Abstract
Purpose
Pilonidal disease (PD) is marked by chronic inflammation and frequent recurrence which can decrease quality of life. However, debate remains regarding the optimal treatment for PD in the pediatric population. This study compares two recommended treatment approaches—excision with off-midline flap reconstruction (OMF: Bascom cleft lift flap, modified Limberg flap) and minimally invasive endoscopic pilonidal sinus treatment (EPSiT).
Methods
Single-center retrospective evaluation of patients 1–21 years of age with PD who underwent either excision with OMF reconstruction or EPSiT between 10/1/2011 and 10/31/2021. Outcomes included were disease recurrence, reoperation, and wound complication rates. Comparisons were performed using Chi-square and Mann–Whitney U tests.
Results
18 patients underwent excision/OMF reconstruction and 45 patients underwent EPSiT. The excision/OMF reconstruction cohort was predominantly male (44.4% vs 17.8% p = 0.028), with history of prior pilonidal infection (33.3% vs 6.7%; p = 0.006), and longer median operative time (60 min vs 17 min; p < 0.001). The excision/OMF reconstruction cohort had a higher rate of wound complications (22.2% vs 0%; p = 0.001), but lower rates of disease recurrence (5.6% vs 33.3%; p = 0.022) and reoperation (5.6% vs 31.1%; p = 0.031).
Conclusion
In pediatric patients with PD, excision with OMF reconstruction may decrease recurrence and reoperation rates with increased operative times and wound complication rates, compared to EPSiT.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pilonidal disease (PD), or pilonidal sinus disease, is an inflammatory disorder involving trapped hair or debris in the natal cleft [1]. PD is marked by chronic inflammation, sinus tract formation, secondary infection, and frequent recurrence [2]. In the United States, this affects 26 per 100,000 people with an increased frequency of occurrence in males and adolescents (14–25 years of age) [3, 4]. For adolescent patients with PD, the associated sequelae such as recurrent discharge or bleeding, pain, infection, abscess formation, and frequent healthcare encounters for treatment have been shown to significantly decrease quality of life and lead to increased absences from school or work [5, 6]. In rare cases, PD-related chronic inflammation can also increase the risk for squamous cell carcinoma formation in patients with compromised immune systems [7]. Thus, PD disproportionately affects the pediatric population and can have a significant impact on both physical and psychosocial wellbeing.
The primary goals of PD treatment are to excise all areas of disease, including undermining sinus tracts, while also minimizing post-operative pain, time away from baseline functional status, and the risk of wound complications (e.g., infection, dehiscence). Thus, the optimal treatment decreases the risk of recurrence and future reintervention, while also minimizing treatment-related morbidity. While prior studies have sought to determine the optimal treatment option, debate still remains regarding the most effective approach to achieving these goals [8,9,10]. Current treatment options include non-operative (e.g., hygiene/lifestyle modification, laser epilation), minimally invasive (e.g., sinusectomy/Gips procedure, endoscopic debridement), and excisional/reconstructive techniques (e.g., secondary healing, negative pressure wound therapy, midline primary closure, off-midline flap reconstruction) [11,12,13,14,15]. In recent years, minimally invasive treatment and excision with off-midline flap (OMF) reconstruction approaches have emerged as the recommended options due to favorable rates of achieving the aforementioned treatment goals [11, 16].
In the pediatric population, minimally invasive techniques are associated with lower rates of wound complications and a faster return to baseline functional status, but are limited by higher rates of disease recurrence and reoperation [11]. In contrast, excisional approaches with OMF reconstruction have demonstrated higher rates of wound complications and prolonged recovery time, with contradictory literature regarding long-term recurrence rates [11, 17]. In the adult population, excision combined with OMF reconstruction has been associated with decreased long-term recurrence rates [18]. This is attributed to the wide excision of diseased tissue and lateralization with flattening of the natal cleft achieved by OMF closure of the soft tissue defect [19,20,21].
In this context, prior studies have sought to compare excision with midline primary closure to minimally invasive techniques, or various off-midline flap reconstruction techniques to one another [8, 22,23,24,25,26]. However, in the pediatric population, little is known regarding direct comparison of minimally invasive endoscopic pilonidal sinus treatment (EPSiT) with excision and OMF reconstruction [11]. The objective of this study is to compare these two treatment approaches among pediatric patients with PD. We hypothesize that while excision and OMF reconstruction may lead to prolonged operative times and higher rates of wound complications, it may decrease PD recurrence and the need for reoperation—which suggests a more durable treatment option for the pediatric population.
Methods
Study design, patient population, and data elements
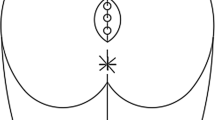
After Institutional Review Board approval was obtained (CHLA-21-00349), a single-center retrospective cohort study was performed. The study cohort included patients between 1 and 21 years of age who underwent surgery for PD between 10/1/2011 and 10/31/2021. Patients were identified using Current Procedural Terminology codes for pilonidal cyst excision (10,080–10081, 11,770–11772). Patients undergoing reoperation for recurrent disease or receiving management for an acute PD infection (e.g., incision and drainage, unroofing, antibiotics) were excluded. Only patients who underwent EPSiT or excision with OMF reconstruction (Bascom cleft lift flap, modified Limberg flap/MLF) were included in the analytic cohort. While prior studies in the adult population have suggested differing outcomes between these two OMF reconstruction approaches, validation in the pediatric population remains under investigation [27]. Thus, these two procedures were grouped together and compared directly to the MISTE approach. These procedures were performed as previously described [12, 20, 28,29,30] by multiple surgeons and procedure type was selected per surgeon preference. The EPSiT approach was performed by excising the draining sinus with a circular punch biopsy, followed by curette debridement and irrigation with a hydrogen peroxide-normal saline solution. A pediatric cystoscope was then used to inspect the sinus cavity and perform additional debridement with irrigation. In addition to operative management, non-operative management (e.g., hygiene modification, laser epilation) was also utilized for all patients per standard of care.
Data elements included patient characteristics (demographic, clinical) and clinical outcomes metrics. Patient demographic information included age, sex, and ethnicity. Clinical data included body mass index (kg/m2), comorbidities, history of pilonidal infection, operation type, total operative time, hospital length of stay, total narcotic use (in oral morphine equivalents), and the presence of post-operative complications. Follow-up data and post-operative outcomes were abstracted from the electronic health record and date of last follow-up was determined as the most recent evaluation by a surgical provider.
Outcomes
The primary outcome was disease recurrence which was defined as the presence of active PD > 28 days after the initial operation. Secondary outcomes included the need for reoperation or the presence of wound complications (dehiscence, infection).
Statistical analysis
Descriptive statistics were reported using frequency and proportions for categorical variables and median and ranges for continuous variables. Comparisons of categorical variables were performed using the Chi-square test, and the Mann–Whitney U test for continuous variables. Multivariate linear regression was performed to identify factors associated with disease recurrence. All analyses were conducted with two-sided significance and a significance cut-off level of 0.05. Analysis was performed using SPSS software v29.0.1.0 (IBM Corp., Armonk, New York, USA).
Results
Over the 10-year study period, a total of 63 patients met the inclusion criteria with 18 patients undergoing wide excision with OMF reconstruction (Bascom cleft lift flap n = 10, MLF n = 8) and 45 patients undergoing the EPSiT procedure. The overall cohort had a mean age of 15.5 years (SD = 1.6) with the youngest patient at 12 years and eldest patient at 18 years. The majority of patients were of Hispanic ethnicity (n = 44, 69.8%) with a male predominance in the excision/OMF reconstruction cohort (44.4% vs 17.8%, p = 0.028) (Table 1).
At median follow-up duration of 62 days, patients who underwent excision with OMF reconstruction experienced lower rates of recurrence (5.6% vs 33.3%, p = 0.022) and reoperation (5.6% vs 31.3%, p = 0.031) (Table 2). However, this cohort also had longer median operative times (60 min, range 35–97 min vs 17 min, range 6–68 min; p < 0.001) and wound dehiscence in four patients requiring wound care (Table 2). There was no difference in total post-operative narcotic use, time to recurrence, time to reoperation, or duration of follow-up (Table 2). Overall post-operative length of stay for all patients was ≤ 48 h with the majority of patients discharged within 24 h (n = 59, 93.7%) (Table 2). Four patients required admission for post-operative pain control, but were all discharged on post-operative day one.
Multivariate linear regression identified younger age and longer follow-up duration as factors associated with an increase in PD recurrence (Table 3). Univariate regression analysis also evaluated the relationship between PD recurrence and additional variables—sex, body mass index, comorbidity type, history of pilonidal infection, total operative time, and presence of wound complications—and none were found to be associated with PD recurrence.
Discussion
Treatment of PD in the pediatric population remains a challenge due to high rates of treatment-related morbidity and frequent recurrence resulting in repeated absences from school/work, decreased quality of life, and added psychosocial morbidity [5]. The breadth of treatment options alludes to the current lack of an optimal treatment modality to eradicate disease and mitigate morbidity. The observations from this comparative study highlight the benefits and limitations of two commonly utilized treatment options. While wide excision with OMF reconstruction demonstrated lower rates of recurrence and need for reoperation, the EPSiT approach required a shorter operative duration and exhibited a lower rate of wound complications. These findings reinforce similar outcomes from prior studies in the adult population and suggest that wide excision with OMF reconstruction is associated with increased early post-operative morbidity, but may provide a more durable treatment option for PD [24, 26].
In comparing the two operative modalities, excision with OMF reconstruction was associated with lower rates of disease recurrence and reoperation at a limited follow-up duration. Our observed recurrence rate after excision with OMF reconstruction was 5.6% which is consistent with previously reported rates ranging from 2.7 to 6.3% after excision with Limberg flap or MLF reconstruction [19, 20, 31]. We found this to be significantly lower than recurrence rates reported after minimally invasive treatment approaches, which have been previously reported at 13.2% at 5-year follow-up in the adult population and up to 38% at 28-month follow-up in the pediatric population [32, 33]. This may be accounted for by the larger area of excision and more complete eradication of the diseased tissue with the excisional approach. Thus, excision with OMF reconstruction may be more beneficial in recurrent or severe PD which may be incompletely excised by minimally invasive approaches [34, 35]. In addition, excision with OMF reconstruction provides a tension-free off-midline closure and flattens the natal cleft which may mitigate recurrence by decreasing skin maceration, bacterial growth, and hair ingrowth that can occur within a deep natal cleft. By decreasing disease recurrence with a more durable initial operation, we also observed lower rates of reoperation. Similar trends have also been observed in prior studies comparing minimally invasive techniques to excisional approaches [33]. While this adds to the existing data directly comparing minimally invasive treatment approaches with excision and OMF reconstruction in the pediatric population, a longitudinal multi-institutional study with long-term follow-up is needed to validate these findings.
Although patients experienced higher rates of recurrence and reoperation with the EPSiT procedure, they also had lower rates of wound complications compared to the excision/OMF reconstruction cohort. Due to the larger extent of excision and reconstruction with the latter approach, wound complications with excision and OMF reconstruction have been reported in up to 25% of pediatric patients with PD [17, 19, 21]. In the excision/OMF reconstruction cohort, we observed partial wound dehiscence in four patients (22.2%) which did not require reoperation, as well as no cases of wound infection, seroma, or hematoma formation. Two (50%) of these occurred in patients who underwent the Bascom cleft lift flap, and two (50%) of these occurred in patients who underwent the modified Limberg flap. In one patient, early unintentional drain removal led to acute wound dehiscence, while early return to athletic activity in another patient led to delayed wound dehiscence in a previously healed scar. While wound complications are a major limitation to excisional approaches, Limberg or MLF reconstruction have been previously reported as having the lowest relative risk of wound dehiscence when compared to alternative OMF reconstruction techniques [24]. Another major concern surrounding wound complications is the subsequent elevated risk of disease recurrence observed after wound dehiscence [36]. We did observe one case of recurrence after wound dehiscence in the excision/OMF reconstruction cohort, but despite this, the overall recurrence rate in this cohort remained low. Thus, while minimally invasive techniques decreased morbidity due to wound complications in the early post-operative period, it did not significantly alter recurrence rates compared to excision/OMF reconstruction approaches.
We also observed that the EPSiT procedure was able to be performed with a significantly shorter operative time compared to excision with OMF reconstruction. Prior experiences with excision and OMF reconstruction in the pediatric population have reported median operative times ranging from 67 to 92 min [19, 20], while shorter operative times up to 41 min have been reported with minimally invasive procedures [22]. Comparing these two operative techniques, the EPSiT approach was designed to be less extensive and less technically demanding compared to excisional/reconstructive techniques which explains the difference in operative duration [12, 37]. As a result, minimally invasive techniques also subsequently reduce anesthetic exposure, healthcare costs, and resource utilization [38]. However, as the EPSiT procedure requires a pediatric cystoscope and is often performed in the operating room in the pediatric population, additional research is needed to fully evaluate the long-term healthcare costs and utilization associated with disease recurrence and recurrent treatment in patients undergoing minimally invasive treatment.
It is important to note that while these findings demonstrate the benefits and limitations of both the EPSiT procedure and excision/OMF reconstruction, both options remain reasonable treatment options when compared to alternative excisional approaches. Although excision with primary midline closure can excise a larger area of diseased tissue and may shorten healing time compared to open healing by secondary intent, this approach is associated with elevated rates of wound complications (e.g., dehiscence, infection/abscess, seroma, hematoma) up to 65% and recurrence rates ranging from 21 to 37.5% [21, 23, 39, 40]. While excision with open healing by secondary intent or negative wound pressure therapy (NWPT) has been recommended to decrease rates of infectious wound complications, this approach is limited by prolonged healing times ranging from 62 days (NWPT) to three months (open wound packing) [41, 42]. In addition, NWPT requires frequent sponge/dressing changes and may lead to additional complications such as device malfunction or retained wound sponges that can further prolong healing time and increase treatment-related morbidity [42]. Thus, while the limitations of the minimally invasive treatment options and excision/OMF reconstruction are outlined in this study, alternative approaches to wound closure after excision (primary midline closure, NWPT, open wound packing) are not recommended [11, 43].
This comparative study has several limitations. Determination of disease recurrence may be limited by the short-term follow-up duration in this study. Although follow-up duration was similar between the two cohorts allowing for direct comparison of short-term disease recurrence, longer duration of follow-up has been shown to be directly associated with PD recurrence [24, 44, 45]. Thus, the follow-up duration in this study may not fully capture additional recurrences and long-term longitudinal monitoring would be prudent in validating these findings. In addition, although this study was performed at a freestanding children’s hospital which serves as a tertiary referral center in a large urban setting, follow-up data may be limited if patients utilized multiple centers for their care. Thus, this study is also vulnerable to the limitations associated with retrospective single-center studies. The retrospective nature of this study is also subject to selection bias and limits insight into treatment selection. As we observed that the entire patient population and the EPSiT cohort was predominantly female, which may be due to selection bias or a treatment approach preference by sex. As PD predominantly occurs in males, the majority of male patients may have been treated via an alternative approach (e.g., excision with midline primary closure or healing by secondary intent), and were, thus, excluded due to the objective of directly comparing two specific treatment approaches. Thus, a larger prospective randomized trial is needed to mitigate potential confounding which this study type is vulnerable to, as well as to further elucidate the optimal treatment method among patients of varying disease severity.
Conclusion
The treatment of pilonidal disease in the pediatric population remains challenging as exemplified by high rates of disease recurrence and reoperation. This study compares the two commonly used treatment approaches of excision with off-midline flap reconstruction and minimally invasive sinus tract excision. Compared to the EPSiT procedure, excision with off-midline flap reconstruction was associated with lower rates of recurrence and reoperation, but prolonged operative times and higher rates of wound dehiscence. Prospective randomized longitudinal data are vital in further evaluating the findings observed in this study.
Data availability
The datasets generated and/or analyzed are available from the corresponding author on reasonable request.
Abbreviations
- EPSiT:
-
Endoscopic pilonidal sinus treatment
- MLF:
-
Modified Limberg flap
- NWPT:
-
Negative pressure wound therapy
- OMF:
-
Off-midline flap
- PD:
-
Pilonidal disease
References
Karydakis GE (1992) Easy and successful treatment of pilonidal sinus after explanation of its causative process. Aust N Z J Surg 62:385–389
López JJ, Cooper JN, Halleran DR et al (2018) High rate of major morbidity after surgical excision for pilonidal disease. Surg Infect 19:603–607
Søndenaa K, Andersen E, Nesvik I et al (1995) Patient characteristics and symptoms in chronic pilonidal sinus disease. Int J Colorectal Dis 10:39–42
Lee PJ, Raniga S, Biyani DK et al (2008) Sacrococcygeal pilonidal disease. Colorectal Dis 10:639–650
Salimi-Jazi F, Abrajano C, Garza D et al (2022) Burden of pilonidal disease and improvement in quality of life after treatment in adolescents. Pediatr Surg Int 38:1453–1459
Henry OS, Farr BJ, Check NM et al (2021) A minimally invasive pilonidal protocol improves quality of life in adolescents. J Pediatr Surg 56:1861–1864
Malek MM, Emanuel PO, Divino CM (2007) Malignant degeneration of pilonidal disease in an immunosuppressed patient: report of a case and review of the literature. Dis Colon Rectum 50:1475–1477
Alkurt EG, Vardar YM, Tüzün İS (2022) Comparison of Limberg flap and Karydakis flap repair in pilonidal sinus surgery: a prospective case-control study. Cureus 14:e28933
de Parades V, Bouchard D, Janier M et al (2013) Pilonidal sinus disease. J Visc Surg 150:237–247
Gil LA, Deans KJ, Minneci PC (2023) Management of Pilonidal Disease: A Review. JAMA Surg
Grabowski J, Oyetunji TA, Goldin AB et al (2019) The management of pilonidal disease: a systematic review. J Pediatr Surg 54:2210–2221
Gips M, Melki Y, Salem L et al (2008) Minimal surgery for pilonidal disease using trephines: description of a new technique and long-term outcomes in 1,358 patients. Dis Colon Rectum 51:1656–1662
Fernandes S, Soares-Aquino C, Teixeira I et al (2022) Minimally invasive treatment of pilonidal sinus disease in a paediatric population: comparison of two techniques. ANZ J Surg 92:3288–3292
Zagory JA, Golden J, Holoyda K et al (2016) Excision and primary closure may be the better option in the surgical management of pilonidal disease in the pediatric population. Am Surg 82:964–967
RoldónGolet M, Siles Hinojosa A, González Ruiz Y et al (2021) Pilonidal sinus in adolescence: is there an ideal surgical approach? Cir Pediatr 34:119–124
Enriquez-Navascues JM, Emparanza JI, Alkorta M et al (2014) Meta-analysis of randomized controlled trials comparing different techniques with primary closure for chronic pilonidal sinus. Tech Coloproctol 18:863–872
Hardy EJO, Herrod PJ, Doleman B et al (2019) Surgical interventions for the treatment of sacrococcygeal pilonidal sinus disease in children: a systematic review and meta-analysis. J Pediatr Surg 54:2222–2233
Arnous M, Elgendy H, Thabet W et al (2019) Excision with primary midline closure compared with Limberg flap in the treatment of sacrococcygeal pilonidal disease: a randomised clinical trial. Ann R Coll Surg Engl 101:21–29
Yamout SZ, Caty MG, Lee YH et al (2009) Early experience with the use of rhomboid excision and Limberg flap in 16 adolescents with pilonidal disease. J Pediatr Surg 44:1586–1590
Kaya B, Eris C, Atalay S et al (2012) Modified Limberg transposition flap in the treatment of pilonidal sinus disease. Tech Coloproctol 16:55–59
Yildiz T, Ilce Z, Kücük A (2014) Modified Limberg flap technique in the treatment of pilonidal sinus disease in teenagers. J Pediatr Surg 49:1610–1613
Prieto JM, Checchi KD, Kling KM et al (2020) Trephination versus wide excision for the treatment of pediatric pilonidal disease. J Pediatr Surg 55:747–751
Sequeira JB, Coelho A, Marinho AS et al (2018) Endoscopic pilonidal sinus treatment versus total excision with primary closure for sacrococcygeal pilonidal sinus disease in the pediatric population. J Pediatr Surg 53:2003–2007
Bi S, Sun K, Chen S et al (2020) Surgical procedures in the pilonidal sinus disease: a systematic review and network meta-analysis. Sci Rep 10:13720
Ray K, Albendary M, Baig MK et al (2020) Limberg flap for the management of pilonidal sinus reduces disease recurrence compared to Karydakis and Bascom procedure: a systematic review and meta-analysis of randomized controlled trials. Minerva Chir 75:355–364
Doll D, Petersen S, Andreae OA et al (2022) Pit picking vs. Limberg flap vs. primary open method to treat pilonidal sinus disease–a cohort of 327 consecutive patients. Innov Surg Sci 7:23–29
Guner A, Boz A, Ozkan OF et al (2013) Limberg flap versus Bascom cleft lift techniques for sacrococcygeal pilonidal sinus: prospective, randomized trial. World J Surg 37:2074–2080
Dudink R, Veldkamp J, Nienhuijs S et al (2011) Secondary healing versus midline closure and modified Bascom natal cleft lift for pilonidal sinus disease. Scand J Surg 100:110–113
Gökbuget ZM, Özcan R, Karagöz A et al (2021) Endoscopic pilonidal sinus treatment (EPSiT) in the pediatric age group: short-term results. Ulus Travma Acil Cerrahi Derg 27:443–448
Velotti N, Manigrasso M, Di Lauro K et al (2019) Minimally invasive pilonidal sinus treatment: a narrative review. Open Med 14:532–536
Song Y, Zang Y, Chen Z et al (2023) The application of the Limberg flap repair technique in the surgical treatment of pilonidal sinus disease. Int Wound J 20:2241–2249
Gips M, Bendahan J, Ayalon S et al (2022) Minimal pilonidal surgery vs. common wide excision operations: better well-being and comparable recurrence rates. Isr Med Assoc J 24:89–95
Speter C, Zmora O, Nadler R et al (2017) Minimal incision as a promising technique for resection of pilonidal sinus in children. J Pediatr Surg 52:1484–1487
Doll D, Luedi MM (2020) The management of pilonidal disease in pediatric patients: some aspects of importance. J Pediatr Surg 55:206–207
Sinnott CJ, Glickman LT (2019) Limberg flap reconstruction for sacrococcygeal pilonidal sinus disease with and without acute abscess: Our experience and a review of the literature. Arch Plast Surg 46:235–240
Demiryas S, Donmez T (2019) Could early postoperative complications be considered as risk factor for recurrence after pilonidal sinus surgery? Chirurgia 114:475–486
Di Castro A, Guerra F, Levi Sandri GB et al (2016) Minimally invasive surgery for the treatment of pilonidal disease. The Gips procedure on 2347 patients. Int J Surg 36:201–205
Delshad HR, Henry O, Mooney DP (2020) Improving resource utilization and outcomes using a minimally invasive pilonidal protocol. J Pediatr Surg 55:182–186
Diéguez I, Costa A, Miró I et al (2022) En bloc resection vs. Gips procedure in pilonidal sinus surgery. Cir Pediatr 35:75–79
Braungart S, Powis M, Sutcliffe JR et al (2016) Improving outcomes in pilonidal sinus disease. J Pediatr Surg 51:282–284
Gendy AS, Glick RD, Hong AR et al (2011) A comparison of the cleft lift procedure vs wide excision and packing for the treatment of pilonidal disease in adolescents. J Pediatr Surg 46:1256–1259
Caniano DA, Ruth B, Teich S (2005) Wound management with vacuum-assisted closure: experience in 51 pediatric patients. J Pediatr Surg 40:128–132
Iesalnieks I, Ommer A, Herold A et al (2021) German National Guideline on the management of pilonidal disease: update 2020. Langenbecks Arch Surg 406:2569–2580
Stauffer VK, Luedi MM, Kauf P et al (2018) Common surgical procedures in pilonidal sinus disease: a meta-analysis, merged data analysis, and comprehensive study on recurrence. Sci Rep 8:3058
Delshad HR, Dawson M, Melvin P et al (2019) Pit-picking resolves pilonidal disease in adolescents. J Pediatr Surg 54:174–176
Acknowledgements
None.
Funding
Open access funding provided by SCELC, Statewide California Electronic Library Consortium. No funds, grants, or other support was received.
Author information
Authors and Affiliations
Contributions
WGL, CS, RGS, KSW, and JCP contributed to study conception and design. WGL, CS, AZ, VV, AS, KSW, JCP contributed to acquisition, analysis, and interpretation of the data. WGL, CS, KSW, JCP wrote the manuscript text and all of the authors contributed to the critical revision of the manuscript. All authors have approved this version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Declarations
The authors have no relevant financial or non-financial interests to disclose. This retrospective chart review study involving human participants was in accordance with the ethical standards of the international and national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The Institutional Review Board of Children’s Hospital Los Angeles approved this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lee, W.G., Short, C., Zhong, A. et al. Outcomes of pediatric pilonidal disease treatment: excision with off-midline flap reconstruction versus endoscopic pilonidal sinus treatment. Pediatr Surg Int 40, 46 (2024). https://doi.org/10.1007/s00383-023-05629-1
Accepted:
Published:
DOI: https://doi.org/10.1007/s00383-023-05629-1