Abstract
Introduction
There is no clear consensus regarding the technique of surgical revascularization for moyamoya disease and syndrome (MMD/MMS) in the pediatric population. Previous meta-analyses have attempted to address this gap in literature but with methodological limitations that affect the reliability of their pooled estimates. This meta-analysis aimed to report an accurate and transparent comparison between studies of indirect (IB), direct (DB), and combined bypasses (CB) in pediatric patients with MMD/MMS.
Methods
In accordance with PRISMA guidelines, systematic searches of Medline, Embase, and Cochrane Central were undertaken from database inception to 7 October 2022. Perioperative adverse events were the primary outcome measure. Secondary outcomes were rates of long-term revascularization, stroke recurrence, morbidity, and mortality.
Results
Thirty-seven studies reporting 2460 patients and 4432 hemispheres were included in the meta-analysis. The overall pooled mean age was 8.6 years (95% CI: 7.7; 9.5), and 45.0% were male. Pooled proportions of perioperative adverse events were similar between the DB/CB and IB groups except for wound complication which was higher in the former group (RR = 2.54 (95% CI: 1.82; 3.55)). Proportions of post-surgical Matsushima Grade A/B revascularization favored DB/CB over IB (RR = 1.12 (95% CI 1.02; 1.24)). There was no significant difference in stroke recurrence, morbidity, and mortality. After meta-regression analysis, year of publication and age were significant predictors of outcomes.
Conclusions
IB, DB/CB are relatively effective and safe revascularization options for pediatric MMD/MMS. Low-quality GRADE evidence suggests that DB/CB was associated with better long-term angiographic revascularization outcomes when compared with IB, although this did not translate to long-term stroke and mortality benefits.
Similar content being viewed by others
Introduction
Moyamoya disease (MMD) or syndrome (MMS) refers to an abnormal progressive steno-occlusive disorder at the distal internal carotid artery (ICA) [1]. Patients are at high risk for transient ischemic stroke (TIA) or stroke. It is asserted that surgical revascularization provides better outcomes for these patients than medical treatment alone. In pediatric patients, the goal of surgery is to augment cerebral blood flow and reduce the risk of ischemic events [2].
Revascularization techniques can be direct, indirect, or combined. Direct bypass (DB) is accomplished by anastomosing extracranial vessels to intracranial vessels (EC-IC bypass), most often the superficial temporal artery (STA) to the middle cerebral artery (MCA) (STA-MCA bypass) [3, 4]. Indirect bypass (IB) has many variations but is generally accomplished by incorporating well-vascularized tissue usually from external carotid artery sources onto the surface of the brain to promote angiogenesis and neovascularization, rather than by direct anastomosis [5,6,7,8,9]. Unlike DB, IB begins to alter the cerebral blood flow only after angiogenesis has taken place, the timescale for which is unpredictable [3]. A combined bypass (CB) utilizes both techniques simultaneously to maximize the effect of short-term and long-term revascularization [3].
There is currently no definite consensus regarding the technique of surgical revascularization in pediatric MMD/MMS [1, 2]. Existing meta-analyses have elegantly attempted to address this controversy in pediatric patients [10, 11]. However, in these studies, repeated patient populations from the same institutions within overlapping time intervals were included [10, 11]. This methodological flaw overstates sample size and number of events, leading to an artificially exaggerated precision in their pooled estimate [12]. In addition, several included primary studies in these meta-analyses had not distinguished outcomes based on the type of bypass nor specifically for children, and hence it was unclear how these meta-analyses were able to distinguish between the techniques or population. This meta-analysis aimed to mitigate against previous methodological limitations and report an accurate and transparent comparison between studies of IB, DB, and CB in pediatric patients with MMD/MMS.
Methods
This review was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [13]. The protocol was registered on the PROSPERO international prospective register (CRD42022365524).
Outcomes
The primary outcome included any reported perioperative adverse events within 30 days after bypass surgery. This included wound complications, seizures, cerebrospinal fluid (CSF) leak extra-axial hemorrhage, TIA, stroke, and death.
Secondary outcomes included modified Rankin score (mRS), long-term stroke, mortality risk, and degree of angiographic revascularization at last follow-up. The degree of revascularization was graded according to Matsushima’s classification of the proportion of arterial territory (Grade A > 2/3, Grade B = 1/3 to 2/3, Grade C < 1/3) [3].
When angiographic assessment in the primary studies was graded according to a 3-grade classification (poor, moderate, or good), or 4-grade classification (none, poor, medium, or extensive) [14], we classified “good” and “extensive” as Grade A, “moderate” and “medium” as Grade B, and “poor” or “none” as Grades C.
Search strategy
Searches of three electronic databases were undertaken: Ovid Medline, Ovid Embase, and Cochrane Central Register of Controlled Trials (CENTRAL). Searches were performed in each database from its inception until 7 October 2022. The full search strategy is presented in Supplementary Table 1.
Eligibility criteria
Articles were selected for inclusion if they were a primary interventional or observational study evaluating the effectiveness and safety of revascularization surgeries in pediatric MMD/MMS. The review included studies on exclusively pediatric patients (< 18 years). Studies that had evaluated both pediatric and adult MMD/MMS but reported outcomes specific to the pediatric population were included. Studies that had evaluated various revascularization techniques but reported outcomes specific for the particular technique were included.
The review excluded narrative and systematic reviews, editorials, commentaries, opinion papers, letters, education papers, conference abstracts, protocols, reports, theses, or book chapters as they were unlikely to contain sufficient detail about the effectiveness and safety of both treatments.
Study selection
All titles and abstracts were screened against the pre-defined eligibility criteria developed independently by two reviewers (KSL and JJYZ). A full list of inclusion and exclusion criteria of studies is stated in Supplementary Table 2. Disagreements were resolved by discussion, and where agreement could not be reached, the senior reviewer assisted with decision-making (AHDS). Agreement among the reviewers was evaluated using Cohen’s kappa [15].
The institutions and data collection period were scrutinized to avoid multiple counting. In the event of multiple publications analyzing the same cohort of patients/hemispheres, the publication that reported the largest patient data with the most relevant outcomes was used for evaluation.
Data extraction
A pro forma was developed and piloted to extract data on the following variables to ensure standardization and consistency in this process: (1) study details; (2) study design; (3) participant demographics; (4) country, institution, and data collection period; (5) selection criteria; (6) treatment and control; (7) indication for treatment; and (8) results.
Risk of bias assessment
The quality of included studies was assessed using the Joanna Briggs Institute (JBI) checklist for cohort studies and case series [16]. KSL and JJYZ assessed the quality of all included studies and discussed discrepancies until consensus was reached.
Statistical analysis
Meta-analyses of primary end points were performed assuming the random effects model to account for heterogeneity within and between individual studies [16].
We analyzed both DB and CB as a single cohort compared with IB. The rationale is that in CB, patients undergo a direct and an indirect component of the revascularization in the same setting. The direct component would afford an immediate increase in cerebral perfusion, while the indirect collateralization would take months to a year to form [3]. As reported denominators were heterogenous, analyses by both patients and hemispheres were performed whenever possible. To obtain risk ratios (RRs) from reported binary outcomes between DB/CB and IB, a pairwise meta-analysis was conducted using the Mantel–Haenszel method, using the Paule-Mandel estimator. Overall pooled proportions were computed using the generalized linear mix model (GLMM) [16]. Knapp-Hartung adjustments were used to calculate the 95% confidence intervals (CIs) around the pooled effect to reduce the risk of a Type 1 error.
For the pooling of means of numerical variables, we computed missing means and standard deviations (SDs) from medians, ranges, and interquartile ranges (IQRs) using the methods proposed by Hozo et al. and Wan et al. [17, 18].
The I2 statistic was used to present inter-study heterogeneity, where I2 ≤ 30%, between 30 and 50%, between 50 and 75%, and ≥ 75% were considered to indicate low, moderate, substantial, and considerable heterogeneity, respectively [16]. P values for the I2 statistic were derived from the chi-squared distribution of Cochran’s Q test.
Summary-level meta-regression was performed using the mixed-effects model after computation of the SD of Freeman-Tukey double arcsine transformed proportions, to identify predictors of perioperative TIA, stroke, long-term revascularization, stroke, and mortality. Predictors were year of publication, age, presence of MMS, presence of sickle cell disease (SCD), neurofibromatosis (NF1), and Down syndrome, in accordance with the literature [5, 7, 19, 20]. Summary-level meta-regression was additionally performed using a mixed-effect meta-analysis model by the GLMM method, as a sensitivity analysis to examine the robustness of the former approach.
The publication bias of studies was assessed visually using funnel plots and quantitatively using Egger’s regression test [16]. The GRADE approach was used to evaluate the quality of evidence for each outcome.
All statistical analyses were performed using R software version 4.2.1 (R Foundation for Statistical Computing, 2022), with the package meta. P values less than 0.05 were considered statistically significant.
Results
Study selection and characteristics
As expected, a substantial number of studies were excluded because they had reported data from the same cohort of patients/hemispheres across overlapping time periods. These were commonly from large high-volume institutions such as Beijing Tiantan Hospital [21,22,23,24,25], Boston Children’s Hospital [5,6,7,8,9, 20, 26,27,28,29,30], and Seoul National University Children’s Hospital [31,32,33,34]. Consequently, only one publication that reported the largest patient data with the most relevant outcomes was included in our analysis.
Thirty-seven studies met the eligibility criteria for inclusion in our systematic review and meta-analysis (Fig. 1) [2,3,4, 19, 35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67]. The reliability of the study selection was substantial at both the title and abstract (Cohen’s κ = 0.86) and the full-text review stages (Cohen’s κ = 1.00) [15].
All included studies were retrospective observational studies—eight cohort studies and 29 case series. A total of 37 studies reporting 2460 pediatric patients were included. Only 36 studies had reported the number of hemispheres, and the total hemisphere count was 4432. Thirty-two studies reported outcomes of IB. Of these, 31 studies reported the number of hemispheres in the IB group (3524) and all 34 reported the number of patients (2227). Seventeen studies reported outcomes of DB/CB. All 17 studies reported the number of hemispheres in the DB/CB group (905) whilst only 10 reported the number of patients (358). Eleven studies compared outcomes between the IB and DB/CB groups (Table 1).
Risk of bias assessment using the JBI checklist for cohort studies and case series are reported in Supplementary Tables S3 and S4.
Baseline characteristics of patients
The gender of the patients was reported in 25 studies in a total of 1731 patients—45.0% male and 55.0% female. The mean and SD of their age were reported or imputable in 29 studies in a total of 2204 patients. Overall pooled mean age was 8.6 years (95% CI: 7.7; 9.5, I2 = 95.3% [p < 0.001]). In total, 308 patients had MMS. The pooled prevalence of MMS within the included population was 21.7% (95% CI: 1.1–86.9%, I2 = 54.2 [p < 0.001]). The number of patients with associated SCD, NF1, Down syndrome, cranial radiation, congenital cardiac abnormality, renal artery stenosis, ACTA2 mutation, and Alagille syndrome were 131 (42.5%), 47 (15.3%), 40 (13.0%), 24 (7.8%), 18 (5.8%), 6 (1.9%), 3 (1.0%), and 3 (1.0%), respectively.
Perioperative adverse events
Table 2 presents a detailed summary of the pooled outcomes in each group and Table 3 presents a direct comparison of outcomes between the two groups. Table 4 summarizes the predictors of these outcomes identified on meta-regression.
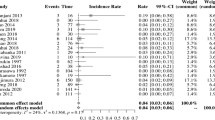
Overall pooled rates of perioperative seizures by hemispheres in the IB and DB/CB groups were 0.84% (95% CI: 0.16; 4.26, I2 = 79.0 [p < 0.001]) and 0.00% (95% CI: 0.00; 1.00, I2 = 0.0 [p = 1.000]) respectively. Two studies of 582 hemispheres directly compared rates of perioperative seizures between the two groups. Perioperative seizure rate was comparable between IB and DB/CB (RR = 0.25 (95% CI: 0.00; 2022.03), I2 = 0.0 [p = 0.514]). Overall pooled rates of perioperative wound complications by hemispheres in the IB and DB/CB groups were 1.18% (95% CI: 0.31; 4.46, I2 = 54.1 [p = 0.033]) and 2.26% (95% CI: 0.46; 10.36, I2 = 0.0 [p = 0.584]), respectively. Overall pooled rates of perioperative wound complications by patients in the IB and DB/CB groups were 3.01% (95% CI: 0.61; 13.46, I2 = 41.0 [p = 0.132]) and 3.03% (95% CI: 0.00; 99.99, I2 = 0.0 [p = 1.000]), respectively. Two studies of 582 hemispheres directly compared rates of perioperative wound complications between the two groups. Perioperative wound complications rate was significantly higher in the DB/CB group (RR = 2.54 (95% CI: 1.82; 3.55), I2 = 0.0 [p = 0978]) (Fig. 2a). Overall pooled rates of perioperative CSF leak by hemispheres in the IB and DB/CB groups were 1.00% (95% CI: 0.34; 2.89, I2 = 30.6 [p = 0.184]) and 1.6% (95% CI: 0.00; 99.29, I2 = 0.0 [p = 0.573]), respectively. No direct comparison was available for rates of perioperative CSF leaks.
Overall pooled rates of perioperative TIA by hemispheres in the IB and DB/CB groups were 2.62% (95% CI: 1.14; 5.91, I2 = 67.8 [p < 0.001]) and 7.61% (95% CI: 2.20; 23.15, I2 = 78.8 [p < 0.001]), respectively. Pooled rates of perioperative TIA by patients in the IB and DB/CB groups were 4.52% (95% CI: 1.95; 10.09, I2 = 59.1 [p < 0.001]) and 9.74% (95% CI: 0.35; 76.75, I2 = 82.0 [p = 0.004]), respectively. Five studies of 935 hemispheres directly compared rates of perioperative TIA. Perioperative TIA rate was comparable between IB and DB/CB (RR = 0.64 (95% CI: 0.38; 1.10), I2 = 0.0 [p = 0.786]). Pooled rates of perioperative stroke by hemispheres in the IB and DB/CB groups were 3.19% (95% CI: 1.915.30, I2 = 54.8 [p < 0.001]) and 4.55% (95% CI: 2.04; 9.84, I2 = 53.1 [p = 0.030]), respectively. Two studies directly compared rates of perioperative stroke by hemispheres and patients and showed comparability (RR = 0.25 (95% CI: 0.00; 2022.04), I2 = 0.0 [p = 0.514]) and (RR = 0.72 (95% CI: 0.00; 5682.31), I2 = 0.0 [p = 0.538]), respectively. On meta-regression, age significantly predicted rates of perioperative stroke (p = 0.048) in the IB group (Fig. 3a). Further meta-regression demonstrated age further significantly predicted rates of perioperative TIA (p = 0.005) and perioperative stroke (p < 0.001) in the DC/CB group (Fig. 3b and c, respectively).
Bubble plot for meta-regression of transformed proportion of a perioperative stroke against age in each IB study, b perioperative stroke against age in each DB/CB study, c perioperative TIA against age in each DB/CB study, d mortality against year of publication in each IB study, and e transformed proportion of long-term stroke recurrence against age in each DB/CB study
Pooled rates of perioperative death in the IB and DB/CB groups were 0.00% (95%CI: 0.00; 1.00, I2 = 0.0 [p = 1.000]) and 0.56% (95%CI: 0.00; 6.89, I2 = 0.0 [p = 1.000]), respectively. Direct comparison between the groups showed comparability (RR = 0.96 (95% CI: 0.04; 22.76), I2 = NA [p = NA]).
Revascularization
Angiographical follow-up duration was reported in 9 studies comprising 1150 hemispheres and pooled duration was 4.3 years (95% CI: 2.2; 6.4, I2 = 99.5 [p < 0.001]).
In the IB group, overall pooled rates of hemispheres with Grade A and Grade A/B revascularization were 56.70% (95% CI: 44.32; 68.29, I2 = 83.4 [p < 0.001]) and 85.61% (95% CI: 78.84; 90.48, I2 = 54.3 [p = 0.008]). In DB/CB group, overall pooled rates of hemispheres with Grade A and Grade A/B revascularization were 44.44% (95% CI: 5.75; 91.27, I2 = 0.0 [p = 0.662]) and 95.42% (95% CI: 17.79; 99.95, I2 = 76.8 [p = 0.002]). Three studies of 144 hemispheres directly compared proportions of Grade A and Grade A/B revascularization. No significant difference in the proportion of Grade A was identified (RR = 1.56 (95% CI 0.99; 2.46), I2 = 0.0 [p = 0.707]), but proportions of Grade A/B favored DB/CB over IB (RR = 1.12 (95% CI 1.02; 1.24), I2 = 0.0 [p = 0.878]) (Fig. 2b and c).
Stroke recurrence, dependence, and mortality at last follow up
Clinical follow-up duration was reported in 33 studies with a total of 1992 patients and pooled duration was 6.5 years (95% CI: 4.4; 8.6, I2 = 99.0 [p < 0.001]).
Overall pooled rates of stroke recurrence by hemispheres at last follow-up in the IB and DB/CB groups were 2.34% (95% CI: 0.88; 6.06, I2 = 64.8 [p = 0.004]) and 2.38% (95% CI: 0.39; 13.28, I2 = 0.0 [p = 0.996]), respectively. Overall pooled rates of stroke recurrence by patients at last follow-up in the IB and DB/CB groups were 5.24% (95% CI: 2.97; 9.08, I2 = 51.6 [p = 0.005]) and 5.87% (95% CI: 1.41; 21.41, I2 = 0.0 [p = 0.890]), respectively. On meta-regression, age (p = 0.010) significantly predicted stroke recurrence in the DC/CB group (Fig. 3e).
Overall pooled rates of patients with mRS scores of 0 and 1 at last follow-up in the IB and DB/CB groups were 80.38% (95% CI: 68.67; 88.45, I2 = 81.0 [p < 0.001]) and 87.44% (95% CI: 39.85; 98.65, I2 = 0.0 [p = 0.734]), respectively. Overall pooled rates of mortality at last follow-up in the IB and DB/CB groups were 0.30% (95% CI: 0.08; 1.17, I2 = 0.0 [p = 1.000]) and 0.48% (95% CI: 0.03; 7.18, I2 = 0.0 [p = 1.000]), respectively. The year of publication (p = 0.044) significantly predicted mortality in the IB group (Fig. 3d).
No direct comparison between the two groups was available for rates of stroke recurrence, dependence, or mortality at last follow-up.
Discussion
Summary of findings
This study represents an accurate systematic review and meta-analysis investigating the role of IB, DB, and CB in pediatric patients with MMD/MMS. Both IB and DB/CB procedures had evidence of efficacy and low rates of complication. A comparative meta-analysis demonstrated a significant benefit in favor of DB/CB in terms of long-term angiographic outcomes, when compared with IB; however, wound complication rates were higher following DB/CB. Other outcomes including perioperative seizures, TIA, stroke, and death were similar between the two groups.
In comparison with the literature
The paucity of studies reporting on DB/CB and widespread available studies investigating IB reflects current patterns of practice favoring IB in the pediatric MMD population. While EDAS and EDAMS were among the originally described techniques for IB, new techniques such as pial synangiosis and multiple burr holes have been added to the surgical armamentarium [38]. Existing evidence is insufficient for there to be consensus regarding the optimal IB technique.
This meta-analysis found low rates of perioperative complications in both DB/CB and IB groups. When compared with IB, CB/DB has been purported to be more technically challenging with a greater risk for postoperative complications [49]. However, many studies have demonstrated the feasibility and safety of DB/CB in pediatric patients with satisfactory outcomes [3, 21, 43, 49]. Factors dissuading the use of DB/CB over IB in the pediatric MMD population, include smaller-caliber recipient and donor vessels, the potential for cross-clamp-induced ischemia, and the risk of poor scalp wound healing. This latter concern was substantiated by the findings of this metanalysis [4, 43]. The lower rates of perioperative adverse events, ranging from wound complications to ischemic events, in our meta-analysis may in general, reflect improved patient selection, anesthetic, and peri-operative care with further knowledge into the management of pediatric MMD/MMS [8]. Regardless of the technique, revascularization should in general be performed in high-volume centers as there is evidence to suggest that caseload correlates with improved care and reduced mortality in pediatric patients with MMD/MMS [68].
In a recent meta-analysis comparing the three bypass techniques in adults, Nguyen et al. [69] found that DB/CB conferred benefits in terms of late stroke recurrence versus IB, with no dissimilarities in terms of perioperative outcomes. Notably, while cerebral hyperperfusion is an undesirable complication of DB in adult patients, this phenomenon is much less frequently observed in pediatric patients and so the conclusions of this study should not constitute a reason to avoid DB in children.
This current metanalysis found evidence of improved angiographic outcomes following DB/CB in comparison with IB; a finding in accordance with previous meta-analyses [70]. Jeon et al. [70] additionally demonstrated a significantly lower risk of future stroke events for DB compared with IB in symptomatic adult patients, although we failed to find evidence of this benefit in our pediatric population.
It has been suggested that patients with various subtypes of MMS undergoing revascularization have poorer outcomes when compared with cases with MMD [5, 7, 19, 20, 59]. Lack of stratification between treatment groups did not allow for a comparison of revascularization strategies between these two pathologies in this current analysis. Furthermore, our meta-regression did not identify the presence of MMS nor its specific phenotypes to significantly affect outcomes; however, this is likely be a function of the limited number of studies reporting them, leading to a Type 2 error. Our meta-regression analysis, however, did identify younger age to be associated with a higher risk of peri-operative stroke and TIA complications. This is consistent with the literature which suggests that younger children with MMD/MMS are thought to be the most severely affected and most challenging to treat [8]. This is likely due to their dynamic clinical course, leading to major strokes on presentation, and poor eventual outcomes [8]. Infants with MMD/MMS have severely compromised cerebrovascular reserve and are particularly vulnerable to anesthetic risks [8].
Clinical implications
As this meta-analysis was not able to directly compare IB and DB/CB for all the stated outcomes, we can at best conclude that both techniques are comparable except for the association of greater rates of angiographic revascularization and wound complication rates in DB/CB. Based on this meta-analysis, it would be prudent to counsel families that although DB/CB is associated of greater rates of angiographic revascularization, this does not necessarily translate into any additional benefit over IB in terms of clinical outcomes such perioperative TIA, perioperative stroke, and long-term stroke recurrence. Indeed, certain studies have suggested a poor correlation between Grades A/B revascularization and future stroke risk [59]. DB/CB allows for immediate augmentation of cerebral blood flow and does not rely on the plasticity and angiogenic potential, unlike IB. In contrast to the immediate flow augmentation by the anastomosis of DB/CB, IB generally relies on the slow neovascularization and recruitment of collaterals over time. In this respect, angiographic success with DB/CB is more reflective of technical anastomosis success. Due to this, the interpretation of angiographic outcomes from IB may be limited if the time to collateral angiogenesis is inadequate, which may explain the findings of our study.
Implication on the direction of future research in MMD/MMS intervention
This systematic review underlines the inconsistency in measurement and reporting within the literature of MMD/MMS. Several included primary studies had not distinguished their outcomes based on the type of bypass, patient population (adult vs pediatric), nor whether or not outcomes were reported in terms of hemispheres or patients. Indeed, previous meta-analyses have also encountered this predicament [10, 11]. This inconsistency in reporting impedes data aggregation and outcome comparison across studies, hindering progress in MMD/MMS management. Conducting a randomized controlled trial in pediatric patients with a rare progressive disease such as MMD/MMS is near impossible due to ethical reasons [1, 2], which highlights the urgency and need for greater standardization in reporting. Consistent reporting in MMD/MMS can be facilitated by an agreed minimum set of indicators to be reported. With a unified standard of data reporting, this will enable valid evidence syntheses and ultimately implementation of management recommendations.
Limitations
Limitations of this meta-analysis include the retrospective and observational nature of included studies. Our study has also highlighted the limited number of studies directly comparing DB/CB and IB for MMD/MMS. This could explain the finding of non-significance in the various outcomes. Additionally, apart from perioperative events, there were no standard time frame with different lengths of clinical follow-up in each study. Furthermore, several outcomes reported in this study have a large encompassing confidence interval, which may be explained by the modest sample size and large heterogeneity between studies. As such, we advise to interpret these outcomes with great caution as the estimates were unlikely to be reliable. Only studies published in English were included; therefore, selection bias may exist because MMD has greater incidence rates among Asian populations. Based on the information from the included studies, our current meta-analysis could not assess whether or not the translation of subjective angiographic assessments across grading scales were accurate in the pediatric cohort. A possible relationship may be uncovered in future with more granular detail. Validation can be achieved by establishing a prospective data registry collected from multiple international centers which can inform future individual participant data meta-analysis in real-world settings. Our meta-analysis included a diverse range of patients of various ethnic diversity, enhancing its external validity. The large number of studies enabled us to perform a meta-regression to explore possible confounders. However, we cannot exclude the possibility that the conclusions drawn in our study may have been affected by residual confounders. Confounders that we did not control for in our analyses include surgeon experience although we controlled for the year of publication given that the surgical and peri-operative management of these patients has generally improved over time due to greater accrued understanding of the condition with time. Most importantly, this meta-analysis is the most reliable and transparent to date as we excluded repeated patient populations from the same institutions within overlapping time intervals.
Conclusions
IB, DB/CB techniques have both been demonstrated to be effective and safe revascularization options for pediatric MMD/MMS. A paucity of cohort studies has a limit direct comparison between these interventions. Available low-quality GRADE evidence suggests that DB/CB is associated with better long-term revascularization outcomes when compared with IB alone, although this did not translate to better long-term stroke outcomes.
Availability of data and material
Not applicable.
Code availability
Not applicable.
References
Scott RM, Smith ER (2009) Moyamoya disease and moyamoya syndrome. N Engl J Med 360(12):1226–1237
Scott RM et al (2004) Long-term outcome in children with moyamoya syndrome after cranial revascularization by pial synangiosis. J Neurosurg 100(2 Suppl Pediatrics):p. 142–9
Matsushima T et al (1998) Multiple combined indirect procedure for the surgical treatment of children with moyamoya disease. A comparison with single indirect anastomosis and direct anastomosis. Neurosurg Focus 5(5):p. e4
Morshed RA et al (2020) Clinical outcomes after revascularization for pediatric moyamoya disease and syndrome: a single-center series. J Clin Neurosci 79:137–143
Koss M et al (2013) Moyamoya syndrome associated with neurofibromatosis Type 1: perioperative and long-term outcome after surgical revascularization. J Neurosurg Pediatr 11(4):417–425
Karsten MB, Smith ER, Scott RM (2021) Late morbidity and mortality following revascularization surgery for moyamoya disease in the pediatric population. J Neurosurg Pediatr p. 1–6
Smith ER et al (2009) Pial synangiosis in patients with moyamoya syndrome and sickle cell anemia: perioperative management and surgical outcome. Neurosurg Focus 26(4):E10
Jackson EM et al (2014) Pial synangiosis in patients with moyamoya younger than 2 years of age. J Neurosurg Pediatr 13(4):420–425
Montaser A et al (2021) Long-term clinical and radiographic outcomes after pial pericranial dural revascularization: a hybrid surgical technique for treatment of anterior cerebral territory ischemia in pediatric moyamoya disease. J Neurosurg Pediatr p. 1–9
Ravindran K, Wellons JC, Dewan MC (2019) Surgical outcomes for pediatric moyamoya: a systematic review and meta-analysis. J Neurosurg Pediatr 24(6):663–672
Macyszyn L et al (2017) Direct versus indirect revascularization procedures for moyamoya disease: a comparative effectiveness study. J Neurosurg 126(5):1523–1529
Lunny C et al (2021) Managing overlap of primary study results across systematic reviews: practical considerations for authors of overviews of reviews. BMC Med Res Methodol 21(1):140
Page MJ et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372:n71
Czabanka M et al (2011) Characterization of direct and indirect cerebral revascularization for the treatment of European patients with moyamoya disease. Cerebrovasc Dis 32(4):361–369
Cohen J (1960) A coefficient of agreement for nominal scales. Educ Psychol Measur 20(1):37–47
Lee KS et al (2022) Tenets for the proper conduct and use of meta-analyses: a practical guide for neurosurgeons. World Neurosurg 161:291-302.e1
Hozo SP, Djulbegovic B, Hozo I (2005) Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol 5(1):13
Wan X et al (2014) Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol 14(1):135
Kennedy BC et al (2014) Pial synangiosis for moyamoya syndrome in children with sickle cell anemia: a comprehensive review of reported cases. Neurosurg Focus 36(1):E12
See AP et al (2015) Down syndrome and moyamoya: clinical presentation and surgical management. J Neurosurg Pediatr 16(1):58–63
Zhao M et al (2017) Adolescents with moyamoya disease: clinical features, surgical treatment and long-term outcomes. Acta Neurochir (Wien) 159(11):2071–2080
Zhao Y et al (2019) Comparison of long-term effect between direct and indirect bypass for pediatric ischemic-type moyamoya disease: a propensity score-matched study. Front Neurol 10:795
Zheng J et al (2019) Clinical features, surgical treatment, and long-term outcome of a multicenter cohort of pediatric moyamoya. Front Neurol 10:14
Ge P et al (2018) Clinical features, surgical treatment, and long-term outcome in children with hemorrhagic moyamoya disease. J Stroke Cerebrovasc Dis 27(6):1517–1523
Wang C et al (2018) Encephaloduroarteriosynangiosis for pediatric moyamoya disease: a single-center experience with 67 cases in China. J Child Neurol 33(14):901–908
Ahn ES et al (2013) Chorea in the clinical presentation of moyamoya disease: results of surgical revascularization and a proposed clinicopathological correlation. J Neurosurg Pediatr 11(3):313–319
Gaillard J et al (2017) Incidence, clinical features, and treatment of familial moyamoya in pediatric patients: a single-institution series. J Neurosurg Pediatr 19(5):553–559
Riordan CP et al (2019) Results of more than 20 years of follow-up in pediatric patients with moyamoya disease undergoing pial synangiosis. J Neurosurg Pediatr p. 1–7
Jea A et al (2005) Moyamoya syndrome associated with Down syndrome: outcome after surgical revascularization. Pediatrics 116(5):e694-701
Robertson RL et al (1997) Angiographic changes after pial synangiosis in childhood moyamoya disease. AJNR Am J Neuroradiol 18(5):837–845
Kim SK et al (2010) Pediatric moyamoya disease: an analysis of 410 consecutive cases. Ann Neurol 68(1):92–101
Choi JW et al (2020) Postoperative symptomatic cerebral infarction in pediatric moyamoya disease: risk factors and clinical outcome. World Neurosurg 136:e158–e164
Phi JH et al (2011) Long-term social outcome in children with moyamoya disease who have reached adulthood. J Neurosurg Pediatr 8(3):303–309
Kim CY et al (2003) Encephaloduroarteriosynangiosis with bifrontal encephalogaleo(periosteal)synangiosis in the pediatric moyamoya disease: the surgical technique and its outcomes. Childs Nerv Syst 19(5–6):316–324
Alamri A et al (2019) Encephaloduroateriosynangiosis (EDAS) in the management of Moyamoya syndrome in children with sickle cell disease. Br J Neurosurg 33(2):161–164
Araki Y et al (2022) Risk factors for cerebral infarction early after revascularization in children younger than 5 years with moyamoya disease. World Neurosurg 160:e220–e226
Bao XY et al (2015) Clinical features, surgical treatment, and long-term outcome in pediatric patients with moyamoya disease in China. Cerebrovasc Dis 39(2):75–81
Blauwblomme T et al (2017) Long-term outcome after multiple burr hole surgery in children with moyamoya angiopathy: a single-center experience in 108 hemispheres. Neurosurgery 80(6):950–956
Chen C et al (2018) Surgical revascularization for children with moyamoya disease: a new modification to the pial synangiosis. World Neurosurg 110:e203–e211
Czabanka M et al (2009) Age-dependent revascularization patterns in the treatment of moyamoya disease in a European patient population. Neurosurg Focus 26(4):E9
Darwish B, Besser M (2005) Long term outcome in children with Moyamoya disease: experience with 16 patients. J Clin Neurosci 12(8):873–877
Oliveira RS et al (2009) Effect of multiple cranial burr hole surgery on prevention of recurrent ischemic attacks in children with moyamoya disease. Neuropediatrics 40(6):260–264
Deng X et al (2021) Risk factors for postoperative ischemic complications in pediatric moyamoya disease. BMC Neurol 21(1):229
Funaki T et al (2014) Incidence of late cerebrovascular events after direct bypass among children with moyamoya disease: a descriptive longitudinal study at a single center. Acta Neurochir (Wien) 156(3):p. 551–9; discussion 559
Furtado SV et al (2021) Surgical outcome of encephaloduroarteriomyosynangiosis for moyamoya disease. Neurol India 69(5):1259–1264
Gadgil N et al (2018) Indirect revascularization with the dural inversion technique for pediatric moyamoya disease: 20-year experience. J Neurosurg Pediatr 22(5):541–549
Goren O et al (2021) Encephaloduroarteriosynangiosis with dural inversion for moyamoya disease in a pediatric and adult population-a single-center 20-year experience. World Neurosurg 149:e16–e21
Griessenauer CJ et al (2015) Encephaloduroarteriosynangiosis and encephalomyoarteriosynangiosis for treatment of moyamoya syndrome in pediatric patients with sickle cell disease. J Neurosurg Pediatr 16(1):64–73
Guzman R et al (2009) Clinical outcome after 450 revascularization procedures for moyamoya disease: clinical article. J Neurosurg 111(5):927–935
Ha EJ et al (2019) Long-term outcomes of indirect bypass for 629 children with moyamoya disease: longitudinal and cross-sectional analysis. Stroke 50(11):3177–3183
Hall EM et al (2016) Reduction in overt and silent stroke recurrence rate following cerebral revascularization surgery in children with sickle cell disease and severe cerebral vasculopathy. Pediatr Blood Cancer 63(8):1431–1437
Ishikawa T et al (1997) Effects of surgical revascularization on outcome of patients with pediatric moyamoya disease. Stroke 28(6):1170–1173
Isono M et al (2002) Long-term outcomes of pediatric moyamoya disease treated by encephalo-duro-arterio-synangiosis. Pediatr Neurosurg 36(1):14–21
Karasawa J et al (1992) Long-term follow-up study after extracranial-intracranial bypass surgery for anterior circulation ischemia in childhood moyamoya disease. J Neurosurg 77(1):84–89
Kim DS et al (2007) Surgical results in pediatric moyamoya disease: angiographic revascularization and the clinical results. Clin Neurol Neurosurg 109(2):125–131
King JA et al (2010) Relative contributions of the middle meningeal artery and superficial temporal artery in revascularization surgery for moyamoya syndrome in children: the results of superselective angiography. J Neurosurg Pediatr 5(2):184–189
Kuroda S et al (2010) Novel bypass surgery for moyamoya disease using pericranial flap: its impacts on cerebral hemodynamics and long-term outcome. Neurosurgery 66(6):1093–101; discussion 1101
Mirone G et al (2019) Multiple burr-hole surgery for the treatment of moyamoya disease and quasi-moyamoya disease in children: preliminary surgical and imaging results. World Neurosurg 127:e843–e855
Ng J et al (2012) Surgical revascularisation for childhood moyamoya. Childs Nerv Syst 28(7):1041–1048
Ogiwara H, Morota N (2012) Bifrontal encephalogaleosynangiosis for children with moyamoya disease. J Neurosurg Pediatr 10(3):246–251
Ong JA et al (2020) Revascularisation surgery for paediatric moyamoya disease: The Singapore experience. J Clin Neurosci 82(Pt B):207–213
Rashad S et al (2016) Long-term follow-up of pediatric moyamoya disease treated by combined direct-indirect revascularization surgery: single institute experience with surgical and perioperative management. Neurosurg Rev 39(4):615–623
Sadashiva N et al (2016) Moyamoya disease: experience with direct and indirect revascularization in 70 patients from a nonendemic region. Neurol India 64(Suppl):S78-86
Sakamoto H et al (1997) Direct extracranial-intracranial bypass for children with moyamoya disease. Clin Neurol Neurosurg 99(Suppl 2):S128–S133
Shen W et al (2017) Enlarged encephalo-duro-myo-synangiosis treatment for moyamoya disease in young children. World Neurosurg 106:9–16
Winstead M et al (2017) Encephaloduroarteriosynangiosis (EDAS) in young patients with cerebrovascular complications of sickle cell disease: single-institution experience. Pediatr Hematol Oncol 34(2):100–106
Yang W et al (2017) Effectiveness of surgical revascularization for stroke prevention in pediatric patients with sickle cell disease and moyamoya syndrome. J Neurosurg Pediatr 20(3):232–238
Titsworth WL, Scott RM, Smith ER (2016) National analysis of 2454 pediatric moyamoya admissions and the effect of hospital volume on outcomes. Stroke 47(5):1303–1311
Nguyen VN et al (2022) Direct, indirect, and combined extracranial-to-intracranial bypass for adult moyamoya disease: an updated systematic review and meta-analysis. Stroke p. 101161STROKEAHA122039584
Jeon JP et al (2018) Meta-analysis of the surgical outcomes of symptomatic moyamoya disease in adults. J Neurosurg 128(3):793–799
Acknowledgements
A special thank you to Kenneth Kek Wee Lee (Papa), Lena Lim (Mama), and Chio Tee Koh (Ahma) back home for their unwavering support, without which, I (Keng Siang Lee) would not be able to achieve my educational goals. Love truly overcomes all obstacles (different time zones and distance). I love you all!
Author information
Authors and Affiliations
Contributions
All authors listed have made substantial, direct, and intellectual contribution to the work and approved it for publications. Keng Siang Lee: conceptualization, methodology, formal analysis and investigation, writing—original draft preparation, writing—review and editing, visualization, funding acquisition. John J. Y. Zhang: conceptualization, methodology, formal analysis and investigation, writing—review and editing, visualization. Sanjay Bhate: writing—review and editing, supervision. Vijeya Ganesan: writing—review and editing, supervision. Dominic Thompson: conceptualization, writing—review and editing, supervision. Greg James: conceptualization, writing—review and editing, supervision. Adikarige Haritha Dulanka Silva: conceptualization, writing—review and editing, supervision.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Consent for publication
Not applicable.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lee, K.S., Zhang, J.J.Y., Bhate, S. et al. Surgical revascularizations for pediatric moyamoya: a systematic review, meta-analysis, and meta-regression analysis. Childs Nerv Syst 39, 1225–1243 (2023). https://doi.org/10.1007/s00381-023-05868-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-023-05868-6