Abstract
Purpose
The purpose of this study is to investigate the association of intake of nonsteroidal anti-inflammatory drugs (NSAIDs) and in particular nonaspirin NSAIDs and compare it with other risk factors for the progression of diverticulosis to diverticulitis in patients who underwent colonoscopy.
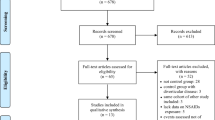
Methods
A total of 194 patients who underwent complete colonoscopy in our center between 2012 and 2016 were recruited: 144 with diverticulosis without prior diverticulitis (median age 71 years, 59.7% men) and 50 with diverticulitis (median age 64 years, 54.0% men). Data concerning current and previous medication as well as concomitant diseases were collected using a structured questionnaire and by revision of patients medical charts.
Results
Patients with diverticulitis were significantly (p < 0.001) younger as compared to individuals with plain diverticulosis (median age 64 versus 71 years, respectively). The intake of NSAIDs significantly (p = 0.002) increased the risk of prior diverticulitis (OR 3.2, 95% CI 1.5–6.9). In the multivariate model, both age (p < 0.001) and NSAIDs (p = 0.03) proved to be independent determinants of diverticulitis. When analyzing aspirin intake, it was not associated with diverticulitis.
Conclusions
Our study demonstrates, in line with previous reports, that intake of NSAIDs is associated with diverticulitis. We show in particular that nonaspirin NSAIDs might be selectively associated with diverticulitis. These results point to divergent role of aspirin and nonaspirin NSAIDs in the development of diverticulitis.


Similar content being viewed by others
References
Tursi A, Brandimarte G, MarioF D, Andreoli A, Annunziata ML, Astegiano M, Bianco MA, Buri L, Cammarota G, Capezzuto E, Chilovi F, Cianci M, Conigliaro R, del Favero G, di Cesare L, di Fonzo M, Elisei W, Faggiani R, Farroni F, Forti G, Germanà B, Giorgetti GM, Giovannone M, Lecca PG, Loperfido S, Marmo R, Morucci P, Occhigrossi G, Penna A, Rossi AF, Spadaccini A, Zampaletta C, Zilli M, Zullo A, Scarpignato C, Picchio M (2015) Development and validation of an endoscopic classification of diverticular disease of the colon: the DICA classification. Dig Dis 33(1):68–76. https://doi.org/10.1159/000366039
Hinchey EJ, Schaal PG, Richards GK (1978) Treatment of perforated diverticular disease of the colon. Adv Surg 12:85–109
Hansen O, Graupe F, Stock W (1998) Prognostic factors in perforating diverticulitis of the large intestine. Der Chirurg 69(4):443–449. https://doi.org/10.1007/s001040050436
Kruis W, Germer CT, Leifeld L (2014) Diverticular disease: guidelines of the german society for gastroenterology, digestive and metabolic diseases and the german society for general and visceral surgery. Digestion 90(3):190–207. https://doi.org/10.1159/000367625
Golder M, Ster IC, Babu P, Sharma A, Bayat M, Farah A (2011) Demographic determinants of risk, colon distribution and density scores of diverticular disease. World J Gastroenterol 17(8):1009–1017. https://doi.org/10.3748/wjg.v17.i8.1009
Everhart JE, Ruhl CE (2009) Burden of digestive diseases in the United States part II: lower gastrointestinal diseases. Gastroenterology 136(3):741–754. https://doi.org/10.1053/j.gastro.2009.01.015
Kang JY, Melville D, Maxwell JD (2004) Epidemiology and management of diverticular disease of the colon. Drugs Aging 21(4):211–228. https://doi.org/10.2165/00002512-200421040-00001
Sandler RS, Everhart JE, Donowitz M, Adams E, Cronin K, Goodman C, Gemmen E, Shah S, Avdic A, Rubin R (2002) The burden of selected digestive diseases in the United States. Gastroenterology 122(5):1500–1511. https://doi.org/10.1053/gast.2002.32978
Delvaux M (2003) Diverticular disease of the colon in Europe: epidemiology, impact on citizen health and prevention. Aliment Pharmacol Ther 18(Suppl 3):71–74. https://doi.org/10.1046/j.0953-0673.2003.01720.x
Crowe FL, Appleby PN, Allen NE, Key TJ (2011) Diet and risk of diverticular disease in Oxford cohort of European Prospective Investigation into Cancer and Nutrition (EPIC): prospective study of British vegetarians and non-vegetarians. BMJ 19:343:d4131. https://doi.org/10.1136/bmj.d4131
Hjern F, Wolk A, Hakansson N (2011) Smoking and the risk of diverticular disease in women. Br J Surg 98(7):997–1002. https://doi.org/10.1002/bjs.7477
Turunen P, Wikstrom H, Carpelan-Holmstrom M, Kairaluoma P, Kruuna O, Scheinin T (2010) Smoking increases the incidence of complicated diverticular disease of the sigmoid colon. Scand J Surg 99:14–17. https://doi.org/10.1177/145749691009900104
Usai P, Ibba I, Lai M, Boi MF, Savarese MF, Cuomo R, D’Alia G, Gemini S, Diaz G, Contu P (2011) Cigarette smoking and appendectomy: effect on clinical course of diverticulosis. Dig Liv Dis 43(2):98–101. https://doi.org/10.1016/j.dld.2010.05.008
Tonnesen H, Engholm G, Moller H (1999) Association between alcoholism and diverticulitis. Br J Surg 86(8):1067–1068. https://doi.org/10.1046/j.1365-2168.1999.01171.x
Aldoori WH, Giovannucci EL, Rimm EB, Wing AL, Trichopoulos DV, Willett WC (1995) A prospective study of alcohol, smoking, caffeine, and the risk of symptomatic diverticular disease in men. Ann Epidemiol 5(3):221–228. https://doi.org/10.1016/1047-2797(94)00109-7
Aldoori WH, Giovannucci EL, Rimm EB, Wing AL, Trichopoulos DV, Willett WC (1994) A prospective study of diet and the risk of symptomatic diverticular disease in men. Am J Clin Nutr 60(5):757–764. https://doi.org/10.1093/ajcn/60.5.757
Rosemar A, Angeras U, Rosengren A (2008) Body mass index and diverticular disease: a 28-year follow-up study in men. Dis Colon Rectum 51(4):450–455. https://doi.org/10.1007/s10350-007-9172-5
Strate LL, Liu YL, Aldoori WH, Syngal S, Giovannucci EL (2009) Obesity increases the risks of diverticulitis and diverticular bleeding. Gastroenterology 136(1):115. https://doi.org/10.1053/j.gastro.2008.09.025
Morris CR, Harvey IM, Stebbings WS, Speakman CT, Kennedy HJ, Hart AR (2003) Anti-inflammatory drugs, analgesics and the risk of perforated colonic diverticular disease. Br J Surg 90(10):1267–1272. https://doi.org/10.1002/bjs.4221
Morris CR, Harvey IM, Stebbings WS, Speakman CT, Kennedy HJ, Hart AR (2003) Do calcium channel blockers and antimuscarinics protect against perforated colonic diverticular disease? A case control study. Gut 52(12):1734–1737. https://doi.org/10.1136/gut.52.12.1734
Humes DJ, Fleming KM, Spiller RC, West J (2011) Concurrent drug use and the risk of perforated colonic diverticular disease: a population-based case-control study. Gut 60(2):219–224. https://doi.org/10.1136/gut.2010.217281
Strate LL, Liu YL, Huang ES, Giovannucci EL, Chan AT (2011) Use of aspirin or nonsteroidal anti-inflammatory drugs increases risk for diverticulitis and diverticular bleeding. Gastroenterology 140(5):1427–1433. https://doi.org/10.1053/j.gastro.2011.02.004
Kvasnovsky CL, Papagrigoriadis S, Bjarnason I (2014) Increased diverticular complications with nonsteriodal anti-inflammatory drugs and other medications: a systematic review and meta-analysis. Colorectal Dis 16(6):O189–O196. https://doi.org/10.1111/codi.12516
Hjern F, Mahmood MW, Abraham-Nordling M, Wolk A, Hakansson N (2015) Cohort study of corticosteroid use and risk of hospital admission for diverticular disease. Br J Surg 102(1):119–124. https://doi.org/10.1002/bjs.9686
Strate LL, Peery AF, Neumann I (2015) American Gastroenterological Association Institute technical review on the management of acute diverticulitis. Gastroenterology 149(7):1950–1976. https://doi.org/10.1053/j.gastro.2015.10.001
Agachan F, Chen T, Pfeifer J, Reissman P, Wexner SD (1996) A constipation scoring system to simplify evaluation and management of constipated patients. Dis Colon Rectum 39(6):681–685. https://doi.org/10.1007/BF02056950
Mpofu S, Mpofu CM, Hutchinson D, Maier AE, Dodd SR, Moots RJ (2004) Steroids, non-steroidal anti-inflammatory drugs, and sigmoid diverticular abscess perforation in rheumatic conditions. Ann Rheum Dis 63(5):588–590. https://doi.org/10.1136/ard.2003.010355
Campbell K, Steele RJ (1991) Non-steroidal anti-inflammatory drugs and complicated diverticular disease: a case-control study. Br J Surg 78(2):190–191. https://doi.org/10.1002/bjs.1800780218
Mathews SN, Lamm R, Yang J, Kang L, Telem D, Pryor AD, Talamini M, Genua J (2017) Factors associated with repeated health resource utilization in patients with diverticulitis. J Gastrointest Surg 21(1):112–120. https://doi.org/10.1007/s11605-016-3245-5
Okayama M, Hayashi S, Aoi Y, Nishio H, Kato S, Takeuchi K (2007) Aggravation by selective COX-1 and COX-2 inhibitors of dextran sulfate sodium (DSS)-induced colon lesions in rats. Dig Dis Sci 52(9):2095–2103. https://doi.org/10.1007/s10620-006-9597-z
Shahedi K, Fuller G, Bolus R, Cohen E, Vu M, Shah R, Agarwal N, Kaneshiro M, Atia M, Sheen V, Kurzbard N, van Oijen MGH, Yen L, Hodgkins P, Erder MH, Spiegel B (2013) Long-term risk of acute diverticulitis among patients with incidental diverticulosis found during colonoscopy. Clin Gastroenterol Hepatol 11(12):1609–1613. https://doi.org/10.1016/j.cgh.2013.06.020
Martel J, Raskin JB (2008) History, incidence, and epidemiology of diverticulosis. J Clin Gastroenterol 42(10):1125–1127. https://doi.org/10.1097/MCG.0b013e3181865f18
Chabok A, Pahlman L, Hjern F, Haapaniemi S, Smedh K (2012) Randomized clinical trial of antibiotics in acute uncomplicated diverticulitis. Br J Surg 99(4):532–539. https://doi.org/10.1002/bjs.8688
Funding
This study was supported by a grant from the Faculty of Medicine, Saarland University (HOMFOR grant T201000747), to Matthias C Reichert.
Author information
Authors and Affiliations
Contributions
MCR and MD designed the study; MCR, BA, FG, CJ, VZ, MC, and BF participated in acquisition of data; MCR collected the data and drafted the manuscript and together with FL, MK, and MD analyzed the data and finalized the manuscript, which was then critically revised by all authors. The final draft of the manuscript has been approved by all authors. The contents of this manuscript are our original work and have not been published, in whole or in part, prior to or simultaneous with our submission of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Terminology
The following definitions are used in this article, since they are not applied coherently in the literature: diverticulosis is the mere presence of colonic diverticula without evidence of inflammation. The term diverticular disease (DD) is used to summarize all possible impact on a patient’s health that could be caused by colonic diverticula, such as symptomatic diverticulosis, complicated and uncomplicated diverticulitis, as well as diverticular bleeding. Currently, no widely accepted classification for diverticulitis exists. Recently the DICA classification has been proposed [1]. The classification was not available at the initiation of our study and could therefore not be applied. Other commonly applied classifications include the predominantly in the USA used Hinchey classification, it could not be applied as it uses intraoperative findings [2], and the Hansen-Stock classification [3], which is used predominantly in Europe. The recent diverticulitis classification from the guidelines of the German Gastroenterological Association (DGVS) [4] is an extension of the Hansen-Stock classification. As our cohort included only patients treated in Germany and currently no other widely accepted suitable classification is available, diagnosis of diverticulosis and diverticulitis was based on these guidelines in this study.
Rights and permissions
About this article
Cite this article
Reichert, M.C., Krawczyk, M., Appenrodt, B. et al. Selective association of nonaspirin NSAIDs with risk of diverticulitis. Int J Colorectal Dis 33, 423–430 (2018). https://doi.org/10.1007/s00384-018-2968-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-018-2968-z