Abstract
Objective
Biliary atresia (BA) is a neonatal liver disease and requires Kasai portoenterostomy. Many patients develop postoperative cholangitis, resulting in a poor prognosis. The preventive strategy of antibiotics is empirical and lacks a standard regimen. We aimed to analyze the effect of different durations of prophylactic intravenous antibiotics against post-Kasai cholangitis.
Study design
A single-center, open-labeled, randomized clinical trial was performed from June 2016 to August 2017. One hundred and eighty BA patients were recruited and randomized into a short-term (n = 90) and a long-term (n = 90) treatment group, and prophylactic intravenous antibiotics were used for 7 versus 14 days, respectively. The primary outcome was the overall cholangitis incidence within 6-months post-Kasai portoenterostomy. The secondary outcomes included cholangitis incidence within 1 and 3 months post-Kasai portoenterostomy, the onset and average episodes of cholangitis, jaundice clearance rate, native liver survival rate, and adverse events within 6-months post-Kasai portoenterostomy.
Results
The cholangitis incidence within 6-months post-Kasai in the short-term group was similar to the long-term group (62% vs. 70%, p = 0.27) with intention-to-treat and pre-protocol analysis. There was no significant difference in jaundice clearance rate or native liver survival rate between the two groups. However, the percentage of early onset (61% vs. 38%, p = 0.02) and average episodes (2.4 ± 0.2 vs. 1.8 ± 0.1 episodes, p = 0.01) of cholangitis were lower in the long-term group.
Conclusion
Long-term intravenous antibiotics can be replaced by the short-term regimen in the general protection against post-Kasai cholangitis.

Similar content being viewed by others
Data availability
This trial was registered at the Chinese Clinical Trial Registry (http://www.chictr.org.cn/), title “Therapeutic effect of prophylactic intravenous antibiotics after Kasai procedure in biliary atresia patients”, registration number: ChiCTR-IPR-16008609. This article is licensed under a Creative Commons Attribution 4.0 International License. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. Application should be submitted to szheng@shmu.edu.cn.
References
Qiao G, Li L, Cheng W, Zhang Z, Ge J, Wang C (2015) Conditional probability of survival in patients with biliary atresia after Kasai portoenterostomy: a Chinese population-based study. J Pediatr Surg 50(8):1310–1315. https://doi.org/10.1016/j.jpedsurg.2015.03.062
Davenport M, Kerkar N, Mieli-Vergani G, Mowat AP, Howard ER (1997) Biliary atresia: the King’s college hospi- tal experience (1974–1995). J Pediatr Surg 32:479–485. https://doi.org/10.1016/S0022-3468(97)90611-4
Nio M, Ohi R (2000) Biliary atresia. Semin Pediatr Surg 9:177–186. https://doi.org/10.1053/spsu.2000.18846
Gottrand F, Bernard O, Hadchouel M, Pariente D, Gauthier F, Alagille D (1991) Late cholangitis after successful surgical repair of biliary atresia. Am J Dis Child 145:213–215. https://doi.org/10.1001/archpedi.1991.02160020107028
Nio M, Sano N, Ishii T, Sasaki H, Hayashi Y, Ohi R (2004) Cholangitis as a late complication in long-term survivors after surgery for biliary atresia. J Pediatr Surg 39(12):1797–1799. https://doi.org/10.1016/j.jpedsurg.2004.08.021
Davenport M, Grieve A (2012) Maximizing Kasai portoenterostomy in the treatment of biliary atresia: medical and surgical options. S Afr Med J 102(11 Pt 2):865–867. https://doi.org/10.7196/samj.6120
Stringer MD, Davison SM, Rajwal SR, McClean P (2007) Kasai portoenterostomy: 12-year experience with a novel adjuvant therapy regimen. J Pediatr Surg 42(8):1324–1328. https://doi.org/10.1016/j.jpedsurg.2007.03.026
Decharun K, Leys CM, West KW, Finnell SM (2016) Prophylactic antibiotics for prevention of cholangitis in patients with biliary atresia status post-kasai portoenterostomy: a systematic review. Clin Pediatr (Phila) 55(1):66–72. https://doi.org/10.1177/0009922815594760
Nio M, Wada M, Sasaki H, Kazama T, Tanaka H, Kudo H (2016) Technical standardization of Kasai portoenterostomy for biliary atresia. J Pediatr Surg 51(12):2105–2108. https://doi.org/10.1016/j.jpedsurg.2016.09.047
Kobayashi A, Utsunomiya T, Kawai S, Ohbe Y (1976) Congenital biliary atresia. Analysis of 97 cases with reference to prognosis after hepatic portoenterostomy. Am J Dis Child 130(8):830–833. https://doi.org/10.1001/archpedi.1976.02120090040007
Hitch DC, Lilly JR (1978) Identification, quantification, and significance of bacterial growth within the biliary tract after Kasai’s operation. J Pediatr Surg 13(6D):563–569. https://doi.org/10.1016/s0022-3468(78)80094-3
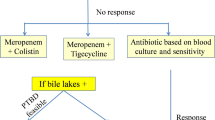
Pang WB, Zhang TC, Chen YJ, Peng CH, Wang ZM, Wu DY, Wang K (2019) Ten-year experience in the prevention of post-kasai cholangitis. Surg Infect (Larchmt) 20(3):231–235. https://doi.org/10.1089/sur.2018.047
Wong KK, Fan AH, Lan LC, Lin SC, Tam PK (2004) Effective antibiotic regime for postoperative acute cholangitis in biliary atresia–an evolving scene. J Pediatr Surg 39(12):1800–1802. https://doi.org/10.1016/j.jpedsurg.2004.08.027
Bu LN, Chen HL, Chang CJ, Ni YH, Hsu HY, Lai HS, Hsu WM, Chang MH (2003) Prophylactic oral antibiotics in prevention of recurrent cholangitis after the Kasai portoenterostomy. J Pediatr Surg 38:590–593. https://doi.org/10.1053/jpsu.2003.50128
Petersen C, Harder D, Melter M, Becker T, Wasielewski RV, Leonhardt J, Ure BM (2008) Postoperative high-dose steroids do not improve mid-term survival with native liver in biliary atresia. J Gastroenterol 103(3):712–719. https://doi.org/10.1111/j.1572-0241.2007.01721.x
Muraji T, Tsugawa C, Nishijima E, Satoh S, Takamizawa S, Ise K, Maekawa T (2002) Surgical management for intractable cholangitis in biliary atresia. J Pediatr Surg 37(12):1713–1715. https://doi.org/10.1053/jpsu.2002.36703
Koga H, Wada M, Nakamura H et al (2013) Factors influencing jaundice-free survival with the native liver in post-portoenterostomy biliary atresia patients: results from a single institution. J Pediatr Surg 48(12):2368–2372. https://doi.org/10.1016/j.jpedsurg.2013.08.007
Chung PH, Wong KK, Tam PK (2015) Predictors for failure after Kasai operation. J Pediatr Surg 50(2):293–296. https://doi.org/10.1016/j.jpedsurg.2014.11.015
Shin JH, Chang EY, Chang HK, Kim SM, Han SJ (2011) Home intravenous antibiotic treatment for intractable cholangitis in patients with biliary atresia following Kasai portoenterostomies. Korean Surg Soc 80(5):355–361. https://doi.org/10.4174/jkss.2011.80.5.355
Zhang D, Yang HY, Jia J, Zhao G, Yue M, Wang JX (2014) Postoperative steroids after Kasai portoenterostomy for biliary atresia: a meta-analysis. Int J Surg 12(11):1203–1209. https://doi.org/10.1016/j.ijsu.2014.08.407
Lee JY, Lim LT, Quak SH, Prabhakaran K, Aw M (2014) Cholangitis in children with biliary atresia: health-care resource utilisation. J Paediatr Child Health 50(3):196–201. https://doi.org/10.1111/jpc.12463
Chen SY, Lin CC, Tsan YT, Chan WC, Wang JD, Chou YJ, Lin CH (2018) Number of cholangitis episodes as a prognostic marker to predict timing of liver transplantation in biliary atresia patients after Kasai portoenterostomy. BMC Pediatr 18(1):119. https://doi.org/10.1186/s12887-018-1074-2
Burns J, Davenport M (2020) Adjuvant treatments for biliary atresia. Transl Pediatr 9(3):253–265. https://doi.org/10.21037/tp.2016.10.08
Cheng K, Molleston JP, Bennett WE Jr (2020) Cholangitis in patients with biliary atresia receivinghepatoportoenterostomy: a national database study. J Pediatr Gastroenterol Nutr 71(4):452–458. https://doi.org/10.1097/MPG.0000000000002836
Lünzmann K, Schweizer P (1999) The influence of cholangitis on the prognosis of extrahepatic biliary atresia. Eur J Pediatr Surg 9:19–23. https://doi.org/10.1055/s-2008-1072206
Yassin NA, El-Tagy G, Abdelhakeem ON, Asem N, El-Karaksy H (2020) Predictors of short-term outcome of kasai portoenterostomy for biliary atresia in infants: a single-center study. Pediatr Gastroenterol Hepatol Nutr 23(3):266–275. https://doi.org/10.5223/pghn.2020.23.3.266
Okubo R, Nio M, Sasaki H, Japanese Biliary Atresia Society (2021) impacts of early kasai portoenterostomy on short-term and long-term outcomes of biliary atresia. Hepatol Commun 5(2):234–243. https://doi.org/10.1002/hep4.1615
Davenport M, Ong E, Sharif K, Alizai N, McClean P, Hadzic N, Kelly DA (2011) Biliary atresia in England and Wales: results of centralization and new benchmark. J Pediatr Surg 46(9):1689–1694. https://doi.org/10.1016/j.jpedsurg.2011.04.013
Kiriyama S, Kozaka K, Takada T et al (2018) Tokyo Guidelines 2018: diagnostic criteria and severity grading of acute cholangitis. J Hepato-biliary Pancreat Sci 25:17–30. https://doi.org/10.1002/jhbp.512
Acknowledgements
We would like to thank all the doctors and nurses in the Department of Pediatric Surgery of Children’s Hospital of Fudan University for the cooperation during the trial. We would like to thank professor Weili Yan from the Department of Clinical Epidemiology, Children’s Hospital of Fudan University for the help in study design and statistical analyses.
Funding
This study was supported by the Shanghai Hospital Development Center (Grant No SHDC12014106), Shanghai Key Disciplines (Grant No.2017ZZ02022), Shanghai Outstanding Youth Medical Talents (Grant No EK00000622), National Natural Science Foundation of China (Grant No 81873545).
Author information
Authors and Affiliations
Contributions
Conceptualization and design of the study: Shan Zheng, Jia Liu, YanLei Huang, Gong Chen. Data collection coordination and supervision: SZ, GC Data collection instruments design: XL, RD, ZS. Data collection: JL, YH, GC, SS, YW. Data analyses: JL, XL, RD, SS, YW, GC. Manuscript drafting: GC, JL, XL, RD, SS, YW. Manuscript review and revise: SZ, GC, JJ. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Conflict of interest
All the authors declare that they have no conflict of interest.
Ethical approval
This study was approved by the Ethics Board for Human Research of the Children’s Hospital of Fudan University, Shanghai, China in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and later amendments.
Consent to participate
Parents and/or legal guardians were appropriately informed and gave written consent for the participation of the participants in this study in all cases.
Consent to publication
All authors consent that this manuscript, if accepted, will be published in Pediatric Surgery International.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chen, G., Liu, J., Huang, Y. et al. Preventive effect of prophylactic intravenous antibiotics against cholangitis in biliary atresia: a randomized controlled trial. Pediatr Surg Int 37, 1089–1097 (2021). https://doi.org/10.1007/s00383-021-04916-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-021-04916-z