Abstract
Purpose
Enhanced recovery after surgery (ERAS) provides many benefits. However, important knowledge gaps with respect to specific components of enhanced recovery after surgery remain because of limited validation data. The aim of the study was to validate a mature ERAS protocol at a different hospital and in a similar population of patients.
Methods
This is a retrospective analysis of patients undergoing elective colorectal surgery from 2009 through 2016. Patients enrolled in ERAS are compared with those undergoing the standard of care. Patient demographic characteristics, length of stay, pain scores, and perioperative morbidity are described.
Results
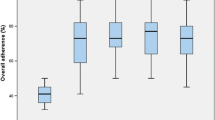
Patients (1396) were propensity matched into two equal groups (ERAS vs non-ERAS). No significant difference was observed for age, Charlson Comorbidity Index, American Society of Anesthesiologists score, body mass index, sex, operative approach, and surgery duration. Median length of stay in ERAS and non-ERAS groups was 3 and 5 days (P < .001). Mean pain scores were lower in the ERAS group, measured at discharge from the postanesthesia unit (P < .001), on postoperative day 1 (P = .002) and postoperative day 2 (P = .02) but were identical on discharge.
Conclusions
This ERAS protocol was validated in a similar patient population but at a different hospital. ERAS implementation was associated with an improved length of stay and pain scores similar to the original study. Different than most retrospective studies, propensity score matching ensured that groups were evenly matched. To our knowledge, this study is the only ERAS validation study in a propensity-matched cohort of patients undergoing elective colorectal surgery.



Similar content being viewed by others
References
Anderson AD, McNaught CE, MacFie J et al (2003) Randomized clinical trial of multimodal optimization and standard perioperative surgical care. Br J Surg 90(12):1497–1504
Basse L, Raskov HH, Hjort Jakobsen D, Sonne E, Billesbolle P, Hendel HW, Rosenberg J, Kehlet H (2002) Accelerated postoperative recovery programme after colonic resection improves physical performance, pulmonary function and body composition. Br J Surg 89(4):446–453
Kehlet H (1997) Multimodal approach to control postoperative pathophysiology and rehabilitation. Br J Anaesth 78(5):606–617
Moiniche S, Bulow S, Hesselfeldt P et al (1995) Convalescence and hospital stay after colonic surgery with balanced analgesia, early oral feeding, and enforced mobilisation. The Eur J Surg 161(4):283–288
Carmichael JC, Keller DS, Baldini G, Bordeianou L, Weiss E, Lee L, Boutros M, McClane J, Feldman LS, Steele SR (2017) Clinical practice guidelines for enhanced recovery after Colon and rectal surgery from the American Society of Colon and Rectal Surgeons and Society of American Gastrointestinal and Endoscopic Surgeons. Dis Colon Rectum 60(8):761–784
Delaney CP, Brady K, Woconish D, Parmar SP, Champagne BJ (2012) Towards optimizing perioperative colorectal care: outcomes for 1,000 consecutive laparoscopic colon procedures using enhanced recovery pathways. Am J Surg 203(3):353–355 discussion 5-6
Gustafsson UO, Hausel J, Thorell A, Ljungqvist O, Soop M, Nygren J, Enhanced Recovery After Surgery Study Group (2011) Adherence to the enhanced recovery after surgery protocol and outcomes after colorectal cancer surgery. Arch Surg 146(5):571–577
Larson DW, Lovely JK, Cima RR, Dozois EJ, Chua H, Wolff BG, Pemberton JH, Devine RR, Huebner M (2014) Outcomes after implementation of a multimodal standard care pathway for laparoscopic colorectal surgery. Br J Surg 101(8):1023–1030
Stephen AE, Berger DL (2003) Shortened length of stay and hospital cost reduction with implementation of an accelerated clinical care pathway after elective colon resection. Surgery 133(3):277–282
Lassen K, Soop M, Nygren J, Cox PB, Hendry PO, Spies C, von Meyenfeldt M, Fearon KC, Revhaug A, Norderval S, Ljungqvist O, Lobo DN, Dejong CH, Enhanced Recovery After Surgery (ERAS) Group (2009) Consensus review of optimal perioperative care in colorectal surgery: enhanced recovery after surgery (ERAS) group recommendations. Arch Surg 144(10):961–969
Kahokehr A, Sammour T, Zargar-Shoshtari K et al (2009) Implementation of ERAS and how to overcome the barriers. Int J Surg (London, England) 7(1):16–19
Ljungqvist O (2015) Sustainability after structured implementation of ERAS protocols. World J Surg 39(2):534–535
Song W, Wang K, Zhang RJ, Dai QX, Zou SB (2016) The enhanced recovery after surgery (ERAS) program in liver surgery: a meta-analysis of randomized controlled trials. Springerplus 5:207
Spanjersberg WR, Reurings J, Keus F, et al. 2011 Fast track surgery versus conventional recovery strategies for colorectal surgery. Cochrane Database Syst Rev. (2):Cd007635
Greco M, Capretti G, Beretta L, Gemma M, Pecorelli N, Braga M (2014) Enhanced recovery program in colorectal surgery: a meta-analysis of randomized controlled trials. World J Surg 38(6):1531–1541
Rawlinson A, Kang P, Evans J, Khanna A (2011) A systematic review of enhanced recovery protocols in colorectal surgery. Ann R Coll Surg Engl 93(8):583–588
Lovely JK, Maxson PM, Jacob AK, Cima RR, Horlocker TT, Hebl JR, Harmsen WS, Huebner M, Larson DW (2012) Case-matched series of enhanced versus standard recovery pathway in minimally invasive colorectal surgery. Br J Surg 99(1):120–126
Moriarty JP, Daniels PR, Manning DM, O’Meara JG, Ou NN, Berg TM, Haag JD, Roellinger DL, Naessens JM (2017) Going beyond administrative data: retrospective evaluation of an algorithm using the electronic health record to help identify bleeding events among hospitalized medical patients on warfarin. Am J Med Qual 32(4):391–396
Varadhan KK, Neal KR, Dejong CH et al (2010) The enhanced recovery after surgery (ERAS) pathway for patients undergoing major elective open colorectal surgery: a meta-analysis of randomized controlled trials. Clin Nutr (Edinburgh, Scotland) 29(4):434–440
Lv L, Shao YF, Zhou YB (2012) The enhanced recovery after surgery (ERAS) pathway for patients undergoing colorectal surgery: an update of meta-analysis of randomized controlled trials. Int J Color Dis 27(12):1549–1554
Wind J, Hofland J, Preckel B, Hollmann MW, Bossuyt PMM, Gouma DJ, van Berge Henegouwen MI, Fuhring JW, Dejong CHC, van Dam RM, Cuesta MA, Noordhuis A, de Jong D, van Zalingen E, Engel AF, Goei TH, de Stoppelaar IE, van Tets WF, van Wagensveld BA, Swart A, van den Elsen MJLJ, Gerhards MF, de Wit LT, Siepel MAM, van Geloven AAW, Juttmann JW, Clevers W, Bemelman WA (2006) Perioperative strategy in colonic surgery; laparoscopy and/or fast track multimodal management versus standard care (LAFA trial). BMC Surg 6:16
Wind J, Polle SW, Fung Kon Jin PH et al (2006) Systematic review of enhanced recovery programmes in colonic surgery. Br J Surg 93(7):800–809
Bond-Smith G, Belgaumkar AP, Davidson BR et al (2016) Enhanced recovery protocols for major upper gastrointestinal, liver and pancreatic surgery. Cochrane Database Syst Rev 2:Cd011382
Nicholson A, Lowe MC, Parker J, Lewis SR, Alderson P, Smith AF (2014) Systematic review and meta-analysis of enhanced recovery programmes in surgical patients. Br J Surg 101(3):172–188
Hendren S, Morris AM, Zhang W, Dimick J (2011) Early discharge and hospital readmission after colectomy for cancer. Dis Colon Rectum 54(11):1362–1367
Andersen J, Hjort-Jakobsen D, Christiansen PS, Kehlet H (2007) Readmission rates after a planned hospital stay of 2 versus 3 days in fast-track colonic surgery. Br J Surg 94(7):890–893
Bergquist JR, Thiels CA, Etzioni DA, Habermann EB, Cima RR (2016) Failure of colorectal surgical site infection predictive models applied to an independent dataset: do they add value or just confusion? J Am Coll Surg 222(4):431–438
Etzioni DA, Lessow CL, Lucas HD, Merchea A, Madura JA, Mahabir R, Mishra N, Wasif N, Mathur AK, Chang YHH, Cima RR, Habermann EB (2018) Infectious surgical complications are not dichotomous: characterizing discordance between administrative data and registry data. Ann Surg 267(1):81–87
Stone AB, Grant MC, Pio Roda C, Hobson D, Pawlik T, Wu CL, Wick EC (2016) Implementation costs of an enhanced recovery after surgery program in the United States: a financial model and sensitivity analysis based on experiences at a quaternary academic medical center. J Am Coll Surg 222(3):219–225
Nelson G, Kiyang LN, Crumley ET, Chuck A, Nguyen T, Faris P, Wasylak T, Basualdo-Hammond C, McKay S, Ljungqvist O, Gramlich LM (2016) Implementation of enhanced recovery after surgery (ERAS) across a provincial healthcare system: the ERAS Alberta colorectal surgery experience. World J Surg 40(5):1092–1103
Funding
Funding provided by Robert D. and Patricia E. Kern Center for Science of Health Care Delivery. The funder had no role in study design; in the collection, analysis, and interpretation of data; in the writing of the report; and in the decision to submit the article for publication.
Author information
Authors and Affiliations
Contributions
All authors made substantial contribution to the conception and design of the work, as well as the acquisition, analysis, and interpretation of data. All authors were critically involved in drafting and revising this project for important intellectual content. Final approval of the version to be published was given by all authors, and they agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
The Mayo Clinic Institutional Review Board approved this retrospective study. This study followed the reporting guidelines of the Strengthening the Reporting of Observational Studies in Epidemiology.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
This manuscript was presented as a “quick shot presentation” at the 13th annual Academic Surgical Congress, January 30-February 1, 2018, Jacksonville, Florida.
Rights and permissions
About this article
Cite this article
Lemini, R., Spaulding, A.C., Naessens, J.M. et al. ERAS protocol validation in a propensity-matched cohort of patients undergoing colorectal surgery. Int J Colorectal Dis 33, 1543–1550 (2018). https://doi.org/10.1007/s00384-018-3133-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-018-3133-4