Abstract
Objectives
Surgical management of cranial burst fracture (CBF) usually involves craniotomy to remove the devitalized brain tissues, followed by watertight repair of dural tears. However, there were times when the dural tear was so extensive that a substantially large bone flap would have to be removed in order to expose the retracted dural margins before it could be repaired. In such cases, strict dural repair would incur a significantly higher risk of damages to the surrounding neural tissues and severe bleeding, especially when the fracture was in the vicinity of eloquent cortical areas and sinus. Basing on our own clinical experiences, we suggest strict dural closure is not mandatory for these selected patients.
Methods
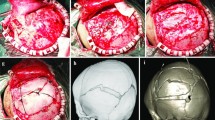
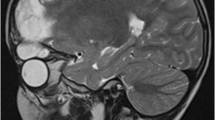
A retrospective review of patients who underwent cranial surgery for CBF at our hospital was performed. Computed tomography (CT) and magnetic resonance imaging (MRI) scans were performed to evaluate the extent of dural and brain laceration and the existence of extra-cranial cerebral tissues. Routine craniotomy was delivered to remove the lacerated brain tissues and evacuate the hematoma. The dural defect was only partially fixed with patient’s own tissues or artificial dura patch. Then the fractured bone flaps were restored using titanium micro plates and screws. Data including preoperative neurological status, surgery related complications, postoperative cranial fracture healing, and clinical outcomes were obtained through clinical and radiological examinations.
Results
From October 2004 to March 2013, a total of four patients diagnosed with CBF were treated by this dural closure sparing technique. Their average age was 18.4 months old and the average area of the skull defects was 91 cm2, with an average interval between primary injury and surgery of 13 days. The diagnosis of CBF was confirmed by intraoperative findings like extrusion of cerebral tissues out of the lacerated dura mater and skull defects. The postoperative courses were uneventful and all patients’ neurological functions improved after surgery. Postoperative three dimensional CT reconstruction of the cranial vault showed the skull fractures healed properly in all patients. No patient developed posttraumatic cerebrospinal fluid leak or epilepsy during the on average 24-month follow-up period.
Conclusions
In those selected cases of CBF in whom an extraordinary large craniotomy would be required to expose the entire retracted dura margins, given satisfactory evacuation of devitalized brain tissues and restoration of the bone flaps were achieved, we suggest strict dura closure is not compulsory.



Similar content being viewed by others
References
Ciurea AV, Gorgan MR, Tascu A, Sandu AM, Rizea RE (2011) Traumatic brain injury in infants and toddlers, 0-3 years old. J Med Life 4:234–243
Demellweek C, Baldwin T, Appleton R, Al-Kharusi A (2002) A prospective study and review of pre-morbid characteristics in children with traumatic brain injury. Pediatr Rehabil 5:81–89. doi:10.1080/136384902320807194
Donahue DJ, Sanford RA, Muhlbauer MS, Chadduck WM (1995) Cranial burst fracture in infants: acute recognition and management. Childs Nerv Syst 11:692–697
Ellis TS, Vezina LG, Donahue DJ (2000) Acute identification of cranial burst fracture: comparison between CT and MR imaging findings. AJNR Am J Neuroradiol 21:795–801
Liu XS, You C, Lu M, Liu JG (2012) Growing skull fracture stages and treatment strategy. J Neurosurg Pediatr 9:670–675. doi:10.3171/2012.2.PEDS11538
Lloyd O, Ownsworth T, Fleming J, Zimmer-Gembeck MJ (2015) Awareness deficits in children and adolescents after traumatic brain injury: a systematic review. J Head Trauma Rehabil. doi:10.1097/HTR.0000000000000113
Matsuura H, Omama S, Yoshida Y, Fujiwara S, Honda T, Akasaka M, Kamei A, Ogasawara K (2012) Use of magnetic resonance imaging to identify the edge of a dural tear in an infant with growing skull fracture: a case study. Childs Nerv Syst 28:1951–1954. doi:10.1007/s00381-012-1891-9
Muhonen MG, Piper JG, Menezes AH (1995) Pathogenesis and treatment of growing skull fractures. Surg Neurol 43:367–372 discussion 372-363
Oehmichen M, Meissner C, Saternus KS (2005) Fall or shaken: traumatic brain injury in children caused by falls or abuse at home—a review on biomechanics and diagnosis. Neuropediatrics 36:240–245. doi:10.1055/s-2005-872812
Pinto PS, Meoded A, Poretti A, Tekes A, Huisman TA (2012) The unique features of traumatic brain injury in children. Review of the characteristics of the pediatric skull and brain, mechanisms of trauma, patterns of injury, complications, and their imaging findings—part 2. J Neuroimaging 22:e18–e41. doi:10.1111/j.1552-6569.2011.00690.x
Pinto PS, Poretti A, Meoded A, Tekes A, Huisman TA (2012) The unique features of traumatic brain injury in children. Review of the characteristics of the pediatric skull and brain, mechanisms of trauma, patterns of injury, complications and their imaging findings—part 1. J Neuroimaging 22:e1–e17. doi:10.1111/j.1552-6569.2011.00688.x
Prasad GL, Gupta DK, Mahapatra AK, Borkar SA, Sharma BS (2015) Surgical results of growing skull fractures in children: a single centre study of 43 cases. Childs Nerv Syst 31:269–277. doi:10.1007/s00381-014-2529-x
Reddy DR (2013) Growing skull fractures: guidelines for early diagnosis and effective operative management. Neurol India 61:455–456. doi:10.4103/0028-3886.121907
Sanford RA (2010) Prevention of growing skull fractures: report of 2 cases. J Neurosurg Pediatr 5:213–218. doi:10.3171/2009.9.PEDS09180
Scarfo GB, Mariottini A, Tomaccini D, Palma L (1989) Growing skull fractures: progressive evolution of brain damage and effectiveness of surgical treatment. Childs Nerv Syst 5:163–167
Singhal A, Steinbok P (2008) Operative management of growing skull fractures: a technical note. Childs Nerv Syst 24:605–607. doi:10.1007/s00381-007-0552-x
Thurman DJ (2014) The epidemiology of traumatic brain injury in children and youths: a review of research since 1990. J Child Neurol. doi:10.1177/0883073814544363
Vignes JR, Jeelani N, Dautheribes M, San-Galli F, Liguoro D (2007) Cranioplasty for repair of a large bone defect in a growing skull fracture in children. J Craniomaxillofac Surg 35:185–188. doi:10.1016/j.jcms.2007.04.002
Wang X, Li G, Li Q, You C (2013) Early diagnosis and treatment of growing skull fracture. Neurol India 61:497–500. doi:10.4103/0028-3886.121918
Winkler R, Taylor NF (2015) Do children and adolescents with mild traumatic brain injury and persistent symptoms benefit from treatment? A systematic review. J Head Trauma Rehabil. doi:10.1097/HTR.0000000000000114
Yang CH, Li Q, Li GP, You C (2009) Internal open brain injury or cranial burst fracture: report of 8 cases. Pediatr Neurosurg 45:402–406. doi:10.1159/000260912
Acknowledgment
We would like to thank Mr. Xiaofeng Ni from Puqi Middle School, Yueqing, Wenzhou, Zhejiang, China for his generous helps in preparation of the Fig. 1 artwork in this manuscript. The authors declare that they have no conflict of interest. This study is funded by Science Technology Department of Zhejiang Province (Grant No. 2015C33144).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Approval to conduct this study was obtained from the Medical Ethics Committee of the Second Affiliated Hospital of Wenzhou Medical University.
Conflict of interest
None of the authors has any potential conflict of interest.
Rights and permissions
About this article
Cite this article
Sheng, Hs., Zhang, N., Lin, J. et al. Delayed surgical repair of cranial burst fracture without strict dura closure: a prudent choice in selected patients?. Childs Nerv Syst 32, 1661–1667 (2016). https://doi.org/10.1007/s00381-016-3155-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-016-3155-6