Abstract
Introduction
Hydrocephalus is variously associated to syndromic craniosynostosis (CS), while it is randomly encountered in monosutural CS. Pathogenesis is still debated and reliable criteria for the diagnosis of overt hydrocephalus are lacking. Additionally, optimal treatment is controversial since it should balance the need to relieve intracranial hypertension and the risk of recurrence favored by lowering intracranial pressure.
Methods
A thorough review of the literature has been performed. Accordingly, pathogenic theories, diagnostic issues, and treatment options on hydrocephalus presenting in the context of CS are discussed.
Results
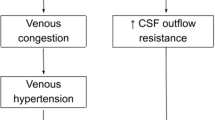
The association of hydrocephalus to simple CS is considered a fortuitous event. Its treatment is usually driven by the etiology and clinical relevance of hydrocephalus, favoring treatment before surgical correction to reduce CSF-related complications. On the other side, pathogenesis of hydrocephalus in the context of syndromic CS has been mainly related to factors that are secondary to the synostostic process, such as craniocerebral disproportion and venous hypertension. Hydrocephalus complicates 12–15% of syndromic CS, though its incidence is more relevant in FGFR2-related CS and raises up to 88% in Pfeiffer syndrome. Overt hydrocephalus should be properly differentiated by non-tense ventriculomegaly that is more frequent in Apert syndrome. Since intracranial hypertension is constant in syndromic CS even in the absence of active hydrocephalus, radiological monitoring of ventricular size along with intracranial pressure monitoring is essential. Active hydrocephalus occurs more frequently in infants, though stable ventriculomegaly may evolve into overt hydrocephalus after cranial expansion. If hydrocephalus is not clinically prominent, cranial expansion should be favored as first surgical step. Although posterior cranial expansion may address posterior cranial fossa constriction and stabilize ventricular dilation, effectiveness in long-term control of hydrocephalus is not clear. ETV is an effective treatment option, though success rate is affected by the presence of brain malformations and patient age. Extrathecal CSF shunting should be used as last resource due to the increased risk of complications in this context.
Conclusions
The pathogenesis of hydrocephalus complicating syndromic CS should be further investigated. Concomitantly, the definition of reliable diagnostic criteria is advocated in order to promptly and properly identify active hydrocephalus. Finally, treatment algorithm should refine the best timing and treatment options aiming to relieve intracranial hypertension on one side and reduce the risk of restenosis on the other side.





Similar content being viewed by others
References
Collmann H, Sörensen N, Krauss J (2005) Hydrocephalus in craniosynostosis: a review. Childs Nerv Syst 21:902–912. https://doi.org/10.1007/s00381-004-1116-y
Cinalli G, Sainte-Rose C, Kollar EM, Zerah M, Brunelle F, Chumas P, Arnaud E, Marchac D, Pierre-Kahn A, Renier D (1998) Hydrocephalus and craniosynostosis. J Neurosurg 88:209–214. https://doi.org/10.3171/jns.1998.88.2.0209
Di Rocco F, Jucá CE, Arnaud E et al (2010) The role of endoscopic third ventriculostomy in the treatment of hydrocephalus associated with faciocraniosynostosis. J Neurosurg Pediatr 6:17–22. https://doi.org/10.3171/2010.3.PEDS09484
Di Rocco C, Frassanito P, Massimi L, Peraio S (2011) Hydrocephalus and Chiari type I malformation. Childs Nerv Syst 27:1653–1664. https://doi.org/10.1007/s00381-011-1545-3
Massimi L, Pennisi G, Frassanito P, Tamburrini G, di Rocco C, Caldarelli M (2019) Chiari type I and hydrocephalus. Childs Nerv Syst 35:1701–1709. https://doi.org/10.1007/s00381-019-04245-6
Kreiborg S, Marsh JL, Cohen MM et al (1993) Comparative three-dimensional analysis of CT-scans of the calvaria and cranial base in Apert and Crouzon syndromes. J Craniomaxillofac Surg 21:181–188. https://doi.org/10.1016/s1010-5182(05)80478-0
Rijken BFM, Lequin MH, Van Veelen M-LC et al (2015) The formation of the foramen magnum and its role in developing ventriculomegaly and Chiari I malformation in children with craniosynostosis syndromes. J Craniomaxillofac Surg 43:1042–1048. https://doi.org/10.1016/j.jcms.2015.04.025
Coll G, El Ouadih Y, Abed Rabbo F et al (2019) Hydrocephalus and Chiari malformation pathophysiology in FGFR2-related faciocraniosynostosis: a review. Neurochirurgie 65:264–268. https://doi.org/10.1016/j.neuchi.2019.09.001
Hoffman HJ, Tucker WS (1976) Cephalocranial disproportion. PNE 2:167–176. https://doi.org/10.1159/000119612
Coll G, Abed Rabbo F, Jecko V, Sakka L, di Rocco F, Delion M (2019) The growth of the posterior cranial fossa in FGFR2-induced faciocraniosynostosis: a review. Neurochirurgie 65:221–227. https://doi.org/10.1016/j.neuchi.2019.09.005
Machado G, Di Rocco F, Sainte-Rose C et al (2011) Cloverleaf skull deformity and hydrocephalus. Childs Nerv Syst 27:1683–1691. https://doi.org/10.1007/s00381-011-1508-8
Mavridis IN, Rodrigues D (2021) Nervous system involvement in Pfeiffer syndrome. Childs Nerv Syst 37:367–374. https://doi.org/10.1007/s00381-020-04934-7
Sainte-Rose C, LaCombe J, Pierre-Kahn A, Renier D, Hirsch JF (1984) Intracranial venous sinus hypertension: cause or consequence of hydrocephalus in infants? J Neurosurg 60:727–736. https://doi.org/10.3171/jns.1984.60.4.0727
Ghali GZ, Zaki Ghali MG, Ghali EZ, Srinivasan VM, Wagner KM, Rothermel A, Taylor J, Johnson J, Kan P, Lam S, Britz G (2019) Intracranial venous hypertension in craniosynostosis: mechanistic underpinnings and therapeutic implications. World Neurosurg 127:549–558. https://doi.org/10.1016/j.wneu.2018.07.260
Cinalli G, Spennato P, Sainte-Rose C, Arnaud E, Aliberti F, Brunelle F, Cianciulli E, Renier D (2005) Chiari malformation in craniosynostosis. Childs Nerv Syst 21:889–901. https://doi.org/10.1007/s00381-004-1115-z
Chen L, Elias G, Yostos MP, Stimec B, Fasel J, Murphy K (2015) Pathways of cerebrospinal fluid outflow: a deeper understanding of resorption. Neuroradiology 57:139–147. https://doi.org/10.1007/s00234-014-1461-9
Frassanito P, Di Rocco C (2020) Hydrocephalus: generalities and clinical presentations. In: Di Rocco C, Pang D, Rutka J (eds) Textbook of pediatric neurosurgery. Springer, Cham
Trevisi G, Frassanito P, Di Rocco C (2014) Idiopathic cerebrospinal fluid overproduction: case-based review of the pathophysiological mechanism implied in the cerebrospinal fluid production. Croat Med J 55:377–387
Chadduck WM, Chadduck JB, Boop FA (1992) The subarachnoid spaces in craniosynostosis. Neurosurgery 30:867–871. https://doi.org/10.1227/00006123-199206000-00008
Coll G, Arnaud E, Collet C, Brunelle F, Sainte-Rose C, di Rocco F (2015) Skull base morphology in fibroblast growth factor receptor type 2-related faciocraniosynostosis: a descriptive analysis. Neurosurgery 76:571–583; discussion 583. https://doi.org/10.1227/NEU.0000000000000676
Noetzel MJ, Marsh JL, Palkes H, Gado M (1985) Hydrocephalus and mental retardation in craniosynostosis. J Pediatr 107:885–892. https://doi.org/10.1016/S0022-3476(85)80181-5
Renier D, Arnaud E, Cinalli G, Sebag G, Zerah M, Marchac D (1996) Prognosis for mental function in Apert’s syndrome. J Neurosurg 85:66–72. https://doi.org/10.3171/jns.1996.85.1.0066
Hanieh A, David DJ (1993) Apert’s syndrome. Childs Nerv Syst 9:289–291. https://doi.org/10.1007/BF00306277
Kilcoyne S, Potter KR, Gordon Z, Overton S, Brockbank S, Jayamohan J, Magdum S, Smith M, Johnson D, Wall S, Wilkie AOM (2021) Feeding, communication, hydrocephalus, and intracranial hypertension in patients with severe FGFR2-associated Pfeiffer syndrome. J Craniofac Surg 32:134–140. https://doi.org/10.1097/SCS.0000000000007153
Murovic JA, Posnick JC, Drake JM, Humphreys RP, Hoffman HJ, Hendricks B (1993) Hydrocephalus in Apert syndrome: a retrospective review. Pediatr Neurosurg 19:151–155. https://doi.org/10.1159/000120720
Capra V, De Marco P, Merello E et al (2009) Craniosynostosis, hydrocephalus, Chiari I malformation and radioulnar synostosis: probably a new syndrome. Eur J Med Genet 52:17–22. https://doi.org/10.1016/j.ejmg.2008.10.005
Beltrami B, Prada E, Tolva G, Scuvera G, Silipigni R, Graziani D, Bulfamante G, Gervasini C, Marchisio P, Milani D (2020) Unexpected phenotype in a frameshift mutation of PTCH1. Mol Genet Genomic Med 8:e987. https://doi.org/10.1002/mgg3.987
Sakamoto K, Senda D, von Däniken S, Boztepe B, Komuro Y, Shimoji K (2021) Robinow syndrome in a newborn presenting with hydrocephalus and craniosynostosis. Childs Nerv Syst. https://doi.org/10.1007/s00381-021-05087-x
Tamburrini G, Caldarelli M, Massimi L, Santini P, di Rocco C (2005) Intracranial pressure monitoring in children with single suture and complex craniosynostosis: a review. Childs Nerv Syst 21:913–921. https://doi.org/10.1007/s00381-004-1117-x
Hayward R (2005) Venous hypertension and craniosynostosis. Childs Nerv Syst 21:880–888. https://doi.org/10.1007/s00381-004-1114-0
Lin LO, Zhang RS, Hoppe IC, Paliga JT, Swanson JW, Bartlett SP, Taylor JA (2019) Onset and resolution of Chiari malformations and hydrocephalus in syndromic craniosynostosis following posterior vault distraction. Plast Reconstr Surg 144:932–940. https://doi.org/10.1097/PRS.0000000000006041
Tamburrini G, Caldarelli M, Massimi L, Gasparini G, Pelo S, di Rocco C (2012) Complex craniosynostoses: a review of the prominent clinical features and the related management strategies. Childs Nerv Syst 28:1511–1523. https://doi.org/10.1007/s00381-012-1819-4
Di Rocco C, Frassanito P, Pelo S, Tamburrini G (2015) Syndromic craniosynostosis. In: Cohen AR (ed) Pediatric neurosurgery: tricks of the trade. Thieme Medical Publishers
Sandberg DI, Navarro R, Blanch J, Ragheb J (2007) Anomalous venous drainage preventing safe posterior fossa decompression in patients with Chiari malformation type I and multisutural craniosynostosis. Report of two cases and review of the literature. J Neurosurg 106:490–494. https://doi.org/10.3171/ped.2007.106.6.490
Frassanito P, Massimi L, Tamburrini G et al (2013) Occipital sinus pericranii superseding both jugular veins: description of two rare pediatric cases. Neurosurgery 72:E1054–E1058; dicussion 1058. https://doi.org/10.1227/NEU.0b013e31828baab4
Thompson DN, Hayward RD, Harkness WJ et al (1995) Lessons from a case of kleeblattschädel. Case report. J Neurosurg 82:1071–1074. https://doi.org/10.3171/jns.1995.82.6.1071
Copeland AE, Hoffman CE, Tsitouras V, Jeevan DS, Ho ES, Drake JM, Forrest CR (2018) Clinical significance of venous anomalies in syndromic craniosynostosis. Plast Reconstr Surg Glob Open 6:e1613. https://doi.org/10.1097/GOX.0000000000001613
Azzolini A, Magoon K, Yang R, Bartlett S, Swanson J, Taylor J (2020) Ventricular shunt complications in patients undergoing posterior vault distraction osteogenesis. Childs Nerv Syst 36:1009–1016. https://doi.org/10.1007/s00381-019-04403-w
Di Rocco C, Frassanito P (2014) Cranio-cerebral disproportion as a late complication. In: Di Rocco C, Turgut M, Jallo G, Martínez-Lage JF (eds) Complications of CSF shunting in hydrocephalus: prevention, identification, and management. Springer, Berlin
Sgulò FG, Spennato P, Aliberti F, di Martino G, Cascone D, Cinalli G (2017) Contemporary occurrence of hydrocephalus and Chiari I malformation in sagittal craniosynostosis. Case report and review of the literature. Childs Nerv Syst 33:187–192. https://doi.org/10.1007/s00381-016-3189-9
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that are no conflict of interest to disclose.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Frassanito, P., Palombi, D. & Tamburrini, G. Craniosynostosis and hydrocephalus: relevance and treatment modalities. Childs Nerv Syst 37, 3465–3473 (2021). https://doi.org/10.1007/s00381-021-05158-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-021-05158-z