Abstract
Introduction
Paediatric ventriculomegaly without obvious signs or symptoms of raised intracranial pressure (ICP) is often interpreted as resulting from either relative brain atrophy, arrested “benign” hydrocephalus, or “successful” endoscopic third ventriculostomy (ETV). We hypothesise that the typical ICP “signature” found in symptomatic hydrocephalus can be present in asymptomatic or oligosymptomatic children, indicating pressure-compensated, but active hydrocephalus.
Methods
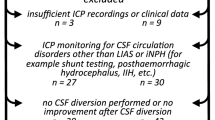
A total of 37 children fulfilling the mentioned criteria underwent computerised ICP overnight monitoring (ONM). Fifteen children had previous hydrocephalus treatment. ICP was analysed for nocturnal dynamics of ICP, ICP amplitudes (AMP), magnitude of slow waves (SLOW), and ICP/AMP correlation index RAP. Depending on the ONM results, children were either treated or observed. The ventricular width was determined at the time of ONM and at 1-year follow-up.
Results
The recordings of 14 children (group A) were considered normal. In the 23 children with pathologic recordings (group B), all ICP values and dependent variables (AMP, SLOW) were significantly higher, except for RAP. In group B, 12 of 15 children had received a pre-treatment and 11 of 22 without previous treatment. All group B children received treatment for hydrocephalus and showed a significant reduction of frontal-occipital horn ratio at 1 year. During follow-up, a positive neurological development was seen in 74% of children of group A and 100% of group B.
Conclusion
Ventriculomegaly in the absence of signs and symptoms of raised ICP was associated in 62% of cases to pathological ICP dynamics. In 80% of pre-treated cases, ETV or shunt failure was found. Treating children with abnormal ICP dynamics resulted in an outcome at least as favourable as in the group with normal ICP dynamics. Thus, asymptomatic ventriculomegaly in children deserves further investigation and, if associated with abnormal ICP dynamics, should be treated in order to provide a normalised intracranial physiology as basis for best possible long-term outcome.





Similar content being viewed by others
Abbreviations
- AMP:
-
Fundamental amplitude (1st harmonic) of ICP after Fourier trans-formation
- CPC:
-
Choroid plexus cauterization
- CSF:
-
Cerebrospinal fluid
- ETV:
-
Endoscopic third ventriculostomy
- FOHR:
-
Frontal-occipital horn ratio
- ICP:
-
Intracranial pressure
- IVH:
-
Intraventricular haemorrhage
- LIAS:
-
Late onset idiopathic aqueduct stenosis
- LOVA:
-
Long-standing overt ventriculomegaly
- PC-MRI:
-
Phase-contrast magnetic resonance imaging
- ONM:
-
Overnight monitoring
- VP-shunt:
-
Ventriculoperitoneal shunt
References
Hamilton R et al (2012) Intracranial pressure pulse waveform correlates with aqueductal cerebrospinal fluid stroke volume. J Appl Physiol (1985) 113(10):1560–1566
Ringstad G, Lindstrøm EK, Vatnehol SAS, Mardal KA, Emblem KE, Eide PK (2017) Non-invasive assessment of pulsatile intracranial pressure with phase-contrast magnetic resonance imaging. PLoS One 12(11):e0188896
Di Rocco C et al (1975) Continuous intraventricular cerebrospinal fluid pressure recording in hydrocephalic children during wakefulness and sleep. J Neurosurg 42(6):683–689
Di Rocco C et al (1977) The study of cerebrospinal fluid dynamics in apparently ‘arrested’ hydrocephalus in children. Childs Brain 3(6):359–374
Mataro M et al (2001) Neuropsychological findings in congenital and acquired childhood hydrocephalus. Neuropsychol Rev 11(4):169–178
Donders J, Rourke BP, Canady AI (1991) Neuropsychological functioning of hydrocephalic children. J Clin Exp Neuropsychol 13(4):607–613
Erickson K, Baron IS, Fantie BD (2001) Neuropsychological functioning in early hydrocephalus: review from a developmental perspective. Child Neuropsychol 7(4):199–229
Mataro M et al (2000) Cognitive changes after cerebrospinal fluid shunting in young adults with spina bifida and assumed arrested hydrocephalus. J Neurol Neurosurg Psychiatry 68(5):615–621
Frank SV, Lazarus T, Nathoo N (2003) Visuospatial deficits in children 3-7 years old with shunted hydrocephalus. S Afr Med J 93(11):865–868
Lacy M, Pyykkonen BA, Hunter SJ, Do T, Oliveira M, Austria E, Mottlow D, Larson E, Frim D (2008) Intellectual functioning in children with early shunted posthemorrhagic hydrocephalus. Pediatr Neurosurg 44(5):376–381
Schuhmann MU, Sood S, McAllister JP, Jaeger M, Ham SD, Czosnyka Z, Czosnyka M (2008) Value of overnight monitoring of intracranial pressure in hydrocephalic children. Pediatr Neurosurg 44(4):269–279
Fallah A, Weil AG, Juraschka K, Ibrahim GM, Wang AC, Crevier L, Tseng CH, Kulkarni AV, Ragheb J, Bhatia S (2017) The importance of extent of choroid plexus cauterization in addition to endoscopic third ventriculostomy for infantile hydrocephalus: a retrospective North American observational study using propensity score-adjusted analysis. J Neurosurg Pediatr 20(6):503–510
Dewan MC, Naftel RP (2017) The global rise of endoscopic third ventriculostomy with choroid plexus cauterization in pediatric hydrocephalus. Pediatr Neurosurg 52(6):401–408
Kulkarni AV, Riva-Cambrin J, Rozzelle CJ, Naftel RP, Alvey JS, Reeder RW, Holubkov R, Browd SR, Cochrane DD, Limbrick DD, Simon TD, Tamber M, Wellons JC, Whitehead WE, Kestle JRW (2018) Endoscopic third ventriculostomy and choroid plexus cauterization in infant hydrocephalus: a prospective study by the Hydrocephalus Clinical Research Network. J Neurosurg Pediatr 21(3):214–223
Weerakkody RA, Czosnyka M, Schuhmann MU, Schmidt E, Keong N, Santarius T, Pickard JD, Czosnyka Z (2011) Clinical assessment of cerebrospinal fluid dynamics in hydrocephalus. Guide to interpretation based on observational study. Acta Neurol Scand 124(2):85–98
Dias, S.F., et al., Value of computerized shunt infusion study in assessment of pediatric hydrocephalus shunt function-a two center cross-sectional study. Childs Nerv Syst, 2019.
Czosnyka M, Czosnyka Z, Momjian S, Pickard JD (2004) Cerebrospinal fluid dynamics. Physiol Meas 25(5):R51–R76
Czosnyka M, Pickard JD (2004) Monitoring and interpretation of intracranial pressure. J Neurol Neurosurg Psychiatry 75(6):813–821
Ragan DK, Cerqua J, Nash T, McKinstry RC, Shimony JS, Jones BV, Mangano FT, Holland SK, Yuan W, Limbrick DD (2015) The accuracy of linear indices of ventricular volume in pediatric hydrocephalus: technical note. J Neurosurg Pediatr 15(6):547–551
O’Hayon B et al (1998) Frontal and occipital horn ratio: a linear estimate of ventricular size for multiple imaging modalities in pediatric hydrocephalus. Pediatr Neurosurg 29:245–249
Bourne S et al (2013) Linear measurements of the cerebral ventricles are correlated with adult ventricular volume. J Clin Neurosci 20:763–764
Czosnyka M et al (2014) Monitoring of intracranial pressure and assessment of cerebrospinal fluid dynamics. In: Rigamonti D (ed) Adult Hydrocephalus. Cambridge University Press, Cambridge
Czosnyka, M., et al., Cerebrospinal fluid pressure dynamics, in Pediatric hydrocephalus, G. Cinalli, Editor. 2019, Springer Nature Switzerland: Switzerland.
Czosnyka M, Whitehouse H, Smielewski P, Kirkpatrick P, Guazzo EP, Pickard JD (1994) Computer supported multimodal bed-side monitoring for neuro intensive care. Int J Clin Monit Comput 11(4):223–232
Droste DW, Krauss JK (1999) Intracranial pressure B-waves precede corresponding arterial blood pressure oscillations in patients with suspected normal pressure hydrocephalus. Neurol Res 21(7):627–630
Kerscher SR, Schöni D, Hurth H, Neunhoeffer F, Haas-Lude K, Wolff M, Schuhmann MU (2020) The relation of optic nerve sheath diameter (ONSD) and intracranial pressure (ICP) in pediatric neurosurgery practice - part I: correlations, age-dependency and cut-off values. Childs Nerv Syst 36(1):99–106
Fukuhara T, Luciano MG (2001) Clinical features of late-onset idiopathic aqueductal stenosis. Surg Neurol 55(3):132–136 discussion 136-7
Canu ED et al (2005) Neuropsychophysiological findings in a case of long-standing overt ventriculomegaly (LOVA). Neurosci Lett 385(1):24–29
Burtscher J, Bartha L, Twerdy K, Eisner W, Benke T (2003) Effect of endoscopic third ventriculostomy on neuropsychological outcome in late onset idiopathic aqueduct stenosis: a prospective study. J Neurol Neurosurg Psychiatry 74(2):222–225
Di Rocco C, Caldarelli M, Ceddia A (1989) “Occult” hydrocephalus in children. Childs Nerv Syst 5(2):71–75
Padayachy LC, Padayachy V, Galal U, Gray R, Fieggen AG (2016) The relationship between transorbital ultrasound measurement of the optic nerve sheath diameter (ONSD) and invasively measured ICP in children: part I: repeatability, observer variability and general analysis. Childs Nerv Syst 32(10):1769–1778
Kerscher SR, Schöni D, Neunhoeffer F, Wolff M, Haas-Lude K, Bevot A, Schuhmann MU (2020) The relation of optic nerve sheath diameter (ONSD) and intracranial pressure (ICP) in pediatric neurosurgery practice - part II: influence of wakefulness, method of ICP measurement, intra-individual ONSD-ICP correlation and changes after therapy. Childs Nerv Syst 36(1):107–115
Ertl M, Aigner R, Krost M, Karnasová Z, Müller K, Naumann M, Schlachetzki F (2017) Measuring changes in the optic nerve sheath diameter in patients with idiopathic normal-pressure hydrocephalus: a useful diagnostic supplement to spinal tap tests. Eur J Neurol 24(3):461–467
Author information
Authors and Affiliations
Contributions
SFD and MUS: conception and design of the study, acquisition of data, descriptive and statistical analysis, interpretation of data, and drafting the article. EJ: acquisition of data and statistical analysis. MUS: in addition critical revision of all article versions. JZ, KH, AB and HO: collection of data. All authors critically reviewed the results and contributed to the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
None of the authors reports conflicts of interest with regards to this work. The authors declare that this study was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The authors state that this work has not been previously published in whole or in part, or submitted elsewhere for review.
Rights and permissions
About this article
Cite this article
Dias, S.F., Jehli, E., Haas-Lude, K. et al. Ventriculomegaly in children: nocturnal ICP dynamics identify pressure-compensated but active paediatric hydrocephalus. Childs Nerv Syst 37, 1883–1893 (2021). https://doi.org/10.1007/s00381-021-05164-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-021-05164-1