Abstract
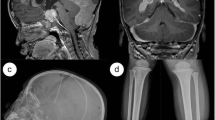
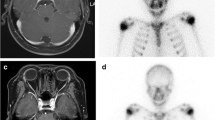
Histiocytosis is a heterogeneous group of disease entities, comprised by two main categories, namely Langerhans and non-Langerhans cell histiocytoses. Central nervous system involvement in histiocytosis is considered very rare and is often secondary to affection of anatomically related bone structures and/or multi-organ disease. We present a never-before described case of rare childhood histiocytosis with hybrid features of Langerhans cell histiocytosis and juvenile xanthogranuloma confined to the central nervous system in a 2- and a half-year-old boy with distinct treatment response to clofarabine. The case also emphasizes the diagnostic significance of stereotactic brain biopsy.



Similar content being viewed by others
References
Jaffe R (2005) The diagnostic histopathology of Langerhans cell histiocytosis. In: Histiocytic disorders of children and adults. Basic Science, Clinical Features and Therapy. Cambridge University Press
Carstensen H, Ornvold K (1993) The epidemiology of LCH in children in Denmark, 1975–89. Med Pediatr Oncol 21:387–388
Grois N, Pötschger U, Prosch H, Minkov M, Arico M, Braier J, Henter JI, Janka-Schaub G, Ladisch S, Ritter J, Steiner M, Unger E, Gadner H, for the DALHX- and LCH I and II Study Committee (2006) Risk factors for diabetes insipidus in Langerhans cell histiocytosis. Pediatr Blood Cancer 46:228–233. https://doi.org/10.1002/pbc.20425
Prayer D, Grois N, Prosch H, Gadner H, Barkovich AJ (2004) MR imaging presentation of intracranial disease associated with Langerhans cell histiocytosis. AJNR Am J Neuroradiol 25:880–891
El DD, Young JL, De NJ et al (2015) Langerhans cell histiocytosis: a comprehensive review. Pathology 47:294–301. https://doi.org/10.1097/PAT.0000000000000256
Grois N, Prayer D, Prosch H, Lassmann H (2005) Neuropathology of CNS disease in Langerhans cell histiocytosis. Brain 128:829–838. https://doi.org/10.1093/brain/awh403
Janssen D, Harms D (2005) Juvenile xanthogranuloma in childhood and adolescence: a clinicopathologic study of 129 patients from the kiel pediatric tumor registry. Am J Surg Pathol 29:21–28
Dehner LP (2003) Juvenile xanthogranulomas in the first two decades of life: a clinicopathologic study of 174 cases with cutaneous and extracutaneous manifestations. Am J Surg Pathol 27:579–593
Chen W, Cheng Y, Zhou S, Chen Y, Chen X, Xia S (2017) Juvenile xanthogranuloma of central nervous system: imaging of two cases report and literature review. Radiol Infect Dis 4:117–120. https://doi.org/10.1016/J.JRID.2017.08.009
Skjøth-Rasmussen J, Jespersen B, Brennum J (2015) The use of Brainsuite iCT for frame-based stereotactic procedures. Acta Neurochir 157:1437–1440. https://doi.org/10.1007/s00701-015-2475-8
Simko SJ, Tran HD, Jones J, Bilgi M, Beaupin LK, Coulter D, Garrington T, McCavit TL, Moore C, Rivera-Ortegón F, Shaffer L, Stork L, Turcotte L, Welsh EC, Hicks MJ, McClain KL, Allen CE (2014) Clofarabine salvage therapy in refractory multifocal histiocytic disorders, including Langerhans cell histiocytosis, juvenile xanthogranuloma and Rosai-Dorfman disease. Pediatr Blood Cancer 61:479–487. https://doi.org/10.1002/pbc.24772
Strehl JD, Stachel K-D, Hartmann A, Agaimy A (2012) Juvenile xanthogranuloma developing after treatment of Langerhans cell histiocytosis: case report and literature review. Int J Clin Exp Pathol 5:720–725
Hoeger PH, Diaz C, Malone M, Pritchard J, Harper JI (2001) Juvenile xanthogranuloma as a sequel to Langerhans cell histiocytosis: a report of three cases. Clin Exp Dermatol 26:391–394
Patrizi A, Neri I, Bianchi F, Guerrini V, Misciali C, Paone G, Burnelli R (2004) Langerhans cell histiocytosis and juvenile xanthogranuloma. Dermatology 209:57–61. https://doi.org/10.1159/000078589
Pérez-Gala S, Torrelo A, Colmenero I, Contra T, Madero L, Zambrano A (2006) Juvenile multiple xanthogranuloma in a patient with Langerhans cell histiocytosis. Actas Dermosifiliogr 97:594–598
Bains A, Parham DM (2011) Langerhans cell histiocytosis preceding the development of juvenile xanthogranuloma: a case and review of recent developments. Pediatr Dev Pathol 14:480–484. https://doi.org/10.2350/10-12-0950-CR.1
Acknowledgements
We would like to acknowledge Dr. Jennifer Picarsic, Children’s Hospital of Pittsburgh, University of Pittsburgh Medical Center, for her important contribution to the pathological examination and diagnosis.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there are no conflicts of interest.
Rights and permissions
About this article
Cite this article
Foss-Skiftesvik, J., Scheie, D., Klausen, C. et al. Rare childhood hybrid histiocytosis of the central nervous system—diagnosed by stereotactic brain biopsy with marked treatment response to clofarabine. Childs Nerv Syst 34, 2321–2324 (2018). https://doi.org/10.1007/s00381-018-3859-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-018-3859-x