Abstract
Purpose
Faecal incontinence (FI) is a debilitating condition, which affects approximately 2–17 % of the population. Clinical assessment, physiological testing and imaging are usually used to evaluate the pathophysiology and guide management of FI. By analysing patient characteristics, symptoms and investigative findings, the aim of this study was to identify which patient characteristics and investigations influence patient management.
Methods
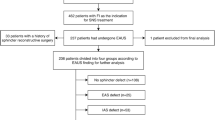
Data was prospectively collected for all patients with FI presenting to a single surgeon at the Royal Prince Alfred Hospital, Sydney, between March 2002 and September 2013. Continuous data was analysed using the independent T-test. Categorical data was analysed using chi-square tests and logistic regression.
Results
Three hundred ninety-eight patients were reviewed; 96 % were female and the mean age was 57 years. Surgical intervention was recommended for 185 patients (47 %) should biofeedback fail. Independent predictors for surgical recommendation were prolapse (p < 0.001, adjusted OR = 4.9 [CI 2.9–8.2]), a functional sphincter length <1 cm (p = 0.032, OR = 1.7 [CI 1.1–2.8]), an external anal sphincter defect (p = 0.028, OR = 1.8 [CI 1.1–3.1]) and a Cleveland Clinic Incontinence Score ≥10 (p = 0.029, OR = 1.7 [CI 1.1–2.6]).
Conclusion
Independent predictors of surgical recommendation included the presence of prolapse, a functional sphincter length <1 cm, an external anal sphincter defect and a Cleveland Clinic Incontinence Score ≥ 10. Pudendal neuropathy was not a predictor of surgical intervention, leading us to question the utility of this investigation.

Similar content being viewed by others
References
Rao SSC (2004) Diagnosis and management of fecal incontinence. Am J Gastroenterol 99:1585–1604
Barachi AE, Wald A, Rao SSC (2006) Debate: anorectal manometry and imaging are necessary in patients with fecal incontinence. Am J Gastroenterol 101(12):2679–2684
Liberman H et al (2001) A prospective evaluation of the value of anorectal physiology in the management of fecal incontinence. Dis Colon rectum 44(11):1567–1574
Wald A (2006) Anorectal manometry and imaging are not necessary in patients with fecal incontinence. Am J Gastroenterol 101(12):2681–2683
Ahmad M, McCallum IJD, Mercer-Jones M (2010) Management of faecal incontinence in adults. BMJ 340:1350–1355
(2007) Faecal incontinence in adults: management. National Institute for Health and Clinical Excellence. http://www.nice.org.uk/guidance/cg49.
Wald A (2007) Fecal incontinence in adults. N Engl J Med 356:1648–1655
Meyer I, Richter HE (2014) An evidence-based approach to the evaluation, diagnostic assessment and treatment of fecal incontinence in women. Curr Obstet Gynecol Rep 3(3):155–164
Pucciani F et al (2015) Diagnosis and treatment of faecal incontinence: consensus statement of the Italian Society of Colorectal Surgery and the Italian Association of Hosital Gastroenterologists. Dig Liver Dis. doi:10.1016/j.dld.2015.03.028
Ricciardi R et al (2006) The utility of pudendal nerve terminal motor latencies in idiopathic incontinence. Dis Colon rectum 49(6):852–857
Diamant NE et al (1999) American Gastroenterological Association technical review on anorectal testing techniques. Gastroenterology 116(3):735–760
Sangwan YP et al (1996) Unilateral pudendal neuropathy. Dis Colon rectum 39(6):686–689
Gilliland R et al (1998) Pudendal neuropathy is predictive of failure following anterior overlapping sphincteroplasty. Dis Colon rectum 41(12):1516–1522
Quezada Y et al (2015) Does preoperative anal physiology testing or ultrasonography predict clinical outcome with sacral neuromodulation for fecal incontinence? International Urogynaecology Journal
Roy A et al (2014) Predictive factors for successful sacral nerve stimulation in the treatment of fecal incontinence: lessons from a comprehensive treatment assessment. Dis Colon rectum 57:772–780
Brown SR, Wadhawan H, Nelson RL (2013) Surgery for faecal incontinence in adults. Cochrane Library 7
Zutshi M et al (2010) Anal physiology testing in fecal incontinence: is it of any value? Int J Color Dis 25(2):277–282
Heymen S et al (2009) Randomized, controlled trial shows biofeedback to be superior to alternative treatments for patients with faecal incontinence. Dis Colon rectum 52:1730–1737
Norton C, Kamm MA (2001) Anal sphincter biofeedback and pelvic floor exercises for faecal incontinence in adults—a systematic review. Aliment Pharmacol Ther 15:1147–1154
Pager CK et al (2002) Long-term outcomes of pelvic floor exerciseand biofeedback treatment for patients with fecal incontinence. Dis Colon rectum 45(8):997–1003
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval was obtained from the Sydney Local Health District Ethics Committee.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Podium presentation at the Asia Pacific Federation of Coloproctology Congress, Melbourne, Australia, 5th–7th October, 2015.
Poster presentation at the Royal Australian College of Surgeons Annual Scientific Congress, Perth, Australia, 4th to 8th May, 2015.
Rights and permissions
About this article
Cite this article
Cooper, E.A., De-Loyde, K.J., Young, C.J. et al. Pudendal nerve testing does not contribute to surgical decision making following anorectal testing in patients with faecal incontinence. Int J Colorectal Dis 31, 1437–1442 (2016). https://doi.org/10.1007/s00384-016-2617-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-016-2617-3