Abstract
Polyps in gastrointestinal tract are mostly benign and result from hamartomas or lymphoid hyperplasia of submucosa. They usually occur as isolated lesions in children and are referred to as juvenile polyps. Multiple polyps with inherited origin are called polyposis and can be seen as a part of the syndrome. The polyps with adenomatous histopathology have malignant potential and necessitate genetic testing and colonoscopy to define the risk of cancer. Although simple endoscopic removal is adequate in the treatment of juvenile polyps, children with familial adenomatous polyposis (FAP) need total colectomy with ileorectal anastomosis (IRA) or ileal pouch-anal anastomosis (IPAA). The timing of prophylactic colectomy and the type of surgical treatment are controversial in children. The clinical features, the assessment of cancer risk, and the alternatives of the surgical treatment of polyps are reviewed in this paper.





Similar content being viewed by others
References
Mestre JR (1986) The changing patterns of juvenile polyps. Am J Gastroenterol 81:312–314
Louw JH (1968) Polypoid lesions of large bowel in children with particular reference to benign lymphoid polyposis. J Pediatr Surg 3:195–209
Verse M (1908) Ueber die Histogenese der Schlerinhautcarcinome. Verh Dtsch Ges Pathol 2:95
Marson BC (1962) Some peculiarities in the histology of intestinal polyps. Dis Colon Rectum 5:337–3344
McColl I, Busxey HY, Veale AM, Morson BC (1964) Juvenile polyposis coli. Proc R Soc Med 57:896–897
Lelli JL (2012) Polypoid disease of gastrointestinal tract in children. In: Coran A, Adzick NS, Krummel T, Leberge JM, Shamberger RC, Caldamone AA (eds) Pediatric surgery, 7th Edition, Mosby, pp 1177–1185
Gupta SK, Fitzgerald JF, Croffie JM et al (2001) Experience with juvenile polyps in North American children: the need for pancolonoscopy. Am J Gastroenterol 96:1695–1697
Fox VL, Perros S, Jiang H, Goldsmith JD (2010) Juvenile polyps recurrence in patients with multiple and solitary polyps. Clin Gastroenterol Hepatol 8:795–799
İbrahimi N, Septer SS, Lee BR, Garola R, Shah R, Attard TM (2019) Polyp characteristics of nonsyndromic and potentially syndromic juvenile polyps. A retrospective cohort analysis. J Pediatr Gastroenterol Nutr 69:668–672
Patel R, Hyer W (2019) Practical management of polyposis syndromes. Frontline Gastroenterol 10:379–387
Brosens LA, Van Hattem A, Hylind LM et al (2007) Risk of colorectal cancer in juvenile polyposis. Gut 56:965–967
Cohen S, Hyer W, Mas E, Auth M, Attard TM, Spalinger J, Latchford A, Durno C (2019) Management of juvenile polyposis syndrome in children and adolescents: a position paper form ESPGHAN polyposis working group. J Pediatr Gastroenterol Nutr 68:453–462
Jass JR, Williams CB, Bussey HJ et al (1988) Juvenile polyposis: a precancerous condition. Histopathology 13:619–630
Brazowski E, Misonzhnick-Bedny F, Rozen P (2004) Cyclooxygenase-2 expression in the hereditary mixed polyposis syndrome. Dig Dis Sci 49:1906–1911
Ishida H, Ishibashi K, Iwama T et al (2018) Malignant tumors associated with juvenile polyposis syndrome in Japan. Surg Today 48:253–263
Latchford A, Cohen S, Auth M, Scaillon M, Viala J, Daniels R, Talbotec C, Attard T, Durno C, Hyer W (2019) Management of Peutz-Jegher Syndrome in children and adolescents: a position paper from the ESPGHAN Polyposis Working Group. J Pediatr Gastroenterol Nutr 68:442–452
Goldstein SA, Hoffenberg EJ (2013) Peutz-Jegher syndrome in childhood: need for updated recommendations? J Pediatr Gastroenterol Nutr 56:191–195
Hinds R, Philp C, Hyer W et al (2004) Complications of childhood Peutz-Jeghers syndrome: implications for paediatric screening. J Pediatr Gastroenterol Nutr 39:219–220
Latchford AR, Neale K, Phillips RK et al (2011) Peutz-Jeghers syndrome: intriguing suggestion of gastrointestinal cancer prevention from surveillance. Dis Colon Rectum 54:1547–1551
Hayer W, Cohen S, Attard T, Vila-Viravet M, Pieanar C, Auth M, Septer S, Hawkins J, Durno C, Latchford A (2019) Management of familiar adenomatous polyps in children and adolescents. Position Paper from ESPGHAN Polyposis Working Group. J Pediatr Gastroenterol Nutr 68:428–441
Vasen HF, Griffioen G, Offenhaus GJ et al (1990) The value of screening and central registration of families with familial adenomatous polyposis. A study of 82 families in the Netherlands. Dis Colon Rectum 33:227–230
Latchford A (2015) Long term data for chemoprevention in colorectal disease in familial adenomatous polyposis. Fam Cancer 14:S47
Burn J, Chapman PD, Burn J et al (1997) Endoscopic screening and surgery for familial adenomatous polyposis: dangerous delays. Br J Surg 84:74–77
Vasen HF, Van der Luijt RB, Slors JF et al (1996) Molecular genetic tests as a guide to surgical management of familial adenomatous polyposis. Lancet 348:433–435
Olsen KO, Juul S, Bulow A et al (2003) Female fecundity before and after operation for familial adenomatous polyposis. Br J Surg 90:227–231
Thomson JPS (1990) Familial adenomatous polyposis: the large bowel. Ann R Coll Surgeons Eng 72:172–180
Bussey HJR, Eyers AA (1985) Ritchie SM Thomson JPS. The rectum in adenomatous polyposis: the St Mark’s policy. Br J Surg 72:29–31
Seethramaiah R, West BT, Ignash SJ, Pakarinen MP, Koivusalo A, Rintala R, Liu DC, Spencer AU et al (2009) Outcomes in pediatric patients undergoing straight vs J pouch ileoanal anastomosis: a multicenter analysis. J Pediatr Surg 44:1410–1417
Drews JD, Onwuka EA, Fisher JG, Hungtinton JT, Dutkiewicz M, Nogalska A, Nwomeh BC (2019) Complications after proctocolectomy and ileal pouch-anal anastomosis in pediatric patients: a systematic review. J Pediatr Surg 54:1331–1339
Dharmarjah R, Dasgupta M, Simpson P, Noe J (2016) Predictors of pouchitis after ileal pouch-anal anastomosis in children. J Pediatr Gastroenterol Nutr 63:58–62
Kennedy RD, Zarroung AE, Moir CR et al (2014) Ileal pouch anal anastamosis in pediatric familial adenomatous polyposis: a 24 year review of operative technique and patient outcome. J Pediatr Surg 49:1409–1412
Treynor JR, McKenna NP, Potter DD, Moir CR, Klikner DB (2019) The effect of divertion on readmission following ilea pouch-anal anastamosis. J Pediatr Surg. https://doi.org/10.1016/j.jpedsurg.2019.11.002
Tudyka VN, Clark SK (2012) Surgical treatment of familial adenomatous polyposis. Ann Gastroenterol 25:201–206
Tilney HS, Constantinides V, Ioannides AS, Tekkis PP, Darzi AW, Haddad MJ (2006) Pouch-anal aanstamosis vs straight ileoanal anastomosis in pediatric patients: a meta-analysis. J Pediatr Surg 41:1799–1808
Durno C, Sherman P, Harris K et al (1998) Outcome after ileoanal anastomosis in pediatric patients with ulcerative colitis. J Pediatr Gastroenterol Nutr 27:501–507
Lovegrove R, Constantinides V, Heriot A et al (2006) A comparison of handsewn versus stapled ileal pouch anal anastomosis (IPAA) following proctocolectomy: a meta-analysis of 4183 patients. Ann Surg 244:18–26
Tajika M, Nakamura T, Nakahara O et al (2009) Prevalence of adeno- mas and carcinomas in the ileal pouch after proctocolectomy in patients with familial adenomatous polyposis. J Gastrointest Surg 13:1266–1273
Parc YR, Olschwang S, Desaint B, Schmitt G, Parc RG, Tiret E (2001) Familial adenomatous polyposis: prevalence of adenomas in the ileal pouch after restorative proctocolectomy. Ann Surg 233:360–364
Ganschow P, Trauth S, Hinz U, Schaible A, Büchler MW, Kadmon M (2018) Risk factors associated with pouch adenomas in patients with familial adenomatous polyposis. Dis Colon Rectum 61:1096–1101
Maehata Y, Esaki M, Nakamura S, Hirahashi M, Ueki T, Iida M, Kitazono T, Matsumoto T (2015) Risk of cancer in the rectal remnant after ileorectal anastomosis in patients with familial adenomatous polyposis: single center experience. Dig Endosc 27(4):471–478
Potter DD, Moir CR, Day CN et al (2019) Fertility and sexual function in women following pediatric ileal pouch-anal anastomosis. J Pediatr Surg. https://doi.org/10.1016/j.jpedsurg.2019.09.051
McKenna NP et al (2019) Laparoscopic approach was not associated with increased major complication and was associated with lower odds of minor complication and shorter length of stay McKenna NP et al. J Pediatr Surg 54:112–117
Traynor MD Jr, McKenna NP, Habermann EB, Yonkus J, Moir CR, Potter DD Jr, Ishitani MB, Klinkner DB (2019) Utilization of maneuvers to increase mesenteric length employed in children undergoing ileal pouch-anal anastomosis. J Laparoendosc Adv Surg Tech A. https://doi.org/10.1089/lap.2019.0124
Kauffman JD, Snyder CW, Danielson PD, Chandler NM (2019) 30-day outcomes of laparoscopic versus open total proctocolectomy with ileoanal anastomosis in children and young adults: a combined analysis of the national surgical quality improvement project pediatric and adult databases. J Laparoendosc Adv Surg Tech A 29:402–408
Hassan I, Chua HK, Wolff BG, Donnelly SF, Dozois RR, Larson DR, Schleck CD, Nelson H (2005) Quality of life after ileal pouch-anal anastomosis and ileorectal anastomosis in patients with familial adenomatous polyposis. Dis Colon Rectum 48:2032–2037
Ardoino I, Signoroni S, Malvicini E, Ricci MT, Biganzoli EM, Bertario L, Occhionorelli S, Vitellaro M (2019) Long-term survival between total colectomy versus proctocolectomy in patients with FAP: a registry-based, observational cohort study. Tumori. https://doi.org/10.1177/0300891619868019
Acknowledgements
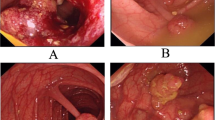
The author would like to thank Associate Professor Semire Serin Ezer for sharing the first and fourth figures from her personal archive.
Funding
The study is review article and there is no funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Author has no conflict of interest.
Studies with human participants or animals
This article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Soyer, T. Polypoid disease of colon in children. Pediatr Surg Int 36, 447–455 (2020). https://doi.org/10.1007/s00383-020-04621-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-020-04621-3