Abstract
Purpose
To describe the potential issues in the methodology of surgical site infection (SSI) prevention and how it was investigated and corrected in a single institution.
Methods
A pediatric orthopedic unit experienced an increase of SSI, concerning up to 10% of scoliosis surgery cases from 2011 to 2013. An institutional procedure of multimodal and interdisciplinary risk evaluation was initiated, including a review of the literature, a morbi-mortality meeting, internal and external audits concerning the hygiene conditions in the operating room, the antibiotic prophylaxis, patients, and sterile material pathways. Several preventive actions were implemented, including the improvement of air treatment in the operating room, wound irrigation with 2L of saline before closure, application of topic vancomycine in the wound, verification of doses and timing of antibiotics injection, and use of waterproof bandages. We compared the rates of spine SSI before (retrospective group, 2011–2013) and after the implementation of various preventive measures (prospective group, 2014–2018).
Results
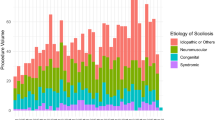
SSI occurred in 12 patients (6 idiopathic and 6 neuromuscular) out of 120 operated on (93 idiopathic, 18 neuromuscular, 9 others) in the retrospective group and 2 (both neuromuscular) out of 196 (150 idiopathic, 33 neuromuscular,13 others) in the prospective group (10% vs 1%, odds ratio=9.7, p=0.001). The groups were comparable for age, etiology, duration of surgery, body mass index, American Society of Anesthesiologists score, number of levels fused, and blood loss (p>0.2).
Conclusion
The systematic analysis of SSI allowed for the understanding of the failures and correcting them. The current process is effectively preventing SSI.
Level of evidence: 3: prospective series with case-control analysis
Similar content being viewed by others
References
Pourtaheri S, Miller F, Dabney K, Shah SA, Dubowy S, Holmes L (2015 Nov) Deep wound infections after pediatric scoliosis surgery. Spine Deform 3(6):533–540. https://doi.org/10.1016/j.jspd.2015.04.003
Warner SJ, Uppstrom TJ, Miller AO, O’Brien ST, Salvatore CM, Widmann RF, Perlman SL (2017 Feb) Epidemiology of deep surgical site infections after pediatric spinal fusion surgery. Spine (Phila Pa 1976) 42(3):E163–E168. https://doi.org/10.1097/BRS.0000000000001735
Labbé AC, Demers AM, Rodrigues R, Arlet V, Tanguay K, Moore DL (2003 Aug) Surgical-site infection following spinal fusion: a case-control study in a children’s hospital. Infect Control Hosp Epidemiol 24(8):591–595
McLeod L, Flynn J, Erickson M et al (2016) Variation in 60-day Readmission for Surgical-site Infections (SSIs) and Reoperation Following Spinal Fusion Operations for Neuromuscular Scoliosis. J Pediatr Orthop 36(6):634-9. https://doi.org/10.1097/BPO.0000000000000495
Newton PO, Bastrom TP, Yaszay B (2017) Patient-specific risk adjustment improves comparison of infection rates following posterior fusion for adolescent idiopathic scoliosis. J Bone Joint Surg Am 99(21) 1846\uc0\u8211{}50
Pesenti S, Blondel B, Peltier E, Launay F, Fuentes S, Bollini G, Viehweger E, Jouve JL (2016) Experience in perioperative management of patients undergoing posterior spine fusion for neuromuscular scoliosis. Biomed Res Int 2016:3053056–3053057. https://doi.org/10.1155/2016/3053056
Pull ter Gunne AF, Hosman AJ et al (2012) A methodological systematic review on surgical site infections following spinal surgery: part 1: risk factors. Spine (Phila Pa 1976) 37(24):2017–2033. https://doi.org/10.1097/BRS.0b013e31825bfca8
Abu-Bonsrah N, Goodwin CR, Ortega G, Abdullah F, Cornwell E, de la Garza-Ramos R, Groves ML, Ain M, Sponseller PD, Sciubba DM (2017) Risk factors associated with short-term complications and mortality after pediatric spinal arthrodesis. Neurosurg Focus 43(4):E7. https://doi.org/10.3171/2017.7.FOCUS17313
Subramanyam R, Schaffzin J, Cudilo EM, Rao MB, Varughese AM (2015) Systematic review of risk factors for surgical site infection in pediatric scoliosis surgery. Spine J 15(6):1422–1431. https://doi.org/10.1016/j.spinee.2015.03.005
Linam WM, Margolis PA, Staat MA, Britto MT, Hornung R, Cassedy A, Connelly BL (2009) Risk factors associated with surgical site infection after pediatric posterior spinal fusion procedure. Infect Control Hosp Epidemiol 30(2):109–116. https://doi.org/10.1086/593952
Milstone AM, Maragakis LL, Townsend T, Speck K, Sponseller P, Song X, Perl TM (2008) Timing of preoperative antibiotic prophylaxis: a modifiable risk factor for deep surgical site infections after pediatric spinal fusion. Pediatr Infect Dis J 27(8):704–708. https://doi.org/10.1097/INF.0b013e31816fca72
Gruenberg MF, Campaner GL, Sola CA, Ortolan EG (2004) Ultraclean air for prevention of postoperative infection after posterior spinal fusion with instrumentation: a comparison between surgeries performed with and without a vertical exponential filtered air-flow system. Spine (Phila Pa 1976) 29(20):2330–2334
Sabah Y, Clément JL, Solla F, Rosello O, Rampal V (2018) Cobalt-chrome and titanium alloy rods provide similar coronal and sagittal correction in adolescent idiopathic scoliosis. Orthop Traumatol Surg Res 104(7):1073–1077. https://doi.org/10.1016/j.otsr.2018.07.018
Allia J, Clément JL, Rampal V, Leloutre B, Rosello O, Solla F (2018) Influence of derotation connectors on 3D surgical correction of adolescent idiopathic scoliosis. Clin Spine Surg 31(3):E209–E215. https://doi.org/10.1097/BSD.0000000000000621
Vitale MG, Riedel MD, Glotzbecker MP et al (2013) Building consensus: development of a Best Practice Guideline (BPG) for surgical site infection (SSI) prevention in high-risk pediatric spine surgery. J Pediatr Orthop 33(5) 471\uc0\u8211{}8
Li Y, Glotzbecker M, Hedequist D (2012) Surgical site infection after pediatric spinal deformity surgery. Curr Rev Musculoskelet Med 5(2):111–119
Marks MC, Newton PO, Bastrom TP et al (2013) Surgical site infection in adolescent idiopathic scoliosis surgery. Spine Deform 1(5) 352\uc0\u8211{}8
McLeod LM, Keren R, Gerber J et al (2013) Perioperative antibiotic use for spinal surgery procedures in US children\uc0\u8217{}s hospitals. Spine 38(7) 609\uc0\u8211{}16
Verma K, Lonner B, Dean L et al (2013) Predictors of postoperative infection in spinal deformity surgery - which curves are at greatest risk? Bull Hosp Jt Dis 71(4) 257\uc0\u8211{}64
Solla F, Tran A, Bertoncelli D, Musoff C, Bertoncelli CM (2018) Why a P-value is not enough. Clin Spine Surg 31(9):385–388. https://doi.org/10.1097/BSD.0000000000000695
Ferreira KS, Lynch K, Ryder BA et al (2018. S1931-7204(17)30675-X) Lessons learned from the surgical morbidity and mortality conference. J Surg Educ. https://doi.org/10.1016/j.jsurg.2018.07.002
Himebauch AS, Sankar WN, Flynn JM et al (2016) Skeletal muscle and plasma concentrations of cefazolin during complex paediatric spinal surgery. Br J Anaesth 117(1) 87\uc0\u8211{}94
National Observatory of the Epidemiology of Bacterial Resistance to Antibiotics (ONERBA) (ONERBA) : Annual Report 2016. www.onerba.org. Accessed 12th March 2020
Hey HWD, Thiam DW, Koh ZSD et al (2017) Is intraoperative local vancomycin powder the answer to surgical site infections in spine surgery? Spine 42(4) 267\uc0\u8211{}74.
Acknowledgements
The authors thank Mrs. Martine Diez and Mrs. Sophie Gallot for clinical support. One author (FS) performed this research in the framework of the International PhD in Innovation Sciences and Technologies of the University of Cagliari, Italy.
Availability of data and material
Manuscript has no associate data.
Code availability
None
Author information
Authors and Affiliations
Contributions
FS conceived and performed the study and wrote the article. RL wrote the article and revised the literature. JLC supervised the study and revised the text. YL wrote the article, revised the literature, and collected data. IO revised the literature and revised the text. CMB performed the statistical analysis and revised the text. VR supervised the study and revised the text.
Corresponding authors
Ethics declarations
Ethics approval
This study was approved by IRB “South-East France” with number 2012-A01663-40, ref 13.003, and protocol 72082012. The authors confirms that the study was approved by the appropriate institutional research ethics committee and certify that the study was performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Consent to participate
Informed consent was obtained by all patients and parents.
Consent for publication
All authors consent for publication.
Conflict of interest
Federico Solla and Jean-Luc Clément received funding for attending congresses from Medicrea Int outside this work. The other authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Solla, F., Lefèbvre, R., Clément, JL. et al. Prevention of surgical site infections in pediatric spines: a single-center experience. Childs Nerv Syst 37, 2299–2304 (2021). https://doi.org/10.1007/s00381-021-05095-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-021-05095-x