Abstract
Significant improvements in percutaneous coronary intervention (PCI) technology have enabled cardiovascular procedures to be performed without onsite cardiac surgery facilities. However, little is known about the association between onsite cardiac surgical support and long-term outcomes of PCI, particularly among emergent and complex cases. We investigated whether the presence or absence of cardiovascular surgery affects the long-term prognosis after PCI, emergent and complex elective cases. The SHINANO 5-year registry, a prospective, observational, and multicenter cohort study registry in Nagano, Japan, consecutively included 1665 patients who underwent PCI between August 2012 and July 2013. The procedures were performed at 11 hospitals with onsite cardiac surgery facilities [onsite surgery (+) group; n = 1257] and 8 hospitals without onsite cardiac surgery facilities [onsite surgery (−) group; n = 408]. The primary endpoint was all-cause mortality and the secondary endpoint was major adverse cardiac and cerebrovascular events [MACCE: all-cause death, Q-wave myocardial infarction, non-fatal stroke, and target lesion revascularization]. The onsite surgery group (+) had a lower rate of emergent PCI and ST-segment elevation myocardial infarction (40.8% vs. 51.7%, p < 0.01 and 24.9% vs. 39.2%, p < 0.01, respectively), and a higher prevalence of hemodialysis and history of peripheral artery disease (7.6% vs. 2.45%, p < 0.01 and 12.1% vs. 6.9%, p < 0.01, respectively). However, the Kaplan–Meier analysis showed no difference in the 5-year mortality rate (16.4% vs. 15.2%, p = 0.421) and MACCE incidence (31.6% vs. 28.9%, p = 0.354) between the groups. Also, there were no differences in the mortality rate and incidence of MACCE among emergent cases of ST-segment elevation myocardial infarction and complex elective cases who underwent PCI. Long-term outcomes of PCI appear to be comparable between institutions with and without onsite cardiac surgical facilities.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Percutaneous coronary intervention (PCI) centers without onsite cardiac surgical support are currently available. With significant improvements in PCI technology and devices, the initial procedural outcome and incidence of complications have improved [1,2,3,4,5,6,7]. In addition, since PCI has become an effective treatment modality for coronary artery disease (CAD), it is possible to provide rapid treatment for patients living in areas away from hospitals that offer cardiovascular surgery. In 2005, it was shown that 16% of all PCI centers in the United States operated without onsite backup cardiac surgery facilities, and this rate may have increased in recent years [8].
Large meta-analyses, prospective registry studies, single-center studies, and retrospective studies have reported no significant differences in mortality rate between the two types of institutions (regarding the availability or unavailability of cardiovascular surgery facilities) [1, 9,10,11]. Also, the latest version of the Japanese guideline recommends (class IIa recommendation) that primary PCI for ST-segment elevation myocardial infarction (STEMI) should be performed at centers without onsite backup cardiac surgery facilities (level of evidence, B) [12, 13]. In complex elective cases, the European Society of Cardiology (ESC) guideline on myocardial revascularization mentioned that non-emergency high-risk PCI procedures should only be performed by adequately experienced operators at centers that have access to circulatory support and intensive care treatment (class IIa recommendation; level of evidence, C) [14]. Currently, PCI is an issue of concern at institutions without onsite surgical support in emergent and complex cases.
In this era, many institutions without onsite cardiac backup surgical facilities have already been established; however, it is believed that there are some differences in the experience of PCI at these institutions.
The SHINANO registry focused on the circumstances surrounding the provision of PCI at local sites in Japan, including institutions without adequately experienced operators. Therefore, it is important to further understand the outcomes of PCI at hospitals without on-site cardiac surgery facilities. The present study aimed to compare the initial and 5-year outcomes of PCI, particularly in emergent and complex elective cases, between hospitals with and without onsite cardiac surgery facilities in a single local prefecture in a mountainous area.
Materials and methods
Study population
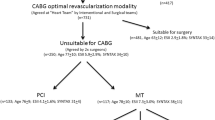
The present retrospective cohort study was based on data from the SHINANO 5-year registry from August 2012 to July 2013 obtained from the Shinshu Prospective Multicenter Analysis for Elderly Patients with Coronary Artery Disease Undergoing Percutaneous Coronary Intervention registry [9]. The SHINANO registry is a prospective, multicenter, observational registry of patients with any CAD diagnosis, including stable angina, STEMI, non-STEMI (NSTEMI), and unstable angina (UA), undergoing PCI at hospitals located in the Nagano prefecture, Japan. This study was based on an all-comer registry, and there were no exclusion criteria. The study protocol was registered with the University Hospital Medical Information Network Clinical Trials Registry, which has been approved by the International Committee of Medical Journal Editors (UMIN-ID 000010070). The study protocol was developed in accordance with the Declaration of Helsinki and was approved by the ethics committee of each participating hospital. All patients provided written informed consent before participating in this study. Among 19 collaborating hospitals in the SHINANO 5-year registry, 11 had onsite cardiac surgery facilities and 8 had no onsite cardiac surgery facilities. Of 1665 patients included in the final analysis, 408 underwent PCI at hospitals without onsite cardiac surgery facilities [onsite surgical backup (−) group] and 1257 underwent PCI at hospitals with onsite cardiac surgery facilities [onsite surgical backup (+) group]. The primary endpoint was all-cause mortality, and the secondary endpoints were major adverse cardiac and cerebrovascular events (MACCE: all-cause death, Q-wave myocardial infarction, non-fatal stroke, and target lesion revascularization) at 5 years. Of 238 patients included in the analysis regarding emergent PCI, 82 underwent PCI at hospitals without onsite cardiac surgery facilities and 156 underwent PCI at hospitals with onsite cardiac surgery facilities. Of 72 patients included in the analysis regarding complex and elective PCI, 14 underwent PCI at hospitals without onsite cardiac surgery facilities and 58 underwent PCI at hospitals with onsite cardiac surgery facilities (Fig. 1).
Definitions
The definitions of variables were based on those of the original paper on the data emanating from the SHINANO registry [15]. Acute coronary syndrome (ACS) was a composite of STEMI, NSTEMI, and UA. “ACS positive” implied that PCI was initially performed for patients with ACS during the enrollment period. STEMI was diagnosed in patients with chest symptoms, ST-segment elevation of 1 mV in two or more limb leads, or 2 contiguous precordial leads, or left bundle branch block, and elevated biochemical markers of myocardial necrosis (troponin T level of 0.01 ng/mL or a creatine phosphokinase level twofold above the upper limit of the normal range). NSTEMI was diagnosed in patients with chest symptoms, ST-segment depression of 0.05 mV, T-wave inversion ≥ 0.3 mV, or transient ST-segment elevation < 0.05 mV, and elevated biochemical markers of myocardial necrosis (and no electrocardiogram abnormalities suggestive of STEMI). UA was diagnosed in patients with persistent resting or nocturnal chest pain with additional features. Diabetes was defined among patients with glycated hemoglobin levels of ≥ 6.5%, fasting plasma glucose levels of ≥ 126 mg/dL, or undergoing treatment with hypoglycemic agents. Hypertension was defined as a systolic blood pressure (BP) ≥ 140 mmHg, diastolic BP ≥ 90 mmHg, or receipt of therapy for hypertension. Dyslipidemia was defined as a serum total cholesterol concentration of ≥ 220 mg/dL, low-density lipoprotein cholesterol concentration ≥ 140 mg/dL, or a current receipt of treatment with lipid-lowering agents. The body mass index was calculated by dividing the weight (in kg) by the square of the patient’s height (in m). Angiographic success was defined as the achievement of a minimum reduction in the stenosis diameter to less than 20% with grade 3 Thrombolysis in Myocardial Infarction flow. The onsite surgical backup (+) group included patients treated at hospitals with full-time physicians who could perform cardiac surgery. Emergent PCI was defined as urgent angioplasty with stenting to open an infarct-related artery during an acute myocardial infarction with ST-segment elevation. Complex elective PCI was defined as a PCI procedure indicated for left main trunk disease, a single remaining patent coronary artery, and chronic total occlusions [14].
Statistical analysis
The normality of distributions was assessed using the Shapiro–Wilk test. Continuous data were reported as the mean ± standard deviation and compared using t tests. Continuous variables without normal distributions were expressed as the median (interquartile range) and compared using the Mann–Whitney U test. Categorical variables were reported as frequencies and percentages. The characteristics of patients in the two groups were compared using chi-squared tests categorical variables or the Kruskal–Wallis test for continuous variables. Survival analyses and MACCE analyses were performed using the Kaplan–Meier method. The statistical analyses were performed using SPSS Statistics version 25.0 (IBM Corporation, Chicago, IL, USA). Analysis items with p < 0.05 were considered statistically significant.
Results
Baseline characteristics
The baseline characteristics and risk factors of the study participants are shown in Table 1. There were no differences in mean age between the two groups (70.61 ± 11.0 vs. 70.86 ± 10.7 years, p = 0.69) and female sex prevalence (22.8% vs. 25.7%, p = 0.23). There were no significant differences in the distributions of coronary risk factors and comorbidities (hypertension, dyslipidemia, and diabetes mellitus) between the groups. In addition, the groups were similar in terms of the distributions of history of heart failure, prior stroke, and previous myocardial infarction. Hemodialysis, peripheral vascular disease, and history of coronary artery bypass grafting (CABG) were more frequently observed in the onsite surgical backup (+) group than in the onsite surgical backup (−) group (7.63% vs. 2.45%, p < 0.01; 12.1% vs. 6.9%, p < 0.01; and 9.5% vs. 3.4%, p < 0.01, respectively). On the other hand, the rates of emergency PCI and STEMI were higher in hospitals without onsite surgical backup (40.8% vs. 51.7%, p < 0.01; 24.9% vs. 39.2%, p < 0.01, respectively).
There were no significant differences in the distribution of patient backgrounds and risk factors between the emergent PCI group and the complex elective PCI group with and without surgery.
Lesion characteristics, procedures, and complications
Table 2 shows the distributions of lesion characteristics, procedures, and PCI complications. In terms of lesion difficulty, number of diseased vessels, bifurcation lesions, chronic total occlusions, and Synergy Between Percutaneous Coronary Intervention with Taxus and Cardiac Surgery scores, no significant differences were found between the two groups. Regarding the technical aspects of PCI, the rates of use of drug-eluting stents and multiple stents were significantly higher in the onsite surgical backup (+) group (46.9% vs. 37.5%, p < 0.01; 22.2% vs. 13.5%, p < 0.01, respectively). However, the rates of use of intra-aortic balloon pumping during PCI were significantly higher in the onsite surgical backup (−) group (4.77% vs. 7.84%, p = 0.024). The rate of complete revascularization was higher in the onsite surgical backup (+) group than in the surgical backup (−) group (67.5% vs. 59.3%, p < 0.01).
Initial and long-term outcomes
The initial success rates were similar between the onsite surgical backup (+) and surgical backup (−) groups (92.8% vs. 90.0%, p = 0.08), despite differences in lesion complexity. There were no differences in in-hospital mortality rate between the two groups (2.07% vs. 3.68%, p = 0.095). In terms of each complication related to PCI, the rates of stent thrombosis and PCI-related stroke were similar between the two groups (0.32% vs. 0.00%, p = 0.578; 0.32% vs. 0.74%, p = 0.372, respectively). In contrast, the rate of in-hospital bleeding events was significantly higher in the onsite surgical backup (−) group (0.00% vs. 2.70%, p < 0.001). There was no difference in the number of cases requiring emergent CABG between the two groups (0.24% vs. 0.25%, p = 1.00) (Table 2).
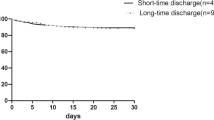
In the 5-year analysis, there were no differences in the rates of all-cause mortality, Q-wave myocardial infarction, and non-fatal stroke (16.4% vs. 15.2%, p = 0.35; 4.22% vs. 15.2%, p = 0.23; and 4.46% vs. 4.90%, p = 0.82, respectively) (Table 3). The Kaplan–Meier analysis showed no differences between the two groups in terms of overall survival (31.6% vs. 28.9%, p = 0.354) and MACCE (22.2% vs. 20.1%, p = 0.269) (Fig. 2).
Long-term outcomes of emergent and complex elective cases
The Kaplan–Meier analysis showed no differences between the two groups in terms of overall survival (25.0% vs. 23.2%, p = 0.670) and MACCE (35.9% vs. 32.9%, p = 0.567) (Fig. 3) among emergent PCI cases. Also, among complex elective cases, there were no differences between the two groups in terms of overall survival (25.9% vs. 14.3%, p = 0.314) and MACCE (39.7% vs. 35.7%, p = 0.718) (Fig. 3).
Discussion
We have shown that there were no differences in initial outcome, long-term mortality, and the incidences of MACCE between patients who underwent PCI at hospitals with onsite surgical backup facilities and those who underwent PCI at hospitals without onsite surgical backup facilities. Also, among patients who underwent emergent PCI on account of STEMI and complex elective PCI there were no significant differences between two groups.
Over a decade ago, in-hospital and 30-day mortality rates were higher in centers without onsite cardiac surgery facilities compared to those with onsite surgical backup facilities [16]. Indeed, the guidelines of those days did not recommend both elective and emergent PCI in institutions without onsite cardiac surgical backup facilities [17]. That recommendation was mainly made to prevent acute occlusions; however, these problems have been resolved in the present decade [2].
Indeed, PCI in hospitals without onsite surgical backup facilities have yielded some favorable results, and the complications of PCI and the need for emergency CABG have become rare events, occurring at rates of only 0.3% [18] to 0.7% [19]. Emergent PCI for STEMI was shown to yield similar outcomes in hospitals with or without cardiac surgery facilities in the presence of an experienced operator [20].
In the last few years, large meta-analyses have reported no significant differences in mortality rates between the two types of institutions (in terms of the presence of cardiovascular surgery for emergent PCI) [1, 9]. In response to these trends, the Japanese guideline recommended that emergent PCI for STEMI should be performed at centers without onsite backup cardiac surgery facilities (class IIa recommendation; level of evidence, B).
A previous study compared the delay of revascularization between emergent PCI performed at an institution without onsite cardiac surgery facilities and emergent PCI performed after transfer to a hospital with onsite cardiac surgery facilities, and revealed a delay of approximately 60 min between the two groups [21]. In general, myocardial infarction is an emergent condition [22] and it is recommended that emergent PCI should be performed as quickly as possible for STEMI within 12 h of onset [23, 24]. In this era, a reduction in the delay of transfer for many institutions that provide PCI might be required.
On the other hand, in complex elective cases, the ESC guideline on myocardial revascularization mentioned that non-emergency high-risk PCI procedures should only be performed by adequately experienced operators at centers that have the facilities to provide circulatory support and intensive care treatment (class IIa recommendation; level of evidence, C) [14]. However, sometimes it is difficult to transfer patients between facilities due to the patient’s condition and the location of facilities. Although the number of complex elective cases were low in this study population, our data supported the safety and efficacy of PCI for emergent cases or complex elective cases.
Considering recent improvements in the quality of PCI, the establishment of a consulting system with experienced operators might enable PCI to be performed for complex cases at institutions without onsite backup surgical facilities. In that respect, establishing a local system and consultation protocol for each situation (e.g., according to emergency and complexity) are important to maintain the safety of patients with CAD.
The main finding of the present study was that the onsite surgical backup (−) group was non-inferior in terms of both acute and long-term outcomes. Furthermore, this non-inferiority was also observed among emergent and/or complex cases. This result might reflect the procedural establishment of PCI, as mentioned above. In addition, it suggests that institutions that provide PCI can function without onsite surgical support in this era. These findings are novel and important for the assessment of the current local medical situation. We also believe that it is useful to assess an appropriate comprehensive system of treatment for patients with CAD. However, further studies should be required to examine the prognosis of the patients who underwent emergent PCI or complex elective PCI, because our research was in one local prefecture and study population was small.
Several limitations of this study should be acknowledged. First, this study was a retrospective analysis. Second, the selection of strategy (between PCI and CABG) entirely depended on each physician’s discretion, which might have led to some bias in our analysis. Third, more than 40% of patients underwent bare-metal stent placement, based on which the strategy may not apply to patients with CAD in clinical practice. Fourth, the cooperation and consultation between each institution were ambiguous. Finally, the experience of PCI operators in each institution was different, which might have caused some discrepancy in the selection of strategy and the outcomes of the procedures.
Emergency PCI is performed more frequently at institutions without onsite backup surgical facilities. There are no differences in the acute and long-term outcomes of PCI between institutions with and without onsite backup surgical facilities. Particularly, regarding PCI for both emergent and complex elective cases, there were no differences in initial and long-term outcomes between the two groups. In this era, even institutions without onsite cardiac surgical backup facilities may be able to provide appropriate care to patients with CAD.
References
Kinlay S (2011) The trials and tribulations of percutaneous coronary intervention in hospitals without on-site CABG surgery. JAMA 306:2507–2509
Shubrooks SJ Jr, Nesto RW, Leeman D, Waxman S, Lewis SM, Fitzpatrick P (2001) Urgent coronary bypass surgery for failed percutaneous coronary intervention in the stent era: Is backup still necessary? Am Heart J 142:190–196
Singh M, Rihal CS, Gersh BJ, Lennon RJ, Prasad A, Sorajja P, Gullerud RE, Holmes DR Jr (2007) Twenty-five-year trends in in-hospital and long-term outcome after percutaneous coronary intervention: a single-institution experience. Circulation 115:2835–2841
Yang EH, Gumina RJ, Lennon RJ, Holmes DR Jr, Rihal CS, Singh M (2005) Emergency coronary artery bypass surgery for percutaneous coronary interventions: changes in the incidence, clinical characteristics, and indications from 1979 to 2003. J Am Coll Cardiol 46:2004–2009
Altmann DB, Racz M, Battleman DS, Bergman G, Spokojny A, Hannan EL, Sanborn TA (1996) Reduction in angioplasty complications after the introduction of coronary stents: results from a consecutive series of 2242 patients. Am Heart J 132:503–507
Haan CK, O’Brien S, Edwards FH, Peterson ED, Ferguson TB (2006) Trends in emergency coronary artery bypass grafting after percutaneous coronary intervention, 1994–2003. Ann Thorac Surg 81:1658–1665
Talley JD, Weintraub WS, Roubin GS, Douglas JS Jr, Anderson HV, Jones EL, Morris DC, Liberman HA, Craver JM, Guyton RA (1990) Failed elective percutaneous transluminal coronary angioplasty requiring coronary artery bypass surgery. In-hospital and late clinical outcome at 5 years. Circulation 82:1203–1213
Dehmer GJ, Kutcher MA, Dey SK, Shaw RE, Weintraub WS, Mitchell K, Brindis RG (2007) Frequency of percutaneous coronary interventions at facilities without on-site cardiac surgical backup—a report from the American College of Cardiology-National Cardiovascular Data Registry (ACC-NCDR). Am J Cardiol 99:329–332
Lee JM, Hwang D, Park J, Kim KJ, Ahn C, Koo BK (2015) Percutaneous coronary intervention at centers with and without on-site surgical backup: an updated meta-analysis of 23 studies. Circulation 132:388–401
Garg S, Anderson SG, Oldroyd K, Berry C, Emdin CA, Peters SAE, West NEJ, Kelly D, Balachandran K, Mcdonald J, Singh R, Devadathan S, Redwood S, Ludman PF, Rahimi K, Woodward M, British Cardiovascular Intervension Society; National Institute for Cardiovascular Outcomes Research (2015) Outcomes of percutaneous coronary intervention performed at offsite versus onsite surgical centers in the United Kingdom. J Am Coll Cardiol 66:363–372
Simard T, Hibbert B, Pourdjabbar A, Ramirez FD, Wilson KR, Hawken S, O’Brien ER (2013) Percutaneous coronary intervention with or without on-site coronary artery bypass surgery: a systematic review and meta-analysis. Int J Cardiol 167:197–204
Kimura K, Kimura T, Ishihara M, Nakagawa Y, Nakao K, Miyaushi K, Sakamoto T, Tsujita K, Hagiwara N, Miyazaki S, Ako J, Arai H, Ishii H, Origuchi H, Shimizu W, Takemura H, Tahara Y, Morino Y, Iino K, Itoh T, Iwanaga Y, Uchida K, Endo H, Kongoji K, Sakamoto K, Shiomi H, Shimohara T, Suzuki A, Takahashi J, Takeushi I, Akihiko T, Tamura T, Nakashima T, Nogushi T, Fukamachi D, Mizuno T, Yamaguchi T, Noguchi T, Fukamachi D, Mizuno T, Yamaguchi J, Yokogawa K, Kosuge M, Kohsaka S, Yoshino H, Yasuda S, Shimokawa H, Hirayama A, Akasaka T, Haze K, Ogawa H, Tsutsui H, Yamazaki T, Japanese Circulation Society Joint Working Group (2018) JCS 2018 guideline on diagnosis and treatment of acute coronary syndrome. Circ J 83:1085–1196
Singh M, Holmes DR Jr, Dehmer GJ, Lennon RJ, Wharton TP, Kutcher MA, Aversano T, Rihal CS (2011) Percutaneous coronary intervention at centers with and without on-site surgery. A meta-analysis. JAMA 306:2487–2494
Neumann FJ, Sousa-Uva M, Ahlsson A, Alfonso F, Banning AP, Benedetto U, Byrne RA, Collet JP, Falk V, Head SJ, Juni P, Kastrati A, Koller A, Kristensen SD, Niebauer J, Richter DJ, Seferovic PM, Sibbing D, Stefanini GG, Windecker S, Yadav R, Zembala MO (2019) 2018 ESC/EACTS guidelines on myocardial revascularization. Eur Heart J 40:87–165
Miura T, Miyashita Y, Motoki H, Shimada K, Kobayashi M, Nakajima H, Kimura H, Akanuma H, Mawatari E, Sato T, Hotta S, Kamiyoshi Y, Maruyama T, Watanabe M, Eisawa T, Aso S, Uchikawa S, Hashizume N, Sekimura N, Morota T, Ebisawa S, Izawa A, Tomita T, Koyama J, Ikeda U (2014) In-hospital clinical outcomes of elderly patients (≥ 80 years) undergoing percutaneous coronary intervention. Circ J 78:1097–1103
Wennberg DE, Lucas FL, Siewers AE, Kellett MA, Malenka DJ (2004) Outcomes of percutaneous coronary interventions performed at centers without and with onsite coronary artery bypass graft surgery. JAMA 292:1961–1968
Smith SC Jr, Feldman TE, Hirshfeld JW Jr, Jacobs AK, Kern MJ, King SB 3rd, Morrison DA, O’Neill WW, Schaff HV, Whitlow PL, Williams DO, Antman EM, Smith SC Jr, Adams CD, Anderson JL, Faxon DP, Fuster V, Halperin JL, Hiratzka LF, Hunt SA, Jacobs AK, Nishimura R, Ornato JP, Page RL, Riegel B, American College of Cardiology/American Heart Association Task Force on Practice Guidelines; ACC/AHA/SCAI Writing Committee to Update the 2001 Guidelines for Percutaneous Coronary Intervention (2001) ACC/AHA/SCAI 2005 guideline update for percutaneous coronary intervention: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (ACC/AHA/SCAI Writing Committee to Update 2001 Guidelines for Percutaneous Coronary Intervention). Circulation 113:e166–e286
Yang EH, Gumina RJ, Lennon RJ, Holmes DR Jr, Rihal CS, Singh M (2005) Emergency coronary bypass surgery for percutaneous coronary intervention. Changes in the incidence, clinical characteristics and indications from 1979 to 2003. J Am Coll Cardiol 46:2004–2009
Dawkins KD, Gershlick T, de Belder M, Chauhan A, Venn G, Schofield P, Smith D, Wakins J, Gray HH, Joint Working Group on Percutaneous Coronary Intervention of the British Cardiovascular Intervention Society and the British Cardiac Society (2005) Percutaneous coronary intervention: recommendations for good practice and training. Heart 91:1–27
Aversano T, Lemmon CC, Liu L, Investigators ACPORT (2012) Outcomes of PCI at hospitals with or without on-site cardiac surgery. N Engl J Med 366:1792–1802
Wharton TP, Grines LL, Turco MA, Johnston JD, Souther J, Lew DC, Shaikh AZ, Bilnoski W, Singhi SK, Atay AE, Sinclair N, Shaddinger DE, Barsamian M, Graham M, Boura J, Grines CL (2004) Primary angioplasty in acute myocardial infarction at hospitals with no surgery on-site (the PAMI-No SOS study) versus transfer to surgical centers for primary angioplasty. J Am Coll Cardiol 43:1943–1950
Lazar HL, Haan CK (1987) Determinants of myocardial infarction following emergency coronary artery bypass for failed percutaneous coronary angioplasty. Ann Thorac Surg 44:646–650
Keeley EC, Boura JA, Grines CL (2003) Primary angioplasty versus intravenous thrombolytic therapy for acute myocardial infarction: a quantitative review of 23 randomised trials. Lancet 361:13–20
Zijlstra F, Hoorntje JC, Boer MJ, Reiffers S, Miedema K, Ottervanger JP, Hof AW, Suryapranata H (1999) Long-term benefit of primary angioplasty as compared with thrombolytic therapy for acute myocardial infarction. N Engl J Med 341:1413–1419
Acknowledgements
We are grateful to the members of the cardiac catheterization laboratories of the participating centers and the clinical research coordinators.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Soichiro Ebisawa is affiliated with the Endowed Department of Medtronic, Abbott Vascular Japan, Boston Scientifics Japan, TERUMO, NIPRO, and Cardinal Health. The other authors declare that they have no conflicts of interest.
Ethical approval
The study protocol was developed in accordance with the Declaration of Helsinki and was approved by the ethics committee of each participating hospital. All patients provided written informed consent before participating in this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Nakamura, C., Ebisawa, S., Miura, T. et al. Effects of cardiac surgical support on long-term outcomes of emergent or complex percutaneous coronary intervention cases: a sub-analysis of the SHINANO 5-year registry. Heart Vessels 37, 1106–1114 (2022). https://doi.org/10.1007/s00380-021-02015-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00380-021-02015-6