Abstract
Purpose
To assess real-world educational outcomes, neurodevelopmental disorders and mental health disorders in patients with intestinal atresia (IA) and compare these to outcomes to age-matched controls.
Methods
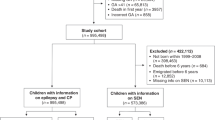
We performed a retrospective case–control study of children with IA born between 1991 and 2017. We evaluated educational outcomes using an Early Developmental Instrument, Grades 3, 7 and 8 assessments, Grade 9 completion and performance, high school graduation, and neurodevelopmental and mental health disorders using International Classification of Diseases codes available from a population-based dataset.
Results
We identified a total of 94 IA cases and 940 date-of-birth-matched controls. Cases with chromosomal anomalies were more likely to fail the Early Developmental Instrument (OR = 2.88, p = 0.037), Grade 8 reading (OR = 2.94, p = 0.043) and Grade 12 (OR = 3.25, p = 0.036); cases without chromosomal anomalies were at no greater risk than their peers of failing to meet expectations and did not have an increased risk of anxiety (OR = 0.48, p = 0.12), depression (OR = 0.74, p = 0.6) or hyperactivity disorder (OR = 1.92, p = 0.087).
Conclusions
Our study demonstrated that IA patients without chromosomal anomalies are not at higher risk of neurodevelopmental and mental health disorders than controls. These results will offer more accurate outcome predictions for parents of children with IA.
Similar content being viewed by others
Data availability
The datasets generated and/or analyzed during the current study are available from the corresponding author upon reasonable request.
References
Burjonrappa S, Crete E, Bouchard S (2011) Comparative outcomes in intestinal atresia: a clinical outcome and pathophysiology analysis. Pediatr Surg Int 27:437–442. https://doi.org/10.1007/s00383-010-2729-8
Walker K, Badawi N, Halliday R et al (2012) Early developmental outcomes following major noncardiac and cardiac surgery in term infants: a population-based study. J Pediatr 161:748–752. https://doi.org/10.1016/j.jpeds.2012.03.044
Moran MM, Gunn-Charlton JK, Walsh JM (2019) Associations of neonatal noncardiac surgery with brain structure and neurodevelopment: a prospective case-control study. J Pediatr 212:93–101. https://doi.org/10.1016/j.jpeds.2019.05.050
Stolwijk LJ, Keunen K, de Vries LS, eet al, (2017) Neonatal surgery for noncardiac congenital anomalies: neonates at risk of brain injury. J Pediatr 182:335–341. https://doi.org/10.1016/j.jpeds.2016.11.080
Rappaport BA, Suresh S, Hertz S et al (2015) Anesthetic neurotoxicity–clinical implications of animal models. N Engl J Med 372:796–797. https://doi.org/10.1056/nejmp1414786
Creeley CE, Dikranian KT, Dissen GA et al (2014) Isoflurane-induced apoptosis of neurons and oligodendrocytes in the fetal rhesus macaque brain. Anesthesiology 120:626–638. https://doi.org/10.1097/aln.0000000000000037
Miyake Y, Seo S, Kataoka K et al (2022) Significant neonatal intraoperative cerebral and renal oxygen desaturation identified with near-infrared spectroscopy. Pediatr Surg Int 38:737–742. https://doi.org/10.1007/s00383-022-05102-5
Kubota A, Nose K, Yamamoto E et al (2011) Psychosocial and cognitive consequences of major neonatal surgery. J Pediatr Surg 46:2250–2253. https://doi.org/10.1016/j.jpedsurg.2011.09.006
Chiu PP, Ijsselstijn H (2012) Morbidity and long-term follow-up in CDH patients. Eur J Pediatr Surg 22:384–392. https://doi.org/10.1055/s-0032-1329412
de Munck S, van der Cammen-van Zijp MHM, Zanen-van den Adel TPL et al (2021) Persisting motor function problems in school-aged survivors of congenital diaphragmatic hernia. Front Pediatr 9:729054
Frisk V, Jakobson LS, Unger S et al (2011) Long-term neurodevelopmental outcomes of congenital diaphragmatic hernia survivors not treated with extracorporeal membrane oxygenation. J Pediatr Surg 46:1309–1318. https://doi.org/10.1016/j.jpedsurg.2010.12.023
Costerus SA, Hendrikx DJIJ et al (2021) Cerebral oxygenation and activity during surgical repair of neonates with congenital diaphragmatic hernia: a center comparison analysis. Front Pediatr 9:798952
Wang X, Xu Z, Miao CH (2014) Current clinical evidence on the effect of general anesthesia on neurodevelopment in children: an updated systematic review with meta-regression. PLoS ONE 9:e85760
Roorda D, Königs M, Eeftinck Schattenkerk L et al (2021) Neurodevelopmental outcome of patients with congenital gastrointestinal malformations: a systematic review and meta-analysis. Arch Dis Child Fetal Neonatal Ed 106:635–642. https://doi.org/10.1136/archdischild-2021-322158
Kubota A, Yamakawa S, Yamamoto E et al (2016) Major neonatal surgery: psychosocial consequence of the patient and mothers. J Pediatr Surg 51:364–367. https://doi.org/10.1016/j.jpedsurg.2015.09.017
Bai Y, Yuan Z, Wang W et al (2000) Quality of life for children with fecal incontinence after surgically corrected anorectal malformation. J Pediatr Surg 35:462–464. https://doi.org/10.1016/s0022-3468(00)90215-x
Hassink EA, Rieu PN, Brugman AT et al (1994) Quality of life after operatively corrected high anorectal malformation: a long-term follow-up study of patients aged 18 years and older. J Pediatr Surg 29:773–776. https://doi.org/10.1016/0022-3468(94)90367-0
Grano C, Aminoff D, Lucidi F et al (2012) Long-term disease-specific quality of life in children and adolescent patients with ARM. J Pediatr Surg 47:1317–1322. https://doi.org/10.1016/j.jpedsurg.2012.01.068
Acknowledgements
The authors acknowledge the generosity of the patients and pediatric surgeons of the HSC-Children’s Hospital whose experiences made this study possible. This work was supported by grants from the DEVOTION Network and the Children’s Hospital Research Institute of Manitoba as well as Project Grant PJT-178387 from the Canadian Institutes of Health Research. Dr. Richard Keijzer is the Thorlakson Chair in Surgical Research for the Department of Surgery and the University of Manitoba. The authors acknowledge the Manitoba Centre for Health Policy for use of data contained in the Manitoba Population Research Data Repository under project # 2017/2018-29. The results and conclusions are those of the authors and no official endorsement by the Manitoba Centre for Health Policy, Manitoba Health, or other data providers are intended or should be inferred. Data used in this study are from the Manitoba Population Research Data Repository housed at the Manitoba Centre for Health Policy, University of Manitoba, and were derived from data provided by Manitoba Health.
Author information
Authors and Affiliations
Contributions
YM, SLM and RK designed the study YM and SLM analyzed the data YM, SLM and RK wrote the manuscript YM, SLM, AY and RK critically reviewed and revised the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, I hereby declare that we have no competing interests that might be perceived to influence the results and/or discussion reported in this paper.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Miyake, Y., Lum Min, S.A., Yamataka, A. et al. The impact of intestinal atresia on educational and mental health outcomes in school-aged children: A case–control cohort study. Pediatr Surg Int 39, 86 (2023). https://doi.org/10.1007/s00383-022-05357-y
Accepted:
Published:
DOI: https://doi.org/10.1007/s00383-022-05357-y