Abstract
Purpose
Self-expandable metallic stents (SEMS) may be used in acute, obstructing, left-sided colorectal cancer (CRC) to avoid high-risk emergency surgery. However, the data regarding the long-term effects of SEMS as a bridge to surgery are limited and contradictory. Our aim is to analyze the long-term oncological outcomes of SEMS compared with surgery.
Methods
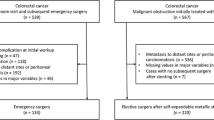
Between January 2006 and November 2013, a total of 855 patients with stage III CRC were regularly followed at the CRC clinic of Severance Hospital, Seoul, Korea. We retrospectively evaluated their 5-year disease-free survival (DFS), 5-year overall survival (OS), and 5-year cancer-specific survival (CSS).
Results
There were 94 patients in the SEMS group, 17 in the emergent-surgery group, and 744 in the elective-surgery group. In the short term, the rate of permanent stoma formation was significantly higher in the emergent-surgery group than in the SEMS group (p = 0.030), although the median hospital stay and overall complication rate were comparable. During the long-term follow-up period, oncological outcomes including 5-year DFS (70.2 vs 52.9%; p = 0.210), OS (70.2 vs 52.9%; p = 0.148), and CSS (79.8 vs 70.6%; p = 0.342) were not different between the SEMS group and the emergent-surgery group. Multivariate analysis showed emergent operation to be a significant risk factor of DFS (hazard ratio [HR], 3.117; 95% confidence interval [CI], 1.498–6.489; p = 0.002).
Conclusions
Preoperative SEMS insertion does not adversely affect long-term oncological outcomes or patient survival.

Similar content being viewed by others
References
Yoon M, Kim N, Nam B, Joo J, Ki M (2015) Changing trends in colorectal cancer in the Republic of Korea: contrast with Japan. Epidemiol Health 37:e2015038. https://doi.org/10.4178/epih/e2015038
Shin A, Kim KZ, Jung KW, Park S, Won YJ, Kim J, Kim DY, Oh JH (2012) Increasing trend of colorectal cancer incidence in Korea, 1999-2009. Cancer Res Treat 44(4):219–226. https://doi.org/10.4143/crt.2012.44.4.219
Fan YB, Cheng YS, Chen NW, Xu HM, Yang Z, Wang Y, Huang YY, Zheng Q (2006) Clinical application of self-expanding metallic stent in the management of acute left-sided colorectal malignant obstruction. World J Gastroenterol 12(5):755–759
Sjo OH, Larsen S, Lunde OC, Nesbakken A (2009) Short term outcome after emergency and elective surgery for colon cancer. Color Dis 11(7):733–739. https://doi.org/10.1111/j.1463-1318.2008.01613.x
McArdle CS, Hole DJ (2004) Emergency presentation of colorectal cancer is associated with poor 5-year survival. Br J Surg 91(5):605–609. https://doi.org/10.1002/bjs.4456
Saida Y, Sumiyama Y, Nagao J, Uramatsu M (2003) Long-term prognosis of preoperative “bridge to surgery” expandable metallic stent insertion for obstructive colorectal cancer: comparison with emergency operation. Dis Colon Rectum 46(10 Suppl):S44–S49. https://doi.org/10.1097/01.DCR.0000087483.63718.A2
Martinez-Santos C, Lobato RF, Fradejas JM, Pinto I, Ortega-Deballon P, Moreno-Azcoita M (2002) Self-expandable stent before elective surgery vs. emergency surgery for the treatment of malignant colorectal obstructions: comparison of primary anastomosis and morbidity rates. Dis Colon Rectum 45(3):401–406
Ng KC, Law WL, Lee YM, Choi HK, Seto CL, Ho JW (2006) Self-expanding metallic stent as a bridge to surgery versus emergency resection for obstructing left-sided colorectal cancer: a case-matched study. J Gastrointest Surg 10(6):798–803. https://doi.org/10.1016/j.gassur.2006.02.006
Jimenez-Perez J, Casellas J, Garcia-Cano J, Vandervoort J, Garcia-Escribano OR, Barcenilla J, Delgado AA, Goldberg P, Gonzalez-Huix F, Vazquez-Astray E, Meisner S (2011) Colonic stenting as a bridge to surgery in malignant large-bowel obstruction: a report from two large multinational registries. Am J Gastroenterol 106(12):2174–2180. https://doi.org/10.1038/ajg.2011.360
Arezzo A, Passera R, Lo Secco G, Verra M, Bonino MA, Targarona E, Morino M (2017) Stent as bridge to surgery for left-sided malignant colonic obstruction reduces adverse events and stoma rate compared with emergency surgery: results of a systematic review and meta-analysis of randomized controlled trials. Gastrointest Endosc 86:416–426. https://doi.org/10.1016/j.gie.2017.03.1542
Huang X, Lv B, Zhang S, Meng L (2014) Preoperative colonic stents versus emergency surgery for acute left-sided malignant colonic obstruction: a meta-analysis. J Gastrointest Surg 18(3):584–591. https://doi.org/10.1007/s11605-013-2344-9
Gorissen KJ, Tuynman JB, Fryer E, Wang L, Uberoi R, Jones OM, Cunningham C, Lindsey I (2013) Local recurrence after stenting for obstructing left-sided colonic cancer. Br J Surg 100(13):1805–1809. https://doi.org/10.1002/bjs.9297
Sabbagh C, Browet F, Diouf M, Cosse C, Brehant O, Bartoli E, Mauvais F, Chauffert B, Dupas JL, Nguyen-Khac E, Regimbeau JM (2013) Is stenting as “a bridge to surgery” an oncologically safe strategy for the management of acute, left-sided, malignant, colonic obstruction? A comparative study with a propensity score analysis. Ann Surg 258(1):107–115. https://doi.org/10.1097/SLA.0b013e31827e30ce
Sloothaak DA, van den Berg MW, Dijkgraaf MG, Fockens P, Tanis PJ, van Hooft JE, Bemelman WA, Collaborative Dutch Stent-In Study Group (2014) Oncological outcome of malignant colonic obstruction in the Dutch Stent-In 2 trial. Br J Surg 101(13):1751–1757. https://doi.org/10.1002/bjs.9645
Han SH, Lee JH (2014) Colonic stent-related complications and their management. Clin Endosc 47(5):415–419. https://doi.org/10.5946/ce.2014.47.5.415
van Hooft JE, van Halsema EE, Vanbiervliet G, Beets-Tan RG, DeWitt JM, Donnellan F, Dumonceau JM, Glynne-Jones RG, Hassan C, Jimenez-Perez J, Meisner S, Muthusamy VR, Parker MC, Regimbeau JM, Sabbagh C, Sagar J, Tanis PJ, Vandervoort J, Webster GJ, Manes G, Barthet MA, Repici A, European Society of Gastrointestinal E (2014) Self-expandable metal stents for obstructing colonic and extracolonic cancer: European Society of Gastrointestinal Endoscopy (ESGE) clinical guideline. Gastrointest Endosc 80(5):747–761 e741–775. https://doi.org/10.1016/j.gie.2014.09.018
Arezzo A, Balague C, Targarona E, Borghi F, Giraudo G, Ghezzo L, Arroyo A, Sola-Vera J, De Paolis P, Bossotti M, Bannone E, Forcignano E, Bonino MA, Passera R, Morino M (2016) Colonic stenting as a bridge to surgery versus emergency surgery for malignant colonic obstruction: results of a multicentre randomised controlled trial (ESCO trial). Surg Endosc 31:3297–3305. https://doi.org/10.1007/s00464-016-5362-3
Tung KL, Cheung HY, Ng LW, Chung CC, Li MK (2013) Endo-laparoscopic approach versus conventional open surgery in the treatment of obstructing left-sided colon cancer: long-term follow-up of a randomized trial. Asian J Endosc Surg 6(2):78–81. https://doi.org/10.1111/ases.12030
Matsuda A, Miyashita M, Matsumoto S, Matsutani T, Sakurazawa N, Takahashi G, Kishi T, Uchida E (2015) Comparison of long-term outcomes of colonic stent as “bridge to surgery” and emergency surgery for malignant large-bowel obstruction: a meta-analysis. Ann Surg Oncol 22(2):497–504. https://doi.org/10.1245/s10434-014-3997-7
Baron TH, Rey JF, Spinelli P (2002) Expandable metal stent placement for malignant colorectal obstruction. Endoscopy 34(10):823–830. https://doi.org/10.1055/s-2002-34271
Carraro PG, Segala M, Orlotti C, Tiberio G (1998) Outcome of large-bowel perforation in patients with colorectal cancer. Dis Colon Rectum 41(11):1421–1426
Marley AR, Nan H (2016) Epidemiology of colorectal cancer. Int J Mol Epidemiol Genet 7(3):105–114
Tejero E, Mainar A, Fernandez L, Tieso A, Cuezva JF, San Jose A (1995) New procedure for relief of malignant obstruction of the left colon. Br J Surg 82(1):34–35
Kim SJ, Kim HW, Park SB, Kang DH, Choi CW, Song BJ, Hong JB, Kim DJ, Park BS, Son GM (2015) Colonic perforation either during or after stent insertion as a bridge to surgery for malignant colorectal obstruction increases the risk of peritoneal seeding. Surg Endosc 29(12):3499–3506. https://doi.org/10.1007/s00464-015-4100-6
Erichsen R, Horvath-Puho E, Jacobsen JB, Nilsson T, Baron JA, Sorensen HT (2015) Long-term mortality and recurrence after colorectal cancer surgery with preoperative stenting: a Danish nationwide cohort study. Endoscopy 47(6):517–524. https://doi.org/10.1055/s-0034-1391333
Sabbagh C, Chatelain D, Trouillet N, Mauvais F, Bendjaballah S, Browet F, Regimbeau JM (2013) Does use of a metallic colon stent as a bridge to surgery modify the pathology data in patients with colonic obstruction? A case-matched study. Surg Endosc 27(10):3622–3631. https://doi.org/10.1007/s00464-013-2934-3
Kwak MS, Kim WS, Lee JM, Yang DH, Yoon YS, Yu CS, Kim JC, Byeon JS (2016) Does stenting as a bridge to surgery in left-sided colorectal cancer obstruction really worsen oncological outcomes? Dis Colon Rectum 59(8):725–732. https://doi.org/10.1097/dcr.0000000000000631
Alcantara M, Serra-Aracil X, Falco J, Mora L, Bombardo J, Navarro S (2011) Prospective, controlled, randomized study of intraoperative colonic lavage versus stent placement in obstructive left-sided colonic cancer. World J Surg 35(8):1904–1910. https://doi.org/10.1007/s00268-011-1139-y
Tan CJ, Dasari BV, Gardiner K (2012) Systematic review and meta-analysis of randomized clinical trials of self-expanding metallic stents as a bridge to surgery versus emergency surgery for malignant left-sided large bowel obstruction. Br J Surg 99(4):469–476. https://doi.org/10.1002/bjs.8689
Sagar J (2011) Colorectal stents for the management of malignant colonic obstructions. Cochrane Database Syst Rev 11:CD007378. https://doi.org/10.1002/14651858.CD007378.pub2
Sebastian S, Johnston S, Geoghegan T, Torreggiani W, Buckley M (2004) Pooled analysis of the efficacy and safety of self-expanding metal stenting in malignant colorectal obstruction. Am J Gastroenterol 99(10):2051–2057. https://doi.org/10.1111/j.1572-0241.2004.40017.x
Khot UP, Lang AW, Murali K, Parker MC (2002) Systematic review of the efficacy and safety of colorectal stents. Br J Surg 89(9):1096–1102. https://doi.org/10.1046/j.1365-2168.2002.02148.x
Acknowledgements
The authors thank native English-speaking experts from BioMed Proofreading® LLC for the editing.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Informed consent was obtained from all patients before the procedure. This study was approved by the institutional review board of Severance Hospital, Yonsei University (Seoul, Korea) and was conducted in accordance with the ethical principles of the Declaration of Helsinki
Electronic supplementary material
ESM 1
(DOCX 31 kb).
Rights and permissions
About this article
Cite this article
Park, J., Lee, H.J., Park, S.J. et al. Long-term outcomes after stenting as a bridge to surgery in patients with obstructing left-sided colorectal cancer. Int J Colorectal Dis 33, 799–807 (2018). https://doi.org/10.1007/s00384-018-3009-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-018-3009-7