Abstract
Purpose
Excessive narcotization in pediatric surgical patients has not been well characterized. This report describes the use of postoperative naloxone in pediatric patients.
Methods
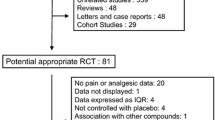
Pediatric surgical patients from January 1, 2010, through June 30, 2016, who underwent general anesthesia and received naloxone within 48 h postoperatively were identified and matched 1:1 with controls by age, sex, and procedure. Cases and controls underwent retrospective chart review.
Results
Forty-seven patients received naloxone, with a rate of 2.0 (95% CI 1.5–2.7) per 1000 anesthetics. Indications were respiratory depression (n = 19), facilitating extubation (n = 15), and reversing sedation (n = 13), and 44 cases received naloxone in a monitored environment. The median (interquartile range) naloxone dose was 4.0 (2.0–23.5) mcg/kg, and five patients (11%) later required subsequent naloxone treatments. Their characteristics were similar to controls, including opioid medications, except cases that had signs of respiratory depression before naloxone administration. The outcomes were similar, although more cases were admitted to the intensive care unit before naloxone administration. One patient died 13 days postoperatively of unrelated causes.
Conclusion
Postoperative naloxone administration in pediatric patients is rare. The observation that most administrations occurred in a monitored setting implies that at-risk patients had been appropriately identified and kept under closer surveillance.

Similar content being viewed by others
Abbreviations
- ICU:
-
Intensive care unit
- IQR:
-
Interquartile range
- ME:
-
Morphine equivalents
- PACU:
-
Postanesthesia care unit
References
Sun Z, Sessler DI, Dalton JE, Devereaux PJ, Shahinyan A, Naylor AJ et al (2015) Postoperative hypoxemia is common and persistent: a prospective blinded observational study. Anesth Analg 121(3):709–715
Lee LA, Caplan RA, Stephens LS, Posner KL, Terman GW, Voepel-Lewis T et al (2015) Postoperative opioid-induced respiratory depression: a closed claims analysis. Anesthesiology 122(3):659–665
Cashman JN, Dolin SJ (2004) Respiratory and haemodynamic effects of acute postoperative pain management: evidence from published data. Br J Anaesth 93(2):212–223
Weingarten TN, Herasevich V, McGlinch MC, Beatty NC, Christensen ED, Hannifan SK et al (2015) Predictors of delayed postoperative respiratory depression assessed from naloxone administration. Anesth Analg 121(2):422–429
Weingarten TN, Warner LL, Sprung J (2017) Timing of postoperative respiratory emergencies: when do they really occur? Curr Opin Anaesthesiol 30(1):156–162
Cheon EC, Palac HL, Paik KH, Hajduk J, De Oliveira GS, Jagannathan N et al (2016) Unplanned, postoperative intubation in pediatric surgical patients: development and validation of a multivariable prediction model. Anesthesiology 125(5):914–928
Chidambaran V, Olbrecht V, Hossain M, Sadhasivam S, Rose J, Meyer MJ (2014) Risk predictors of opioid-induced critical respiratory events in children: naloxone use as a quality measure of opioid safety. Pain Med 15(12):2139–2149
Jay MA, Thomas BM, Nandi R, Howard RF (2017) Higher risk of opioid-induced respiratory depression in children with neurodevelopmental disability: a retrospective cohort study of 12,904 patients. Br J Anaesth 118(2):239–246
Jacox A, Carr DB, Payne R, Berde CB, Breitbart W, Cain JM et al (1994) Management of cancer pain. In: Clinical practice guideline no. 9. AHCPR Publication No. 94-0592. Agency for Health Care Policy and Research, US Department of Health and Human Services, Public Health Service, Rockville
American Pain Society (1999) Principles of analgesic use in the treatment of acute pain and cancer pain, 4th edn. American Pain Society, Glenview
Hegenbarth MA; American Academy of Pediatrics Committee on Drugs(2008) Preparing for pediatric emergencies: drugs to consider. Pediatrics 121(2):433–443
Acknowledgements
Source of funding: This project, including the statistical analyses, was supported by the Department of Anesthesiology and Perioperative Medicine, Mayo Clinic College of Medicine, Mayo Clinic, Rochester, Minnesota. Role of the funding source: the funding source had no role in data collection or interpretation; in the writing of the manuscript; or in the decision to submit it for publication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Weingarten currently serves as a consultant to Medtronic in the role as Chairman of the Clinical Endpoint Committee for the Prodigy Trial. Dr. Weingarten has received unrestricted investigator-initiated grants from Merck for research unrelated to the current study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Donempudi, V.K., Sprung, J. & Weingarten, T.N. Pediatric patients receiving naloxone within 48 h of anesthesia: a case–control study. Pediatr Surg Int 34, 335–341 (2018). https://doi.org/10.1007/s00383-017-4212-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-017-4212-2