Abstract
Purpose
To the best of our knowledge, this is the first study conducted in Tunisia on the neurosurgical management of child cranial trauma. The objectives of the present work were to identify the causes of pediatric head injuries, explore epidemiological and clinical specificities, and analyze the short- and long-term postoperative evolution.
Methods
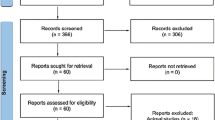
A retrospective review was conducted on one hundred children with head injuries over a five-year period at one of the largest neurosurgery departments in Tunisia. The collected data encompassed demographic information, clinical presentation features, neuroimaging characteristics, surgical management, complications, and outcomes.
Results
Over a five-year period, we have found 118 children who have undergone surgery, representing an annual incidence of twenty-four children per year. The average age was 10 years. Falls emerged as the primary cause of childhood head injuries in our series, followed by road traffic accidents. The most frequently encountered initial sign was the loss of consciousness (52%), followed by headaches (28%), vomiting (25%), and seizures (8%). The average time between the accident and admission to the operating unit was 10 h. Various neurosurgeries were performed, with the evacuation of an epidural hematoma being the most common procedure. At a median follow-up of 24 months, the outcomes were favorable in 88% of cases.
Conclusion
The main prognostic factors for head trauma in children included age, circumstances of the accident, association with polytrauma, the initial Glasgow Coma Scale, the nature of the initial cerebral lesions, and the timeliness and quality of initial management.
Similar content being viewed by others
References
Primalani NK et al (2022) Abusive head injury in the very young: outcomes from a Singapore children’s hospital, Childs Nerv. Syst. ChNS Off. J. Int. Soc. Pediatr. Neurosurg 38(12):2397–2407. https://doi.org/10.1007/s00381-022-05572-x
Narang SK, Fingarson A, Lukefahr J (2020) Council, on child abuse, and neglect (Apr. 2020) Abusive Head Trauma in infants and children. Pediatrics 145(4):e20200203. https://doi.org/10.1542/peds.2020-0203
Duhaime A-C, Christian CW (2019) Abusive head trauma: evidence, obfuscation, and informed management, J. Neurosurg. Pediatr 24(5):481–488. https://doi.org/10.3171/2019.7.PEDS18394
Cheong TM et al (2022) Decompressive surgery in abusive head injury: Experience from a Singapore children’s hospital and a review of literature, Childs Nerv. Syst. ChNS Off. J. Int. Soc. Pediatr. Neurosurg 38(12):2437–2444. https://doi.org/10.1007/s00381-022-05669-3
Bandyopadhyay S et al (2021) Traumatic Brain Injury–Related Pediatric Mortality and Morbidity in Low- and Middle-Income countries: a systematic review. World Neurosurg 153:109–130e. https://doi.org/10.1016/j.wneu.2021.06.077
Bedry T, Tadele H (2020) Pattern and Outcome of Pediatric Traumatic Brain Injury at Hawassa University Comprehensive Specialized Hospital, Southern Ethiopia: Observational Cross-Sectional Study, Emerg. Med. Int 2020:1–9. https://doi.org/10.1155/2020/1965231
Rabiu TB, Ogundipe H (2022) Profile of Pediatric Traumatic Brain Injury in South-West Nigeria. World Neurosurg 166:e711–e720. https://doi.org/10.1016/j.wneu.2022.07.078
Barcenas LK et al (2022) The epidemiology of pediatric traumatic brain injury presenting at a referral center in Moshi, Tanzania. PLoS ONE 17(10):e0273991. https://doi.org/10.1371/journal.pone.0273991
Raees M et al (2022) An exploratory assessment of the management of pediatric traumatic brain injury in three centers in Africa. Front Pediatr 10:936150. https://doi.org/10.3389/fped.2022.936150
Davis T, Ings A (2015) National Institute of Health and Care Excellence Head injury: triage, assessment, investigation and early management of head injury in children, young people and adults (NICE guideline CG 176), Arch. Dis. Child. Educ. Pract. Educ 100(2):97–100. https://doi.org/10.1136/archdischild-2014-306797
Di Rocco F, Beuriat PA, Mottolese C, Beuriat AS, Fanton L, Vinchon M (2022) Non-accidental head injury of infants: legal implications for the pediatric neurosurgeon, Childs Nerv. Syst. ChNS Off. J. Int. Soc. Pediatr. Neurosurg 38(12):2295–2299. https://doi.org/10.1007/s00381-022-05722-1
Ryan E et al (2020) Paediatric Head Injury and Traumatic Brain Injury, Ir. Med. J 113(6):94
Hung K-L (2020) Pediatric abusive Head Trauma. Biomed J 43(3):240–250. https://doi.org/10.1016/j.bj.2020.03.008
Schunk JE, Schutzman SA (2012) Pediatric head injury. Pediatr Rev 33(9):398–410 quiz 410–411. https://doi.org/10.1542/pir.33-9-398
Raza HF, Archambault É, Pépin K, Lord A, Frappier J-Y (2022) Traumatic head injury due to child maltreatment: epidemiology, cost analysis, and impact of prevention, Childs Nerv. Syst. ChNS Off. J. Int. Soc. Pediatr. Neurosurg 38(12):2281–2287. https://doi.org/10.1007/s00381-022-05560-1
Lui A, Kumar KK, Grant GA (2022) Management of severe traumatic brain Injury in Pediatric patients. Front Toxicol 4:910972. https://doi.org/10.3389/ftox.2022.910972
Murray GD et al (1999) The European Brain Injury Consortium Survey of Head Injuries, Acta Neurochir. (Wien) 141(3):223–236. https://doi.org/10.1007/s007010050292
Kochanek PM et al (2019) Guidelines for the management of Pediatric severe traumatic brain Injury, Third Edition: update of the Brain Trauma Foundation Guidelines. Pediatr Crit Care Med 20:S1–S82. https://doi.org/10.1097/PCC.0000000000001735
Chesnut RM et al (2012) A Trial of Intracranial-Pressure Monitoring in Traumatic Brain Injury, N. Engl. J. Med 367(26):2471–2481. https://doi.org/10.1056/NEJMoa1207363
Kochanek PM et al (2019) Guidelines for the Management of Pediatric Severe Traumatic Brain Injury, Third Edition: Update of the Brain Trauma Foundation Guidelines, Executive Summary, Neurosurgery 84(6):1169–1178. https://doi.org/10.1093/neuros/nyz051
Bramwell KJ, Haizlip J, Pribble C, VanDerHeyden TC, Witte M (2006) The Effect of Etomidate on Intracranial Pressure and Systemic Blood Pressure in Pediatric Patients with Severe Traumatic Brain Injury:, Pediatr. Emerg. Care 22(2):90–93. https://doi.org/10.1097/01.pec.0000199563.64264.3a
Carney N et al (2017) Guidelines for the Management of Severe Traumatic Brain Injury, Fourth Edition, Neurosurgery 80(1):6–15. https://doi.org/10.1227/NEU.0000000000001432
Funding
No funds, grants, or other support was received.
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Financial interests
The authors have no relevant financial or non-financial interests to disclose.
Competing interests
The authors declare no competing interests.
Patients consent
The patients and/or their family consented to participate and publish their clinical data.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Trifa, A., Rkhami, M., Maamri, K. et al. Pediatric head injuries: particularities and neurosurgical experience in a lower-middle income country. Childs Nerv Syst 40, 1193–1198 (2024). https://doi.org/10.1007/s00381-023-06271-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-023-06271-x