Abstract
Introduction
Analgesia Nociception Index (ANI) as a monitor of peri-operative nociception-anti-nociception balance has not been studied in paediatric neurosurgery. The objectives were to study the correlation between ANI (Mdoloris Education system) and revised FLACC (r-FLACC) score for the prediction of acute postoperative pain in paediatric population undergoing elective craniotomies and to compare the changes in ANI values with heart rate (HR), mean arterial pressure (MAP) and surgical plethysmographic index (SPI) during various time points of intraoperative noxious stimulation and before and after opioid administration.
Methods
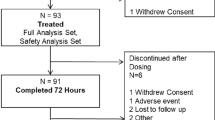
This prospective observational pilot study included 14 patients between 2 and 12 years of age undergoing elective craniotomies. HR, MAP, SPI, ANI instantaneous (ANIi) and ANI mean (ANIm) values were recorded intraoperatively and before and after opioid administration. Postoperatively HR, MAP, ANIi and ANIm, and pain scores (r-FLACC scale) were recorded.
Results
There was a statistically significant negative correlation between ANIi and ANIm with r-FLACC during the time course of PACU stay (r = − 0.89, p < 0.001 and r = − 0.88 and p < 0.001 respectively). Intraoperatively, in patients with ANIi values < 50, with additional fentanyl administration, there was an increasing trend in values beyond 50, which was statistically significant (p < 0.05) at 3, 4, 5 and 10 min. The trend in changes of SPI after opioid administration was not found to be significant for patients irrespective of the baseline SPI values.
Conclusion
The ANI is a reliable tool for objective assessment of acute postoperative pain as assessed by r-FLACC in children undergoing craniotomies for intracranial lesions. It may be used as a guide to nociception-antinociception balance during the peri-operative period in this population.


Similar content being viewed by others
References
Suksompong S, Chaikittisilpa N, Rutchadawong T, Chankaew E, von Bormann B (2016) Pain after major craniotomy in a university hospital: a prospective cohort study. J Med Assoc Thail 99(5):539–548
Tsaousi GG, Logan SW, Bilotta F (2017) Postoperative pain control following craniotomy: a systematic review of recent clinical literature. Pain Pract 17:968–981. https://doi.org/10.1111/papr.12548
Teo JH, Palmer GM, Davidson AJ (2011) Post-craniotomy pain in a paediatric population. Anaesth Intensive Care 39(1):89–94. https://doi.org/10.1177/0310057X1103900115
Xing F, An LX, Xue FS et al (2019) Postoperative analgesia for pediatric craniotomy patients: a randomized controlled trial. BMC Anesthesiol 19:53. https://doi.org/10.1186/s12871-019-0722-x
Bronco A, Pietrini D, Lamperti M, Somaini M, Tosi F, del Lungo LM et al (2014) Incidence of pain after craniotomy in children. Pediatr Anesth 24:781–787. https://doi.org/10.1111/pan.12351
Maxwell LG, Buckley GM, Kudchadkar SR, Ely E, Stebbins EL, Dube C, Morad A, Jastaniah EA, Sethna NF, Yaster M (2014) Pain management following major intracranial surgery in pediatric patients: a prospective cohort study in three academic children’s hospitals. Paediatr Anaesth 24(11):1132–1140. https://doi.org/10.1111/pan.12489
Kommula LK, Bansal S, Umamaheswara Rao GS (2019) Analgesia nociception index monitoring during supratentorial craniotomy. J Neurosurg Anesthesiol 31:57–61. https://doi.org/10.1097/ANA.0000000000000464
Theerth KA, Sriganesh K, Chakrabarti D, Reddy KR, Rao GS (2019) Analgesia nociception index and hemodynamic changes during skull pin application for supratentorial craniotomies in patients receiving scalp block versus pin-site infiltration: a randomized controlled trial. Saudi J Anaesth 13(4):306–311. https://doi.org/10.4103/sja.SJA_812_18
Silvetti MS, Drago F, Ragonese P (2001) Heart rate variability in healthy children and adolescents is partially related to age and gender. Int J Cardiol 81:169–174. https://doi.org/10.1016/s0167-5273(01)00537-x
Bobkowski W, Stefaniak ME, Krauze T, Gendera K, Wykretowicz A, Piskorski J, Guzik P (2017) Measures of heart rate variability in 24-h ECGs depend on age but not gender of healthy children. Front Physiol 8:311. https://doi.org/10.3389/fphys.2017.00311
Logier R, Jeanne M, De Jonckheere J, Dassonneville A, Delecroix M, Tavernier B (2010) PhysioDoloris: a monitoring device for analgesia / nociception balance evaluation using heart rate variability analysis. Annu Int Conf IEEE Eng Med Biol Soc 1194–7. https://doi.org/10.1109/IEMBS.2010.5625971
Ledowski T, Sommerfield D, Slevin L, Conrad J, von Ungern-Sternberg BS (2017) Surgical pleth index: prediction of postoperative pain in children? Br J Anaesth 119(5):979–983. https://doi.org/10.1093/bja/aex300
Pedersen LK, Rahbek O, Nikolajsen L, Møller-Madsen B (2015) The revised FLACC score: reliability and validation for pain assessment in children with cerebral palsy. Scand J Pain 9(1):57–61. https://doi.org/10.1016/j.sjpain.2015.06.007
Malviya S, Voepel-Lewis T, Burke C, Merkel S, Tait AR (2006) The revised FLACC observational pain tool: improved reliability and validity for pain assessment in children with cognitive impairment. Paediatr Anaesth 16(3):258–265. https://doi.org/10.1111/j.1460-9592.2005.01773.x
Aldrete JA (1995) The post-anaesthesia recovery score revisited. J Clin Anaesth 7:89–91. https://doi.org/10.1016/0952-8180(94)00001-K
R Core Team (2018) R: a language and environment for statistical computing R Foundation for Statistical Computing. Vienna, Austria. https://www.R-project.org/
Kuznetsova A, Brockhoff PB, Christensen RHB (2017) lmerTest package: tests in linear mixed effects models. J Stat Softw 82(13):1–26. https://doi.org/10.18637/jss.v082.i13
Wickham H (2016) ggplot2: elegant graphics for data analysis (Use R!). 2nd edn. New york: Springer-Verlag, pp 147–168. https://doi.org/10.1007/978-3-319-24277-4
Baptiste Auguie (2017) gridExtra: miscellaneous functions for “grid” graphics R package version 2.3. https://CRAN.R-project.org/package=gridExtra
Julien-Marsollier F, Rachdi K, Caballero MJ, Ayanmanesh F, Vacher T, Horlin AL, Skhiri A, Brasher C, Michelet D, Dahmani S (2018) Evaluation of the analgesia nociception index for monitoring intraoperative analgesia in children. Br J Anaesth 121(2):462–468. https://doi.org/10.1016/j.bja.2018.03.034
Ledowski T, Tiong WS, Lee C, Wong B, Fiori T, Parker N (2013) Analgesia nociception index: evaluation as a new parameter for acute postoperative pain. BJA: Br J Anaesth 111(4):627–9. https://doi.org/10.1093/bja/aet111
Lee JH, Choi BM, Jung YR, Lee YH, Bang JY, Noh GJ (2020) Evaluation of Surgical Pleth Index and Analgesia Nociception Index as surrogate pain measures in conscious postoperative patients: an observational study. J Clin Monit Comput 34(5):1087–1093. https://doi.org/10.1007/s10877-019-00399-5
Gall O, Champigneulle B, Schweitzer B, Deram T, Maupain O, Montmayeur Verchere J, Orliaguet G (2015) Postoperative pain assessment in children: a pilot study of the usefulness of the analgesia nociception index. Br J Anaesth 115(6):890–895. https://doi.org/10.1093/bja/aev361
Abdullayev R, Uludag O, Celik B (2019) Analgesia Nociception Index: assessment of acute postoperative pain. Braz J Anesthesiol 69(4):396–402. https://doi.org/10.1016/j.bjan.2019.01.003
Boselli E, Bouvet L, Bégou G, Dabouz R, Davidson J, Deloste JY, Rahali N, Zadam A, Allaouchiche B (2014) Prediction of immediate postoperative pain using the analgesia/nociception index: a prospective observational study. Br J Anaesth 112(4):715–721. https://doi.org/10.1093/bja/aet407
Weber F, Geerts NJE, Roeleveld HG, Warmenhoven AT, Liebrand CA (2018) The predictive value of the heart rate variability-derived Analgesia Nociception Index in children anaesthetized with sevoflurane: an observational pilot study. Eur J Pain 22(9):1597–1605. https://doi.org/10.1002/ejp.1242
Park JH, Lim BG, Kim H, Lee IO, Kong MH, Kim NS (2015) Comparison of Surgical Pleth Index–guided analgesia with conventional analgesia practices in children: a randomized controlled trial. Anesthesiology 122:1280–1287. https://doi.org/10.1097/ALN.0000000000000650
Chowdhury T, Garg R, Sheshadri V, Venkatraghavan L, Bergese SD, Cappellani RB, Schaller B (2017) Perioperative factors contributing the post-craniotomy pain: a synthesis of concepts. Front Med (Lausanne) 4:23. https://doi.org/10.3389/fmed.2017.00023
Author information
Authors and Affiliations
Contributions
P. S.: methodology, data collection, writing—original draft, formal analysis, literature search; K. N. G. and K. R. S.: conceptualisation, methodology, writing—review and editing, supervision, project administration; D. C.: software, formal analysis, writing—review and editing; N. S.: data analysis, writing—review and editing; K. S.: data collection, literature search.
Corresponding author
Ethics declarations
Ethics approval
The study was approved by Institute Ethics Committee of the National Institute of Mental Health and Neurosciences and appropriate consent obtained before recruiting.
Conflict of interest
None to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
381_2023_5905_MOESM1_ESM.docx
Supplementary file1 (DOCX 14 KB) Table S1: Descriptive statistics (mean ± standard deviation) of all the study variables across intra-operative study time points. ANIi = Analgesia nociception index instantaneous; ANIm = Analgesia nociception index mean; HR = Hear Rate; SBP = Systolic blood pressure; DBP = Diastolic blood pressure; MAP = Mean arterial pressure; SPI = Surgical plethysmographic index; T15,T30..T180 = Time in minutes after durotomy.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sharma, P., Shwethashri, K.R., Chakrabarti, D. et al. Analgesia Nociception Index (ANI) as a monitor of peri-operative nociception-antinociception balance in paediatric craniotomies: a prospective observational study. Childs Nerv Syst 39, 2169–2176 (2023). https://doi.org/10.1007/s00381-023-05905-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-023-05905-4