Abstract
Purpose
The purpose of this paper is to study invasiveness, tumor features and clinical symptoms of pediatric pituitary adenoma, and to discuss some inconclusive results in prior studies.
Methods
We retrospectively reviewed 34 cases of children (<20 year-old) who were pathologically diagnosed with pituitary adenoma and surgically treated from 2010 to 2017. Data of general information, clinical symptoms, invasive behaviors, surgery approaches, and tumor features were collected and analyzed.
Results
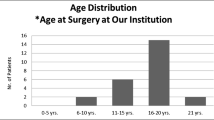
Sixteen boys and 18 girls aged from 12 to 19 years old were included. Prolactinoma was most suffered, followed by GH-, none- and ACTH-secreting pituitary adenoma. Invasive behaviors were observed frequently and suprasellar extensions were most found. Macroadenoma account 70% of all cases. Meanwhile, unlike prior studies, a significant raise of incidence on invasive tumor and pituitary adenoma apoplexy were observed. Craniotomy and transsphenoidal surgery were both applied with zero mortality. Nine cases occurred with transient hypopituitarism and diabetes insipidus. Three cases of tumor recurrence received secondary surgery or radiotherapy.
Conclusions
Invasive behaviors were more frequent than previous prediction. Craniotomy is worth considering for total tumor removal. Pituitary adenoma apoplexy needs further studies since its different features between children and adults in present study. Specialized care and teamwork of neurosurgeons, pediatricians, and endocrinologists are important.



Similar content being viewed by others
References
Wong TT, Ho DM, Chang KP, Yen SH, Guo WY, Chang FC, Liang ML, Pan HC, Chung WY (2005) Primary pediatric brain tumors: statistics of Taipei VGH, Taiwan (1975-2004). Cancer 104(10):2156–2167. doi:10.1002/cncr.21430
Zhang R, Shen WQ, Zhou LF (2007) Primary pediatric central nervous system tumors statistic: study of 763 cases in a single institution. Zhonghua Yi Xue Za Zhi 87(7):442–447
McCrea HJ, George E, Settler A, Schwartz TH, Greenfield JP (2016) Pediatric suprasellar tumors. J Child Neurol 31(12):1367–1376. doi:10.1177/0883073815620671
Ortiz-Suarez H, Erickson DL (1975) Pituitary adenomas of adolescents. J Neurosurg 43(4):437–439. doi:10.3171/jns.1975.43.4.0437
Kunwar S, Wilson CB (1999) Pediatric pituitary adenomas. J Clin Endocrinol Metab 84(12):4385–4389. doi:10.1210/jcem.84.12.6240
Fraioli B, Ferrante L, Celli P (1983) Pituitary adenomas with onset during puberty. Features Treat J Neurosurg 59(4):590–595. doi:10.3171/jns.1983.59.4.0590
Mindermann T, Wilson CB (1995) Pediatric pituitary adenomas. Neurosurgery 36(2):259–268; discussion 269
Richmond IL, Wilson CB (1978) Pituitary adenomas in childhood and adolescence. J Neurosurg 49(2):163–168. doi:10.3171/jns.1978.49.2.0163
Maira G, Anile C (1990) Pituitary adenomas in childhood and adolescence. Can J Neurol Sci J Can Sci Neurol 17(1):83–87
Partington MD, Davis DH, Laws ER Jr, Scheithauer BW (1994) Pituitary adenomas in childhood and adolescence. Results Transsphenoidal Surg J Neurosurg 80(2):209–216. doi:10.3171/jns.1994.80.2.0209
Kane LA, Leinung MC, Scheithauer BW, Bergstralh EJ, Laws ER Jr, Groover RV, Kovacs K, Horvath E, Zimmerman D (1994) Pituitary adenomas in childhood and adolescence. J Clin Endocrinol Metab 79(4):1135–1140. doi:10.1210/jcem.79.4.7525627
Dyer EH, Civit T, Visot A, Delalande O, Derome P (1994) Transsphenoidal surgery for pituitary adenomas in children. Neurosurgery 34(2):207–212; discussion 212
Pandey P, Ojha BK, Mahapatra AK (2005) Pediatric pituitary adenoma: a series of 42 patients. J Clin Neurosci: Off J Neurosurg Soc Australas 12(2):124–127. doi:10.1016/j.jocn.2004.10.003
Mehrazin M (2007) Pituitary tumors in children: clinical analysis of 21 cases. Childs Nerv Syst: ChNS: Off J Int Soc Pediatr Neurosurg 23(4):391–398. doi:10.1007/s00381-006-0259-4
Webb C, Prayson RA (2008) Pediatric pituitary adenomas. Arch Pathol Lab Med 132(1):77–80. doi:10.1043/1543-2165(2008)132[77:ppa]2.0.co;2
Taskapilioglu MO, Yilmazlar S, Eren E, Tarim O, Guler TM (2015) Transnasal transsphenoidal surgical method in pediatric pituitary adenomas. Pediatr Neurosurg 50(3):128–132. doi:10.1159/000381862
Zhenye L, Chuzhong L, Youtu W, Xiaolei L, Lei C, Lichuan H, Hongyun W, Yonggang W, Fei W, Yazhuo Z (2014) The expression of TGF-beta1, Smad3, phospho-Smad3 and Smad7 is correlated with the development and invasion of nonfunctioning pituitary adenomas. J Transl Med 12:71. doi:10.1186/1479-5876-12-71
Nawar RN, AbdelMannan D, Selman WR, Arafah BM (2008) Pituitary tumor apoplexy: a review. J Intensive Care Med 23(2):75–90. doi:10.1177/0885066607312992
Micko AS, Wohrer A, Wolfsberger S, Knosp E (2015) Invasion of the cavernous sinus space in pituitary adenomas: endoscopic verification and its correlation with an MRI-based classification. J Neurosurg 122(4):803–811. doi:10.3171/2014.12.jns141083
Xing B, Kong YG, Yao Y, Lian W, Wang RZ, Ren ZY (2013) Study on the expression levels of CXCR4, CXCL12, CD44, and CD147 and their potential correlation with invasive behaviors of pituitary adenomas. Biomed Environ Sci: BES 26(7):592–598. doi:10.3967/0895-3988.2013.07.011
Sakalas R, David RB, Vines FS, Becker DP (1973) Pituitary apoplexy in a child. Case Rep J Neurosurg 39(4):519–522. doi:10.3171/jns.1973.39.4.0519
Banerjee C, Snelling B, Hanft S, Komotar RJ (2015) Bilateral cerebral infarction in the setting of pituitary apoplexy: a case presentation and literature review. Pituitary 18(3):352–358. doi:10.1007/s11102-014-0581-x
Verrees M, Arafah BM, Selman WR (2004) Pituitary tumor apoplexy: characteristics, treatment, and outcomes. Neurosurg Focus 16(4):E6
Kruse A, Astrup J, Cold GE, Hansen HH (1992) Pressure and blood flow in pituitary adenomas measured during transsphenoidal surgery. Br J Neurosurg 6(4):333–341
Briet C, Salenave S, Bonneville JF, Laws ER, Chanson P (2015) Pituitary apoplexy. Endocr Rev 36(6):622–645. doi:10.1210/er.2015-1042
Maccagnan P, Macedo CL, Kayath MJ, Nogueira RG, Abucham J (1995) Conservative management of pituitary apoplexy: a prospective study. J Clin Endocrinol Metab 80(7):2190–2197. doi:10.1210/jcem.80.7.7608278
Tu M, Lu Q, Zhu P, Zheng W (2016) Surgical versus non-surgical treatment for pituitary apoplexy: a systematic review and meta-analysis. J Neurol Sci 370:258–262. doi:10.1016/j.jns.2016.09.047
Rajasekaran S, Vanderpump M, Baldeweg S, Drake W, Reddy N, Lanyon M, Markey A, Plant G, Powell M, Sinha S, Wass J (2011) UK guidelines for the management of pituitary apoplexy. Clin Endocrinol 74(1):9–20. doi:10.1111/j.1365-2265.2010.03913.x
Haddad SF, VanGilder JC, Menezes AH (1991) Pediatric pituitary tumors. Neurosurgery 29(4):509–514
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was funded by the Department of Science and Technology of Sichuan Province (2016SZ0015).
Conflict of interest
All authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of West China Hospital, Sichuan University, and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Zhang, N., Zhou, P., Meng, Y. et al. A retrospective review of 34 cases of pediatric pituitary adenoma. Childs Nerv Syst 33, 1961–1967 (2017). https://doi.org/10.1007/s00381-017-3538-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-017-3538-3