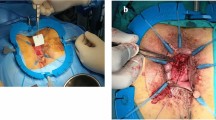
With the patient in the French position, four trocars were positioned: a camera port at the level of the umbilicus, two 5-mm trocars in the right lower quadrant, and a third 5-mm trocar in the left lower quadrant. The j-pouch was mobilized ventrally and laterally to the level of the sphincter. A 4 × 16-cm piece of ADM (EPIFLEX®, POLYTECH Health & Aesthetics, Dieburg, Germany) was sutured to the levators on both sides and to the ventral pouch directly cranial of the sphincter. In the next step, the ADM was attached to the promontory. Subsequently, further sutures were placed to attach the pouch to the ADM. Finally, the ADM was sewn to the cranial vaginal pole.
Results
Operating time was 249 min. The postoperative course was uneventful except for a higher stool frequency which could be managed conservatively. The patient was discharged on POD 9. At the latest follow-up (12 months after surgery), the patient was still symptom free without any sign of recurrence.
Conclusions
Laparoscopic ventral pouch pexy with ADM performed by a surgeon experienced in laparoscopic pouch surgery is a safe and effective treatment option in patients with pouch prolapse.






Similar content being viewed by others
References
Joyce MR, Fazio VW, Hull TT, Church J, Kiran RP, Mor I, Lian L, Shen B, Remzi FH (2010) Ileal pouch prolapse: prevalence, management, and outcomes. Journal of gastrointestinal surgery : official journal of the Society for Surgery of the Alimentary Tract 14(6):993–997. https://doi.org/10.1007/s11605-010-1194-y
Sagar PM, Pemberton JH (2012) Intraoperative, postoperative and reoperative problems with ileoanal pouches. Br J Surg 99(4):454–468. https://doi.org/10.1002/bjs.8697
Sherman J, Greenstein AJ, Greenstein AJ (2014) Ileal j pouch complications and surgical solutions: a review. Inflamm Bowel Dis 20(9):1678–1685. https://doi.org/10.1097/mib.0000000000000086
Changchien EM, Griffin JA, Murday ME, Bossart PW (2015) Mesh pouch pexy in the management of J-pouch prolapse. Dis Colon rectum 58(4):e46–e48. https://doi.org/10.1097/dcr.0000000000000337
Ehsan M, Isler JT, Kimmins MH, Billingham RP (2004) Prevalence and management of prolapse of the ileoanal pouch. Dis Colon rectum 47(6):885–888. https://doi.org/10.1007/s10350-004-0511-5
Funayama Y, Fukushima K, Shibata C, Takahashi K, Sasaki I (2005) Transabdominal repair of prolapsed pelvic ileal J-pouch after restorative proctocolectomy. Int J Color Dis 20(6):553–554. https://doi.org/10.1007/s00384-004-0687-0
Ragupathi M, Patel CB, Ramos-Valadez DI, Haas EM (2010) Robotic-assisted laparoscopic “salvage” rectopexy for recurrent ileoanal J-pouch prolapse. Gastroenterol Res Pract 2010:790462–790464. https://doi.org/10.1155/2010/790462
Williams NS, Giordano P, Dvorkin LS, Huang A, Scott SM (2004) Full-thickness pouch prolapse after restorative proctocolectomy: a potential future problem treated by the new technique of external pelvic neorectal suspension (the express procedure). Dis Colon Rectum 47(8):1415–1419
Yong FA, Tsoraides S (2015) Salvage of ileal pouch-anal anastomosis after recurrent prolapse. Int J Color Dis 30(3):433–434. https://doi.org/10.1007/s00384-014-2011-y
Author information
Authors and Affiliations
Contributions
Study conception and design: J. Hardt, P. Kienle; acquisition of data: J. Hardt, P. Kienle; Analysis and interpretation of data: J. Hardt, P. Kienle; writing manuscript: J. Hardt, P. Kienle. All authors gave final approval of the version to be published.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Hardt, J., Kienle, P. Laparoscopic ventral pouch pexy with acellular dermal matrix (ADM)—a novel technique for the treatment of full-thickness pouch prolapse after restorative proctocolectomy and j-pouch. Int J Colorectal Dis 33, 1643–1646 (2018). https://doi.org/10.1007/s00384-018-3135-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-018-3135-2