Abstract
Aim
To study delayed presentation of ARMs, management and its effect on surgical and functional complications.
Methods
It is a retrospective study from March 2015 to March 2020. All the patients satisfying the criteria of delayed ARMs, i.e., presenting 7 days after birth were included. Information regarding type of ARM, mode of presentation, time of presentation, associated anomalies, management strategy, postoperative complications and functional outcome was noted. Minimum follow-up period was 6 months.
Results
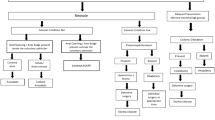
Out of 102 patients with ARM, 44 patients presented late. Among the 44 patients, 9 were males and 35 were females. Associated comorbidities observed are low birth weight (n = 9) and preterm (n = 13). Associated anomalies observed were cardiac (n = 18), renal (n = 8), other gastrointestinal (n = 5) and skeletal (n = 1). (1) Male: rectourethral fistula—2 (staged repair), anal stenosis—3 (anoplasty) and anocutaneous fistula—4 (anoplasty). (2) Female: vestibular fistula: 15 (6 primary definitive surgery + 9 staged repair), ectopic anus: 3 (staged repair), anal stenosis: 2 (anoplasty), urogenital sinus: 4 (staged repair), H-type ARM: 8 (staged repair) and persistent cloaca: 3 (staged repair). Primary repair was done in 15 patients (34%), and staged repair was done in 29 patients (65.9%). Anoplasty was done in 9 patients, ASARP (modified tsuchida’s procedure) in 8 patients and PSARP in 27 patients. Postoperative complications observed were constipation (n = 21, 47.7%), fecal incontinence (n = 12, 27.27%) with perianal excoriation in 2 patients, anal stenosis (n = 3, 6.8%) and rectal mucosal prolapse (n = 2, 4.5%)
Conclusion
Delayed presentation of ARMs is not uncommon and is more common in females. Management is almost similar to those who present early. Those who present with chronic constipation and megarectum require staged repair. Complications were more frequent with delayed presentation. Hence, every newborn should have careful examination of perineum and screened for ARM to avoid possible morbidity and mortality.





Similar content being viewed by others
References
Taiwo JO, Abdurrahman LO, Nasir AA, Odi TO (2009) Primary PSARP in the adolescent girl: how safe? Afr J Surg 6:144–153
Eltayeb A (2010) Delayed presentation of anorectal malformations: the possible associated morbidity and mortality. Pediatr Surg Int 26(8):801–806
Gangopadhyay AN, Pandey V (2015) Anorectal malformations. J Indian Assoc Pediatr Surg 20:10–15
Soeselo D, Grimaldy G, Susilawati, (2020) Delayed diagnosis of congenital anorectal malformation. J Pediatr Surg Case Reports 57:101446
Lindley R, Shawis R, Roberts J (2006) Delays in the diagnosis of anorectal malformations are common and significantly increase serious early complications. Acta Paediatr 95(3):364–368
Haider N, Fischer R (2007) Mortality and morbidity associated with late diagnosis of anorectal malformations in children. Surgeon 5:327–330
Sinha SK, Kanojia RP, Wakhlu A, Rawat JD, Kureel SN, Tandon RK (2008) Delayed presentation of anorectal malformations. J Indian Assoc Pediatr Surg 13:64–68
Sharma S, Gupta D (2012) Delayed presentation of anorectal malformation for definitive surgery. Pediatr Surg Int 28(8):831–834
Negm M, Khedre M (2020) Two-stage repair for delayed presentation of anorectal malformation with vestibular and perineal fistulae in females. Egyptian J Surgery 39(2):401
Sham M, Singh D, Phadke D (2012) Anorectal malformations: definitive management during and beyond adolescence. J Indian Assoc Pediatr Surg 17:120–123
Kim HL, Gow KW, Penner JG, Blair GK, Murphy JJ, Webber EM (2000) Presentation of low anorectal malformations beyond the neonatal period. Pediatrics 105:E68
Rathod K, Bawa M, Rao K, Mahalik S, Samujh R (2011) Delayed presentation of anorectal malformations: need of community awareness. Indian J Public Health 55(2):135
Karkera PJ, Kothari PR, Gupta RK, Gupta AR, Ranjan RR, Kesan K (2012) Delayed primary presentation of a male child with high anorectal malformation: a case report and review of relevant literature. Ann Trop Med Public Health 5:600–602
Grechukhina O, Gressel G, Taylor G, Schwartz J, Welsh R (2014) Unusual presentation of a rectovestibular fistula as gastrointestinal hemorrhage in a postmenopausal woman. Case Rep Obstet Gynecol 2014:1–3
Sandlas G, Kothari P, Sarda D, Karkera P (2011) Spontaneous bowel perforation in a neonate with anorectal malformation. Saudi J Gastroenterol 17(1):72
Chalapathi G, Chowdhary S, Rao K, Samujh R, Narasimhan K, Mahajan J et al (2004) Risk factors in the primary management of anorectal malformations in Northern India. Pediatr Surg Int 20(6):408–411
Bhatnagar V (2005) Assessment of postoperative results in anorectal malformations. J Indian Assoc Pediatr Surg 10:80–85
Chakravartty S, Maitey K, Ghosh D, Choudhury CR, Das S (2009) Successful management in neglected cases of adult anorectal malformation. Singapore Med J 50:e280–e282
Tareen F, Coyle D, Aworanti OM, Gillick J (2013) Delayed diagnosis of anorectal malformation–a persistent problem. Ir Med J 106(8):238–240 (PMID: 24282893)
Moss GD, Cartilidge PH, Speidel BD, Chambers TL (1991) Routine examination in the neonatal period. BMJ 302:878–879
Bloomfield L, Rogers C, Townsend J, Wolke D, Quist-Therson E (2003) The quality of routine examinations of the newborn performed by midwives and SHOs; an evaluation using video recordings. J Med Screen 10:176–180
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Divya, G., Kundal, V.K., Debnath, P.R. et al. Delayed presentation of anorectal malformations in a tertiary care hospital in India. Pediatr Surg Int 37, 451–456 (2021). https://doi.org/10.1007/s00383-020-04843-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-020-04843-5