Abstract
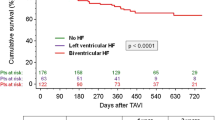
Aortic regurgitation (AR) following continuous flow left ventricular assist device implantation (cf-LVAD) may adversely impact outcomes. We aimed to assess the incidence and impact of progressive AR after cf-LVAD on prognosis, biomarkers, functional capacity and echocardiographic findings. In an analysis of the PCHF-VAD database encompassing 12 European heart failure centers, patients were dichotomized according to the progression of AR following LVAD implantation. Patients with de-novo AR or AR progression (AR_1) were compared to patients without worsening AR (AR_0). Among 396 patients (mean age 53 ± 12 years, 82% male), 153 (39%) experienced progression of AR over a median of 1.4 years on LVAD support. Before LVAD implantation, AR_1 patients were less frequently diabetic, had lower body mass indices and higher baseline NT-proBNP values. Progressive AR did not adversely impact mortality (26% in both groups, HR 0.91 [95% CI 0.61–1.36]; P = 0.65). No intergroup variability was observed in NT-proBNP values and 6-minute walk test results at index hospitalization discharge and at 6-month follow-up. However, AR_1 patients were more likely to remain in NYHA class III and had worse right ventricular function at 6-month follow-up. Lack of aortic valve opening was related to de-novo or worsening AR (P < 0.001), irrespective of systolic blood pressure (P = 0.67). Patients commonly experience de-novo or worsening AR when exposed to continuous flow of contemporary LVADs. While reducing effective forward flow, worsening AR did not influence survival. However, less complete functional recovery and worse RV performance among AR_1 patients were observed. Lack of aortic valve opening was associated with progressive AR.



Similar content being viewed by others
References
Crespo-Leiro MG, Metra M, Lund LH, Milicic D, Costanzo MR, Filippatos G, Gustafsson F, Tsui S, Barge-Caballero E, De Jonge N, Frigerio M, Hamdan R, Hasin T, Hülsmann M, Nalbantgil S, Potena L, Bauersachs J, Gkouziouta A, Ruhparwar A, Ristic AD, Straburzynska-Migaj E, McDonagh T, Seferovic P, Ruschitzka F (2018) Advanced heart failure: a position statement of the Heart Failure Association of the European Society of Cardiology. Eur J Heart Fail 20:1505–1535
Mehra MR (2019) The burden of hemocompatibility with left ventricular assist systems: a complex weave. Eur Heart J 40:673–677
Gasparovic H, Kopjar T, Saeed D, Cikes M, Svetina L, Petricevic M, Lovric D, Milicic D, Biocina B (2017) De novo aortic regurgitation after continuous-flow left ventricular assist device implantation. Ann Thorac Surg 104:704–711
Bouabdallaoui N, El-Hamamsy I, Pham M, Giraldeau G, Parent MC, Carrier M, Rouleau JL, Ducharme A (2018) Aortic regurgitation in patients with a left ventricular assist device: a contemporary review. J Heart Lung Transplant 37:1289–1297
Imamura T, Kim G, Nitta D, Fujino T, Smith B, Kalantari S, Nguyen A, Narang N, Holzhauser L, Grinstein J, Juricek C, Rodgers D, Song T, Ota T, Jeevanandam V, Sayer G, Uriel N (2019) Aortic insufficiency and hemocompatibility-related adverse events in patients with left ventricular assist devices. J Card Fail 25:787–794
Martina JR, Schipper ME, de Jonge N, Ramjankhan F, de Weger RA, Lahpor JR, Vink A (2013) Analysis of aortic valve commissural fusion after support with continuous-flow left ventricular assist device. Interact Cardiovasc Thorac Surg 17:616–624
Bhagra S, Bhagra C, Özalp F, Butt T, Ramesh BC, Parry G, Roysam C, Woods A, Robinson-Smith N, Wrightson N, MacGowan GA, Schueler S (2016) Development of de novo aortic valve incompetence in patients with the continuous-flow HeartWare ventricular assist device. J Heart Lung Transplant 35:312–319
Sidhu K, Lam PH, Mehra MR (2020) Evolving trends in mechanical circulatory support: clinical development of a fully magnetically levitated durable ventricular assist device. Trends Cardiovasc Med 30:223–229
Cowger J, Pagani FD, Haft JW, Romano MA, Aaronson KD, Kolias TJ (2010) The development of aortic insufficiency in left ventricular assist device-supported patients. Circ Heart Fail 3:668–674
Cikes M, Jakus N, Claggett B, Brugts JJ, Timmermans P, Pouleur AC, Rubis P, Van Craenenbroeck EM, Gaizauskas E, Grundmann S, Paolillo S, Barge-Caballero E, D’Amario D, Gkouziouta A, Planinc I, Veenis JF, Jacquet LM, Houard L, Holcman K, Gigase A, Rega F, Rucinskas K, Adamopoulos S, Agostoni P, Biocina B, Gasparovic H, Lund LH, Flammer AJ, Metra M, Milicic D, Ruschitzka F, PCHF-VAD registry, (2019) Cardiac implantable electronic devices with a defibrillator component and all-cause mortality in left ventricular assist device carriers: results from the PCHF-VAD registry. Eur J Heart Fail 21:1129–1141
Zoghbi WA, Enriquez-Sarano M, Foster E, Grayburn PA, Kraft CD, Levine RA, Nihoyannopoulos P, Otto CM, Quinones MA, Rakowski H, Stewart WJ, Waggoner A, Weissman NJ, American Society of Echocardiography (2003) Recommendations for evaluation of the severity of native valvular regurgitation with two-dimensional and Doppler echocardiography. J Am Soc Echocardiogr 16:777–802
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG (2009) Research electronic data capture (REDCap)–a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 42:377–381
Kasahara S, Sakata Y, Nochioka K, Miura M, Abe R, Sato M, Aoyanagi H, Fujihashi T, Yamanaka S, Shiroto T, Sugimura K, Takahashi J, Miyata S, Shimokawa H (2019) Conversion formula from B-type natriuretic peptide to N-terminal proBNP values in patients with cardiovascular diseases. Int J Cardiol 280:184–189
Noly PE, Pagani FD, Noiseux N, Stulak JM, Khalpey Z, Carrier M, Maltais S (2020) Continuous-flow left ventricular assist devices and valvular heart disease: a comprehensive review. Can J Cardiol 36:244–260
Aliseda A, Chivukula VK, Mcgah P, Prisco AR, Beckman JA, Garcia GJ, Mokadam NA, Mahr C (2017) LVAD outflow graft angle and thrombosis risk. ASAIO J 63:14–23
Saeed D, Westenfeld R, Maxhera B, Keymel S, Sherif A, Sadat N, Petrov G, Albert A, Lichtenberg A (2016) Prevalence of De novo aortic valve insufficiency in patients after HeartWare VAD implantation with an intermittent low-speed algorithm. ASAIO J 62:565–570
Iizuka K, Nishinaka T, Ichihara Y, Miyamoto T, Yamazaki K (2018) Outflow graft anastomosis site design could be correlated to aortic valve regurgitation under left ventricular assist device support. J Artif Organs 21:150–155
Jorde UP, Uriel N, Nahumi N, Bejar D, Gonzalez-Costello J, Thomas SS, Han J, Morrison KA, Jones S, Kodali S, Hahn RT, Shames S, Yuzefpolskaya M, Colombo P, Takayama H, Naka Y (2014) Prevalence, significance, and management of aortic insufficiency in continuous flow left ventricular assist device recipients. Circ Heart Fail 7:310–319
Grinstein J, Kruse E, Sayer G, Fedson S, Kim GH, Jorde UP, Juricek C, Ota T, Jeevanandam V, Lang RM, Uriel N (2016) Accurate quantification methods for aortic insufficiency severity in patients with LVAD: role of diastolic flow acceleration and systolic-to-diastolic peak velocity ratio of outflow cannula. JACC Cardiovasc Imaging 9:641–651
Funding
No funding to disclose.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Gasparovic has nothing to disclose. Dr. Jakus reports non-financial support from Servier, personal fees from Teva Pharmaceutical Industries, personal fees from Krka, non-financial support from Abbott, personal fees from Sanofi Genzyme, outside the submitted work. Dr. Brugts reports grants and personal fees from Abbott, outside the submitted work. Dr. Pouleur reports Advisory Board/Speaker Fee for Astra-Zeneca, MSD, Bayer, Novartis, Actelion, Pfizer. Dr. Timmermans has nothing to disclose. Dr. Rubiś has nothing to disclose. Dr. Gaizauskas has nothing to disclose. Dr. Van Craenenbroeck has nothing to disclose. Dr. Barge-Caballero reports grants from ABBOT, personal fees from ABBOT, other from MEDTRONIC, outside the submitted work. Dr. Grundmann has nothing to disclose. Dr. Paolillo has nothing to disclose. Dr. D'Amario has nothing to disclose. Dr. Braun has nothing to disclose. Dr. Meyns has nothing to disclose. Dr. Droogne has nothing to disclose. Dr. Wierzbicki has nothing to disclose. Dr. Holcman has nothing to disclose. Dr. Planinc reports personal fees from Boehringer Ingelheim, personal fees from Teva Pharmaceutical Industries, personal fees and non-financial support from Novartis, personal fees and non-financial support from Pfizer, personal fees from Servier, personal fees and non-financial support from Krka, personal fees and non-financial support from Bayer, personal fees from Sandoz, personal fees from Corvia, personal fees and non-financial support from Abbott, non-financial support from Sanofi Aventis, outside the submitted work. Dr. Lovric reports personal fees and non-financial support from Astra Zeneca, personal fees and non-financial support from Boehringer Ingelheim, personal fees from Novartis, personal fees from Pliva, personal fees from Servier, personal fees from Sandoz, personal fees from Krka Pharma, personal fees and non-financial support from PharmaS, non-financial support from Pfizer, personal fees from Bayer, personal fees from Pharma Swiss, personal fees from Berlin Chemie, non-financial support from Sanofi Genzyme, personal fees from Novo-Nordisc, personal fees from Mylan, personal fees from CSL Behring, personal fees from Belupo, personal fees from Amgen, personal fees from Alkaloid, outside the submitted work. Dr. Flammer reports personal fees from Alnylam, grants and personal fees from AstraZeneca, personal fees from Bayer, personal fees from Boehringer Ingelheim, personal fees from Fresenius, personal fees from Imedos GmBH, personal fees from Medtronic, personal fees from MSD, personal fees from Mundipharma, grants and personal fees from Novartis, personal fees from Pierre Fabre, personal fees from Pfizer, personal fees from Roche, personal fees from Vifor, personal fees from Zoll, grants from Berlin Heart, outside the submitted work. Dr. Petricevic has nothing to disclose. Dr. Biocina has nothing to disclose. Dr. Lund reports personal fees from Merck, grants and personal fees from Vifor-Fresenius, grants and personal fees from AstraZeneca, grants and personal fees from Relypsa, personal fees from Bayer, grants from Boston Scientific, personal fees from Pharmacosmos, personal fees from Abbott, personal fees from Medscape, personal fees from Myokardia, grants and personal fees from Boehringer Ingelheim, grants and personal fees from Novartis, personal fees from Sanofi, personal fees from Lexicon, outside the submitted work. Dr. Milicic reports personal fees from Boehringer Ingelheim, personal fees from Bayer, personal fees from Pfizer, personal fees from Novartis, personal fees from AstraZeneca, personal fees from Novo Nordisk, personal fees from Teva, personal fees from Servier, outside the submitted work. Dr. Ruschitzka has not received personal payments by pharmaceutical companies or device manufacturers in the last three years (remuneration for the time spent in activities, such as participation in steering committee member of clinical trials, were made directly to the University of Zurich). The Department of Cardiology (University Hospital of Zurich/University of Zurich) reports research-, educational- and/or travel grants from Abbott, Amgen, Astra Zeneca, Bayer, B. Braun, Biosense Webster, Biosensors Europe AG, Biotronik, BMS, Boehringer Ingelheim, Boston Scientific, Bracco, Cardinal Health Switzerland, Daiichi, Diatools AG, Edwards Lifesciences, Guidant Europe NV (BS), Hamilton Health Sciences, Kaneka Corporation, Labormedizinisches Zentrum, Medtronic, MSD, Mundipharma Medical Company, Novartis, Novo Nordisk, Orion, Pfizer, Quintiles Switzerland Sarl, Sanofi, Sarstedt AG, Servier, SIS Medical, SSS International Clinical Research, Terumo Deutschland, V- Wave, Vascular Medical, Vifor, Wissens Plus, ZOLL. The research and educational grants do not impact on Prof. Ruschitzka`s personal remuneration. Dr. Cikes reports grants and personal fees from Novartis, grants and non-financial support from Abbott, personal fees and non-financial support from GE Healthcare, non-financial support from Corvia, personal fees and non-financial support from Pfizer, personal fees from Bayer, personal fees from Boehringer-Ingelheim, personal fees from AstraZeneca, personal fees from Sanofi, personal fees and non-financial support from Teva Pharmaceutical Industries, personal fees from Orion Pharma, personal fees from Medtronic, outside the submitted work.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Gasparovic, H., Jakus, N., Brugts, J.J. et al. Impact of progressive aortic regurgitation on outcomes after left ventricular assist device implantation. Heart Vessels 37, 1985–1994 (2022). https://doi.org/10.1007/s00380-022-02111-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00380-022-02111-1