Abstract
Introduction
Pial arteriovenous fistulas (pAVF) are rare vascular malformations, especially in children and newborns. In neonates, the most common symptom is congestive heart failure.
Case presentation
We report a case of an asymptomatic preterm newborn incidentally diagnosed with pAVF during a routine cranial ultrasound (cUS) on the third day of life. Cerebral magnetic resonance (MRI) confirmed the diagnosis. A wait-and-see approach was chosen by the multidisciplinary team. The cUS and the MRI on day 14 of life showed the spontaneous resolution of the lesion.
Conclusions
This case underlines the challenges in identifying pAVF in the first weeks of life and demonstrates a possible positive outcome for affected neonates.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Avoid common mistakes on your manuscript.
Introduction
Neonatal intracranial vascular malformations represent a rare clinical entity. They can be divided into malformations without and with arteriovenous (AV) shunt [1, 2]. The latter comprise different lesions with various etiologies, treatment options, and outcomes, including vein of Galen aneurysmal malformations (VGAMs) and single-hole pial arteriovenous fistulas (pAVFs, also known as non-Galenic fistulas). If VGAMs account for about 1% of the abnormalities of the foetal cerebral arteriovenous system [3, 4], PAVFs are rarely seen in the first year of life, and no extensive epidemiologic data are available. In the largest available series of AV malformations published by Lasjaunias et al., neonatal pAVFs accounted for 15% [5]. PAVFs are more frequently localized in the supratentorial compartment [5, 6]. They are defined as abnormal and direct communications between intracranial pial arteries and veins without an interposed capillary bed or malformative nidus. The angio-architectural differences, the age of the patient, and the clinical presentation influence the management strategies [7].
Digital subtraction angiography (DSA) has long been the gold standard to detect and confirm cerebro- and spinovascular lesions, like pAVFs, but has the disadvantages of invasiveness, need for procedural preparation, and expenses. Cerebral magnetic resonance imaging (MRI) with MR angiography can be another, less demanding technique to define pAVFs’ features (origin, size, localization, and angioarchitecture) [8,9,10].
Clinically, the most common presentation in children is congestive heart failure (from fistula overload) [5, 9], and haemorrhage, among others [10]. Treatment options in newborns are similar to those in the adult population, although limitations exist due to body weight, size of the lesion, and potential comorbidities [7]: endovascular treatment is the preferred approach [11,12,13].
We describe a unique case of a pAVF incidentally diagnosed in an asymptomatic preterm newborn from a neurological point of view showing a benign evolution and no need for surgical or endovascular intervention. A literature review follows this case report.
Case report
Perinatal history
A female preterm infant was born via urgent cesarean section at 31+5 gestational weeks (GW) due to alteration of the cardiotocographic trace. The pregnancy was characterized by maternal hypertension and intrauterine growth restriction (IUGR) at 30+6 GW. No maternal infectious disease markers were present: serologies, blood tests (c-reactive protein, blood count and biochemical profile), and urine culture were negative.
At birth, the newborn was in good condition with normal vital parameters sign. At 8 min of life, due to dyspnea, continuous positive airway pressure (CPAP) was started with neonatal resuscitation T-piece. Arterial cordonal blood gas analysis was balanced. Given the gestational age and the need for respiratory support, the newborn was transported to the neonatal intensive care unit (NICU) for further care.
Neonatal course and investigations
On admission at our NICU (Padova University Hospital, Italy), the baby was alert with a mild hypotonia (explainable by the gestational age and the IUGR). Her birth weight was 1540 gr (40th%ile). Due to increased dyspnoea, a nasal intermittent mandatory ventilation was preferred. An umbilical central venous catheter was placed.
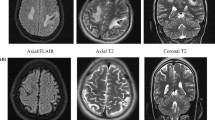
On admission, a cerebral ultrasound (cUS) was performed showing a cystic lesion in the left germinal matrix. However, the following cUS on day 3 of life (DOL) depicted the presence of flow within the cyst on colour Doppler mode, revealing a vascular nature of the lesion (Fig. 1a). Neurological examination was normal. A brain MRI scan was therefore carried out, which demonstrated a flow void in the site of the lesion depicted at cUS, interpreted as a venous pouch. A time-of-flight (ToF) MR angiography showed arterial flow in the pouch due to the presence of a fistula with two feeders from the posterior cerebral arteries and a single deep venous drainage into the vein of Galen. In addition, T1-weighted images demonstrated hyperintensity in the posterior wall of the pouch, due to initial thrombosis (Fig. 1b–d). Considering the radiological features of the lesion, the gestational age, and the weight of the patient, decision was taken for a conservative approach consisting of cardiovascular monitoring and serial cUS examinations (every 2 days). Lastly, an amplitude-integrated-EEG was carried out and resulted to be normal. No other vascular malformations were detected at abdominal US. No genetic investigation was required, given the sporadic nature of the lesion.
Evolution
The patient remained clinically stable for the course of the NICU hospitalization, with normal haematocrit levels. The cUS performed at 14 DOL showed increased echogenicity inside the vascular pouch (Fig. 2a–c). A follow-up brain MRI scan showed disappearance of the vascular flow inside the pouch due to complete spontaneous thrombosis. Additionally, arterial flow was no longer visible in both feeding and draining vessels (Fig. 2c, d).
a Cerebral ultrasound demonstrating a “cystic” lesion in the left germinal matrix with flow on color Doppler mode. b A ToF MR angiography in the arterial phase shows arterial flow in the pouch and the presence of a fistula with two feeders from the posterior cerebral arteries. c A single deep venous drainage into the vein of Galen is noted. d A T1-weighted MR image demonstrates hyperintensity of the posterior wall of the pouch due to partial thrombosis.
The baby was discharged at 40+2 GW (60th DOL). Her neurological examination was adequate for age with normal head circumference.
The 12-month follow-up visit demonstrated a normal neurological exam with good and appropriate psychomotor evolution for the corrected GA.
An MRI with MR angiography at the same age confirmed the absence of the vascular lesion and its afferent and efferent branches and the remnant small malacic area adjacent to the left lateral ventricle.
Review of literature
A comprehensive literature search on intracranial arteriovenous fistula in neonates was performed on PubMed/MEDLINE online databases. The following key words and Medical Subject Heading terms were used: “newborn”, “infant”, “neonate”, “pediatric”, “intracranial”, “cerebral”, and “pial arteriovenous fistula”. Articles written in English and published between 2005 and October 2021 were included. Nine articles were selected after the application of the above-listed criteria (Table 1).
Table 1 summarizes data on pAVFS in the neonatal population: 35 patients with diagnosis of pAVFs have been reported in the last 15 years in the neonatal and infant population (Table 1). The postnatal incidental detection, the prematurity of the patient, the diagnostic process, the management, and the unusual clinical progression warrant the relevance of reporting our case.
To our knowledge, this is the first case describing an incidental diagnosis and a spontaneous resolution of a pAVF. Moreover, pAVF involving the posterior circulation are rare in newborns and even rarer in preterm newborns [7].
According to our review of the literature, heart failure, epilepsy, and macrocrania are the most common manifestations of pAVFs [3, 4, 7,8,9, 12,13,14,15]. Luckily, our case was not diagnosed due to such clinical presentation but during a routine cUS. This also highlights the role of a non-invasive tool like cUS and the importance of using colour Doppler to evaluate the nature of cystic lesions. cUS may also be useful in the monitoring of these lesions over time. After this case, we have well-defined redefined o reviewed our local protocol, recommending the use of colour Doppler to investigate any cerebral cystic lesions. Post-natal MRI and angiography can be useful, fast, and non-invasive tools to confirm the presence of cerebrovascular lesions and pAVFs. Indeed, almost all cases of arterial aneurysms described in the literature so far were diagnosed or confirmed by MRI and/or angiography after an antenatal suspicion or after a typical clinical presentation [3, 4, 8,9,10, 13,14,15,16].
DSA in newborns should be performed mainly in the case of a life-threatening condition to address a complete or partial occlusion of the AV shunt. The possibility of obtaining detailed diagnostic information on the vascular lesion and the surrounding tissues by means of DSA was rejected in our case in consideration of the low weight of the baby that allowed only a very small amount of contrast to be used. Additionally, the steal phenomenon caused by the AV shunt often prevents a detailed assessment.
Both surgical and endovascular approaches can be used to control the AV shunt. In recent years, thanks to technological improvements and the growing experience of neuroradiologists, endovascular techniques have gained a more important role in treating AV shunts, even in children and newborns [16]. Therefore, the risks and benefits of both endovascular and surgical approaches must be carefully considered, and a case-by-case evaluation should be adopted.
The most relevant feature of our case was the occurrence of a spontaneous thrombosis of the lesion with a good outcome despite the early onset. This favourable course of the disease was the ideal one among the 3 hypothesized during the multidisciplinary meetings. The other possible outcomes were, in fact, the progressive growth of the lesion and the haemorrhagic rupture of the venous pouch. The “wait-and-see” approach was weighed against the option of an endovascular approach, and the decision was guided by the age of the patient and the absence of clinical symptoms related to the lesion. These benefits were considered to be greater than the risk of the procedure.
The clinical stability of the patient radically changed the management plan, with no further need for invasive procedures. So far, no clear explanation for this phenomenon could be proposed.
Given the rarity of the condition, an international database of newborns affected by AV shunts in the first 28 days of life could help in delineating a standardized management of these vascular malformations according to GW and weight. A multidisciplinary operational framework is suggested, which needs to take into account the chance of a positive outcome without any treatment.
Conclusion
Intracranial vascular malformations are rare conditions in the neonatal population. Few data in preterm infants and no standardized management and therapeutic protocols are available. This case of unexpected spontaneous thrombosis of a cerebral pial arteriovenous fistula in a preterm neonate represents an unusual event. An international collaboration to collect data of affected patients may be useful in the further development of shared guidelines.
Availability of data and materials
Not applicable.
Abbreviations
- PAVF or pAVF:
-
Pial arteriovenous fistulas
- cUS :
-
Cranial ultrasound
- MRI :
-
Cerebral magnetic resonance
- AV:
-
Arteriovenous
- VGAMs :
-
Vein of Galen aneurysmal malformations
- GW :
-
Gestational weeks
- IUGR :
-
Intrauterine growth restriction
- CPAP :
-
Continuous positive airway pressure
- NICU :
-
Neonatal intensive care unit
- DOL :
-
Day of life
- DSA :
-
Digital subtraction angiography
References
Eguchi S, Aihara Y, Yamaguchi K, Okada Y (2012) Limitations of fetal ultrasonography and magnetic resonance imaging in prenatal diagnosis of congenital cerebral arteriovenous malformations with hemorrhagic onset. J Neurosurg Pediatr 10(2):154–158
Long DM, Seljeskog EL, Chou SN et al (1974) Giant arteriovenous malformations of infancy and childhood. J Neurosurg 40:304–311
Zuccaro G, Argañara RZ, Villasante F et al (2010) Neurosurgical vascular malformations in children under 1 year of ag. Childs Nerv Sys 26(10):1381–94
Pedicelli A, Iacobucci M, Frassanito P (2017) Prenatal diagnosis and multimodal neonatal treatment of a rare pial arteriovenous fistula: case report and review of the literature. World Neurosurg 104:1050.e13-1050.e18
Lasjaunias P, Hui F, Zerah M et al (1995) Cerebral arteriovenous malformations in children. Management of 179 consecutive cases and review of the literature. Childs Nerv Syst 11(2):66–79; discussion 79
Yoshida Y, Weon YC, Sachet M, Mahadevan J (2004) Posterior cranial fossa single-hole arteriovenous fistulae in children: 14 consecutive cases. Neuroradiology 46(6):474–481
Berenstein A, Ortiz R, Niimi Y, Elijovich L, Fifi J, Madrid M, Ghatan S, Molofsky W (2010) Endovascular management of arteriovenous malformations and other intracranial arteriovenous shunts in neonates, infants, and children. Childs Nerv Syst 26:1345–1358
Zareen F, Keiichi I, Masaaki H, Tsutomu A (2010) Time-resolved contrast-enhanced magnetic resonance digital subtraction angiography (MRDSA) in an infant with congenital pial arteriovenous fistula in the brain: a case report. Nerv Syst 26(8):1121–4
Maejima R, Ohshima T, Miyachi S (2018) Neonatal intracranial pial arteriovenous fistula treated with endovascular embolization: a case report. World Neurosurg 118:261–264
Kraneburg UM, Nga VDW, Ting EYS et al (2014) Intracranial pial arteriovenous fistula in infancy: a case report and literature review. Childs Nerv Syst 30(2):365–369
Niimi Y (2017) Endovascular treatment of pediatric intracranial arteriovenous shunt. Pediatr Int 59(3):247–257
Vasan R, Patel J, Sweeney JM, Carpenter AM, Downes K, Youssef AS, van Loveren H, Agazzi S (2013) Pediatric intracranial aneurysms: current national trends in patient management and treatment. Childs Nerv Syst 29(3):451–6
Cooke D, Tatum J, Farid H et al (2012) Transvenous embolization of a pediatric pial arteriovenous fistula. J Neurointerv Surg 4(4):e14
Martínez-Payo C, Sancho Saúco J, Miralles M et al (2017) Nongalenic pial arteriovenous fistula: prenatal diagnosis. J Clin Ultrasound 45(9):621–625
Potter CA, Armstrong-Wells J, Fullerton HJ et al (2009) Neonatal giant pial arteriovenous malformation: genesis or rapid enlargement in the third trimester. J Neurointerv Surg 1(2):151–3
Weon YC, Yoshida Y, Sachet M et al (2004) Supratentorial cerebral arteriovenous fistulas (AVFs) in children: review of 41 cases with 63 non choroidal single-hole AVFs. Acta Neurochir 147(1):17–31
Funding
Open access funding provided by Università degli Studi di Padova within the CRUI-CARE Agreement.
Author information
Authors and Affiliations
Contributions
SC, LM, SS, GT, NM, PE wrote the main manuscript text. LM prepared ultra-sound figures; GT and FC proposed MRI figures of the case. All authors contributed to the manuscript, reviewed it, and accepted it in the last form.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Conflict of interest
The authors have no conflict of interest to declare concerning the current manuscript.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sabrina, C., Laura, M., Sabrina, S. et al. Expect the unexpected: a case of spontaneous thrombosis of a pial arteriovenous fistula in a preterm newborn with review of the literature. Childs Nerv Syst 39, 793–799 (2023). https://doi.org/10.1007/s00381-022-05652-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-022-05652-y