Abstract
Purpose
The management of pediatric ovarian neoplasms (ON) is based on finding a balance between adequate surgical treatment and future reproductive capacity. We aimed to evaluate long-term results of patients who underwent surgery for ON.
Methods
A retrospective cohort study design was used. Medical records of patients with ON were reviewed. They were invited to participate in a telephone-based survey assessing complaints, menstrual status, and post-surgical recurrence.
Results
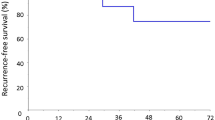
Eighty-five patients were operated for ON between 1995 and 2015. Median age at surgery was 14.7 years. 62.4% of patients had ovary-sparing surgery (OSS). Median tumor size in oophorectomy group was significantly larger than OSS group (p = 0.029). Median length of follow-up was 5.1 years. Recurrent/metachronous disease was not significantly different between OSS and oophorectomy groups (p = 1.000). In OSS group, irregular menses (p = 0.004) and painful menses (p = 0.002) were significantly higher than oophorectomy group.
Conclusion
The main goal of treatment in pediatric ON is to find the right balance between adequate and appropriate tumor resection and maximal effort for fertility preservation. Our results showed no difference between oophorectomy and OSS in the terms of recurrence. Although irregular and painful menses were found to be significantly higher in the OSS group, longer follow-up and prospective studies are needed to clarify this issue.

Similar content being viewed by others
References
Taskinen S, Fagerholm R, Lohi J, Taskinen M (2015) Pediatric ovarian neoplastic tumors: Incidence, age at presentation, tumor markers and outcome. Acta Obstet Gynecol Scand 94:425–429. https://doi.org/10.1111/aogs.12598
Amies Oelschlager AME, Gow KW, Morse CB, Lara-Torre E (2016) Management of large ovarian neoplasms in pediatric and adolescent females. J Pediatr Adolesc Gynecol 29:88–94. https://doi.org/10.1016/j.jpag.2014.07.018
Papic JC, Finnell SME, Slaven JE, Billmire DF, Rescorla FJ, Leys CM (2014) Predictors of ovarian malignancy in children: Overcoming clinical barriers of ovarian preservation. J Pediatr Surg 49:144–148. https://doi.org/10.1016/j.jpedsurg.2013.09.068
Braungart S, Craigie RJ, Losty PD (2018) Controversies in the management of ovarian tumours in prepubertal children—A BAPS and UK CCLG surgeons cancer group national survey. J Pediatr Surg 53:2231–2234. https://doi.org/10.1016/j.jpedsurg.2017.11.068
Szymon O, Bogusz B, Taczanowska-Niemczuk A, Maślanka M, Górecki W (2021) Ovarian sparing surgery in mature ovarian teratomas in children: a 20-year single-center experience. Eur J Pediatr Surg 31:2–7. https://doi.org/10.1055/s-0040-1716877
Braungart S, Craigie RJ, Farrelly P, Losty PD (2020) Operative management of pediatric ovarian tumors and the challenge of fertility-preservation: results from the UK CCLG Surgeons Cancer Group Nationwide Study. J Pediatr Surg 55:2425–2429. https://doi.org/10.1016/j.jpedsurg.2020.02.057
Lawrence AE, Fallat ME, Hewitt G, Hertweck P, Onwuka A, Afrazi A et al (2020) Understanding the value of tumor markers in pediatric ovarian neoplasms. J Pediatr Surg 55:122–125. https://doi.org/10.1016/j.jpedsurg.2019.09.062
Rosendahl M, Simonsen MK, Kjer JJ (2017) The influence of unilateral oophorectomy on the age of menopause. Climacteric 20:540–544. https://doi.org/10.1080/13697137.2017.1369512
Shuster LT, Rhodes DJ, Gostout BS, Grossardt BR, Rocca WA (2010) Premature menopause or early menopause: Long-term health consequences. Maturitas 65:161–166. https://doi.org/10.1016/j.maturitas.2009.08.003
Taskinen S, Urtane A, Fagerholm R, Lohi J, Taskinen M (2014) Metachronous benign ovarian tumors are not uncommon in children. J Pediatr Surg 49:543–545. https://doi.org/10.1016/j.jpedsurg.2013.09.019
Çelik A, Ergün O, Aldemir H, Özcan C, Özok G, Erdener A et al (2005) Long-term results of conservative management of adnexal torsion in children. J Pediatr Surg 40:704–708. https://doi.org/10.1016/j.jpedsurg.2005.01.008
Braungart S, Craigie RJ, Farrelly P, Losty PD (2020) Ovarian tumors in children: how common are lesion recurrence and metachronous disease? A UK CCLG Surgeons Cancer Group nationwide study. J Pediatr Surg 55:2026–2029. https://doi.org/10.1016/j.jpedsurg.2019.10.059
Yasui T, Hayashi K, Mizunuma H, Kubota T, Aso T, Matsumura Y et al (2012) Factors associated with premature ovarian failure, early menopause and earlier onset of menopause in Japanese women. Maturitas 72:249–255. https://doi.org/10.1016/j.maturitas.2012.04.002
Palomba S, Zupi E, Russo T, Falbo A, Del Negro S, Manguso F et al (2007) Comparison of two fertility-sparing approaches for bilateral borderline ovarian tumours: a randomized controlled study. Hum Reprod 22:578–585. https://doi.org/10.1093/humrep/del381
Chaloutsou K, Aggelidis P, Pampanos A, Theochari E, Michala L (2017) Premature ovarian insufficiency: an adolescent Series. J Pediatr Adolesc Gynecol. https://doi.org/10.1016/j.jpag.2017.04.003
Avis NE, Brockwell S, Colvin A (2005) A universal menopausal syndrome? Am J Med 118:37–46. https://doi.org/10.1016/j.amjmed.2005.09.057
Rocca WA, Grossardt BR, Shuster LT, Stewart EA (2012) Hysterectomy, oophorectomy, estrogen, and the risk of dementia. Neurodegener Dis 10:175–178. https://doi.org/10.1159/000334764
Oltmann SC, Garcia NM, Barber R, Hicks B, Fischer AC (2010) Pediatric ovarian malignancies: how efficacious are current staging practices? J Pediatr Surg 45:1096–1102. https://doi.org/10.1016/j.jpedsurg.2010.02.069
Terzic M, Rapisarda AMC, Della Corte L, Manchanda R, Aimagambetova G, Norton M et al (2020) Diagnostic work-up in paediatric and adolescent patients with adnexal masses: an evidence-based approach. J Obstet Gynaecol (Lahore). https://doi.org/10.1080/01443615.2020.1755625
Depoers C, Martin F-A, Nyangoh Timoh K, Morcet J, Proisy M, Henno S et al (2019) A preoperative scoring system for adnexal mass in children and adolescents to preserve their future fertility. J Pediatr Adolesc Gynecol 32:57–63. https://doi.org/10.1016/j.jpag.2018.08.009
Xac MC, Jetelina KK, Jarin J, Wilson E (2021) Benign, borderline, and malignant pediatric adnexal masses: a 10-year review. J Pediatr Adolesc Gynecol 34:454–461. https://doi.org/10.1016/j.jpag.2021.01.002
Kirkham YA, Lacy JA, Kives S, Allen L (2011) Characteristics and management of adnexal masses in a Canadian pediatric and adolescent population. J Obstet Gynaecol Canada 33:935–943. https://doi.org/10.1016/S1701-2163(16)35019-8
Renaud EJ, Sømme S, Islam S, Cameron DB, Gates RL, Williams RF et al (2019) Ovarian masses in the child and adolescent: an American Pediatric Surgical Association Outcomes and Evidence-Based Practice Committee systematic review. J Pediatr Surg 54:369–377. https://doi.org/10.1016/j.jpedsurg.2018.08.058
Ye G, Xu T, Liu J, Xu W, Lv Z (2020) The role of preoperative imaging and tumor markers in predicting malignant ovarian masses in children. Pediatr Surg Int 36:333–339. https://doi.org/10.1007/s00383-019-04591-1
Stanković ZB, Sedlecky K, Savić D, Lukač BJ, Mažibrada I, Perovic S (2017) Ovarian preservation from tumors and torsions in girls: prospective diagnostic study. J Pediatr Adolesc Gynecol 30:405–412. https://doi.org/10.1016/j.jpag.2017.01.008
Spinelli C, Strambi S, Liloia C, Bertocchini A, Messineo A (2016) Update on the surgical management of ovarian neoplasms in children and adolescents: analysis on 32 cases. Gynecol Endocrinol 32:787–791. https://doi.org/10.1080/09513590.2016.1190819
Arthur F, Hennessey I, Pizer B, Losty PD (2021) Surgical management and outcomes of paediatric ovarian tumours—a 25-year UK single centre experience. Pediatr Surg Int 37:1355–1359. https://doi.org/10.1007/s00383-021-04950-x
Cass DL (2005) Ovarian torsion. Semin Pediatr Surg 14:86–92. https://doi.org/10.1053/j.sempedsurg.2005.01.003
Galinier P, Carfagna L, Delsol M, Ballouhey Q, Lemasson F, Le Mandat A et al (2009) Ovarian torsion. Management and ovarian prognosis: a report of 45 cases. J Pediatr Surg 44:1759–1765. https://doi.org/10.1016/j.jpedsurg.2008.11.058
Oltmann SC, Fischer A, Barber R, Huang R, Hicks B, Garcia N (2010) Pediatric ovarian malignancy presenting as ovarian torsion: incidence and relevance. J Pediatr Surg 45:135–139. https://doi.org/10.1016/j.jpedsurg.2009.10.021
Qazi SH, Jeelani SM, Dogar SA, Das JK, Saxena AK (2020) Approaches to the management of pediatric ovarian masses in the 21st century: Systematic review and meta-analysis. J Pediatr Surg 55:357–368. https://doi.org/10.1016/j.jpedsurg.2019.09.003
Łuczak J, Bagłaj M (2017) Selecting treatment method for ovarian masses in children - 24 years of experience. J Ovarian Res 10:1–9. https://doi.org/10.1186/s13048-017-0353-0
Oue T, Uehara S, Sasaki T, Nose S, Saka R, Yamanaka H et al (2015) Treatment and ovarian preservation in children with ovarian tumors. J Pediatr Surg 50:2116–2118. https://doi.org/10.1016/j.jpedsurg.2015.08.036
Kolstad HA, Bonde JP, Hjøllund NH, Jensen TK, Henriksen TB, Ernst E et al (1999) Menstrual cycle pattern and fertility: a prospective follow-up study of pregnancy and early embryonal loss in 295 couples who were planning their first pregnancy. Fertil Steril 71:490–496. https://doi.org/10.1016/S0015-0282(98)00474-9
Gardner J (1983) Adolescent menstrual characteristics as predictors of gynaecological health. Ann Hum Biol 10:31–40. https://doi.org/10.1080/03014468300006161
Zhai A, Axt J, Hamilton EC, Koehler E, Lovvorn HN (2012) Assessing gonadal function after childhood ovarian surgery. J Pediatr Surg 47:1272–1279. https://doi.org/10.1016/j.jpedsurg.2012.03.038
Azarakhsh N, Grimes S, Chotai PN, Shephard C, Huang EY (2017) Post-resection outcomes for pediatric ovarian neoplasm: is ovarian-preserving surgery a good option? Pediatr Surg Int 33:97–104. https://doi.org/10.1007/s00383-016-3987-x
Author information
Authors and Affiliations
Contributions
BTK is a consultant for study conception and design, data acquisition, analysis and data interpretation and drafting of the manuscript. ZD is a consultant for drafting of the manuscript. ED is a consultant for analysis and data interpretation. OE is a consultant for critical revision. GO is a consultant for critical revision. AC is a consultant for study conception—design and critical revision.
Corresponding author
Ethics declarations
Conflict of interest
None of the authors has anything to disclose or conflict of interest. Each author participated sufficiently in the work to take public responsibility for appropriate portions of the manuscript contents.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Toker Kurtmen, B., Dokumcu, Z., Divarci, E. et al. Long-term surgical outcomes in pediatric ovarian neoplasms: 20-year single-center experience. Pediatr Surg Int 38, 2035–2044 (2022). https://doi.org/10.1007/s00383-022-05256-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-022-05256-2