Abstract
Purpose
Multidisciplinary team meetings (MDTMs) are essential in the clinical management of pediatric central nervous system (CNS) tumors. Evaluations of the impact of MDTMs on childhood CNS tumors and clinicians’ perspectives on their effectiveness are scarce.
Methods
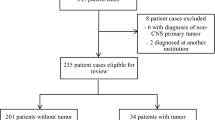
We retrospectively reviewed the clinical data of pediatric patients (aged <18 years) with CNS tumors diagnosed and treated in the Pediatric Hematology-Oncology Division at the University Malaya Medical Center from 2008 to 2019. We also conducted a web-based survey of the core members of the multidisciplinary team to evaluate the impact of the MDTMs.
Results
During the pre-MDTM era (2008–2012), 29 CNS tumors were diagnosed and treated, and during the MDTM era (2014–2019), 49 CNS tumors were diagnosed and treated. The interval for histologic diagnosis was significantly shorter during the MDTM era (p=0.04), but the interval from diagnosis to chemotherapy or radiotherapy and the 5-year overall survival of the 78 patients did not improve (62.1% ± 9.0% vs. 68.8% ± 9.1%; p=0.184). However, the 5-year overall survival of patients with medulloblastoma or rare tumors significantly improved in the MDTM era (p=0.01). Key factors that contributed to delayed treatment and poor outcomes were postoperative complications, the facility’s lack of infrastructure, poor parental education about early treatment, cultural beliefs in alternative medicine, and infection during chemotherapy. Eighteen clinicians responded to the survey; they felt that the MDTMs were beneficial in decision-making and enhanced the continuity of coordinated care.
Conclusion
MDTMs significantly reduced the diagnostic interval and improved the overall outcomes. However, delayed treatment remains a major challenge that requires further attention.




Similar content being viewed by others
Data availability
All relevant data are available in the paper.
References
Girardi F, Allemani C, Coleman MP (2019) Worldwide trends in survival from common childhood brain tumors: a systematic review. J Glob Oncol 5:1–25
Zaghloul MS (2016) Single pediatric neuro-oncology center may make difference in low/middle-income countries. Childs Nerv Syst 32:241–242
Allemani C, Matsuda T, Di Carlo V, Harewood R, Matz M, Niksic M, Bonaventure A, Valkov M, Johnson CJ, Esteve J, Ogunbiyi OJ, Azevedo ESG, Chen WQ, Eser S, Engholm G, Stiller CA, Monnereau A, Woods RR, Visser O, Lim GH, Aitken J, Weir HK, Coleman MP, Group CW (2018) Global surveillance of trends in cancer survival 2000-14 (CONCORD-3): analysis of individual records for 37 513 025 patients diagnosed with one of 18 cancers from 322 population-based registries in 71 countries. Lancet 391:1023–1075
Calman KC, Hine D (1995) A report by the expert advisory group on cancer to the chief medical officers of England and Wales. a policy framework for Comissioning Cancer Services (The Calman-Hine Report) London Department of Health
NICE (2006) Improving outcomes for people with brain and other CNS tumours. London: National Institute of Health and Clinical Excellence
Pillay B, Wootten AC, Crowe H, Corcoran N, Tran B, Bowden P, Crowe J, Costello AJ (2016) The impact of multidisciplinary team meetings on patient assessment, management and outcomes in oncology settings: A systematic review of the literature. Cancer Treat Rev 42:56–72
Brannstrom F, Bjerregaard JK, Winbladh A, Nilbert M, Revhaug A, Wagenius G, Morner M (2015) Multidisciplinary team conferences promote treatment according to guidelines in rectal cancer. Acta Oncol 54:447–453
Prades J, Remue E, van Hoof E, Borras JM (2015) Is it worth reorganising cancer services on the basis of multidisciplinary teams (MDTs)? A systematic review of the objectives and organisation of MDTs and their impact on patient outcomes. Health Policy (Amsterdam, Netherlands) 119:464–474
Freeman RK, Ascioti AJ, Dake M, Mahidhara RS (2015) The effects of a multidisciplinary care conference on the quality and cost of care for lung cancer patients. Ann Thorac Surg 100:1834–1838 discussion 1838
Pan C-C, Kung P-T, Wang Y-H, Chang Y-C, Wang S-T, Tsai W-C (2015) Effects of multidisciplinary team care on the survival of patients with different stages of non-small cell lung cancer: a national cohort study. PLoS One 10:e0126547
Munro A, Brown M, Niblock P, Steele R, Carey F (2015) Do Multidisciplinary Team (MDT) processes influence survival in patients with colorectal cancer? A population-based experience. BMC Cancer 15:686
Keating NL, Landrum MB, Lamont EB, Bozeman SR, Shulman LN, McNeil BJ (2013) Tumor boards and the quality of cancer care. J Natl Cancer Inst 105:113–121
Davies AR, Deans DA, Penman I, Plevris JN, Fletcher J, Wall L, Phillips H, Gilmour H, Patel D, de Beaux A, Paterson-Brown S (2006) The multidisciplinary team meeting improves staging accuracy and treatment selection for gastro-esophageal cancer. Dis Esophagus 19:496–503
McNair AG, Choh CT, Metcalfe C, Littlejohns D, Barham CP, Hollowood A, Falk SJ, Blazeby JM (2008) Maximising recruitment into randomised controlled trials: the role of multidisciplinary cancer teams. Eur J Cancer 44:2623–2626
Twelves CJ, Thomson CS, Young J, Gould A (1998) Entry into clinical trials in breast cancer: the importance of specialist teams. Eur J Cancer 34:1004–1007
Gabel M, Hilton NE, Nathanson SD (1997) Multidisciplinary breast cancer clinics. Do they work? Cancer 79:2380–2384
Goodden JR, Yeomanson D, Zaki HS, Lee V, McMullan PJ (2009) Care of children with brain and spine tumours - a review of practice. Br J Neurosurg 23:270–275
Guilfoyle MR, Weerakkody RA, Oswal A, Oberg I, Jeffery C, Haynes K, Kullar PJ, Greenberg D, Jefferies SJ, Harris F, Price SJ, Thomson S, Watts C (2011) Implementation of neuro-oncology service reconfiguration in accordance with NICE guidance provides enhanced clinical care for patients with glioblastoma multiforme. Br J Cancer 104:1810–1815
Field KM, Rosenthal MA, Dimou J, Fleet M, Gibbs P, Drummond K (2010) Communication in and clinician satisfaction with multidisciplinary team meetings in neuro-oncology. J Clin Neurosci 17:1130–1135
Qaddoumi I, Musharbash A, Elayyan M, Mansour A, Al-Hussaini M, Drake J, Swaidan M, Bartels U, Bouffet E (2008) Closing the survival gap: implementation of medulloblastoma protocols in a low-income country through a twinning program. Int J Cancer 122:1203–1206
Qaddoumi I, Mansour A, Musharbash A, Drake J, Swaidan M, Tihan T, Bouffet E (2007) Impact of telemedicine on pediatric neuro-oncology in a developing country: the Jordanian-Canadian experience. Pediatr Blood Cancer 48:39–43
Raine R, Wallace I, Nic a’ Bhaird C, Xanthopoulou P, Lanceley A, Clarke A, Prentice A, Ardron D, Harris M, Gibbs JSR, Ferlie E, King M, Blazeby JM, Michie S, Livingston G, Barber J (2014) Improving the effectiveness of multidisciplinary team meetings for patients with chronic diseases: a prospective observational study, Southampton (UK)
Soukup T, Lamb BW, Arora S, Darzi A, Sevdalis N, Green JS (2018) Successful strategies in implementing a multidisciplinary team working in the care of patients with cancer: an overview and synthesis of the available literature. J Multidiscip Healthc 11:49–61
Bydder S, Nowak A, Marion K, Phillips M, Atun R (2009) The impact of case discussion at a multidisciplinary team meeting on the treatment and survival of patients with inoperable non-small cell lung cancer. Intern Med J 39:838–841
Ameratunga M, Miller D, Ng W, Wada M, Gonzalvo A, Cher L, Gan HK (2018) A single-institution prospective evaluation of a neuro-oncology multidisciplinary team meeting. J Clin Neurosci 56:127–130
Patkar V, Acosta D, Davidson T, Jones A, Fox J, Keshtgar M (2011) Cancer multidisciplinary team meetings: evidence, challenges, and the role of clinical decision support technology. Int J Breast Cancer 2011:831605
Macaskill EJ, Thrush S, Walker EM, Dixon JM (2006) Surgeons’ views on multi-disciplinary breast meetings. Eur J Cancer 42:905–908
Acknowledgements
We thank Dr. Angela McArthur for the scientific editing of this manuscript.
Author information
Authors and Affiliations
Contributions
Revathi Rajagopal, Tsiao Yi Yap, Jasmin Loh, Nicholas G. Gottardo, Daniel C Moreira, and Ibrahim Qaddoumi designed the study. Jen Chun Foo and Vida Jawin collected the data. Nor Faizal Ahmad Bahuri, Dharmendra Ganesan, Kein Seong Mun, and Jen Chun Foo coordinated the web-based cross-sectional survey. Revathi Rajagopal and Daniel C Moreira analyzed the data. Jen Chun, Vida Jawin, Daniel Moreira, and Revathi Rajagopal drafted the manuscript. All authors reviewed and revised the manuscript.
Corresponding author
Ethics declarations
Ethics approval
Study approval was obtained from the University Malaya Medical Center Medical Research Ethics Committee for patient data collection (MREC ID: 201914-6968). The UMMC Ethics Committee waived the need for written informed consent from patients and families.
Conflict of interest
The authors have no conflicts of interest to declare.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This report is from a Global Alliance Pediatric Neuro-Oncology quality improvement project conducted at the University Malaya Medical Center, Kuala Lumpur, Malaysia. Clinicians from various departments and centers participated in this study.
Supplementary Information
ESM 1
(DOCX 86 kb)
Rights and permissions
About this article
Cite this article
Foo, J.C., Jawin, V., Yap, T.Y. et al. Conduct of neuro-oncology multidisciplinary team meetings and closing the “gaps” in the clinical management of childhood central nervous system tumors in a middle-income country. Childs Nerv Syst 37, 1573–1580 (2021). https://doi.org/10.1007/s00381-021-05080-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-021-05080-4