Abstract
Purpose
To review available and emerging evidence of radiotherapy for symptom management and disease control in metastatic bladder cancer.
Methods
A literature search and subsequent cross-referencing were carried out for articles in the PubMed and Scopus databases using terms ‘radiotherapy’ OR ‘palliative radiation therapy’ with ‘metastatic bladder cancer’ OR ‘advanced bladder cancer’ between 1990 and 2023, excluding articles with no English translation.
Results
Palliative radiotherapy is an effective and accessible treatment for the alleviation of haematuria and pain due to the primary and metastatic disease. With growing recognition of oligometastatic disease state at diagnosis, response, or progression, radiotherapy can consolidate response by ablating residual or resistant lesions. Experience with other primary cancers supports positive impact of radiotherapy on disease control, quality of life, and survival in oligometastatic stage, without significant adverse effects. Alongside immune checkpoint inhibitors, fibroblast growth receptor inhibitors, and antibody–drug conjugates, the immunomodulatory potential of radiotherapy is being explored in combination with these systemic therapies for metastatic bladder cancer.
Conclusion
Radiotherapy is an effective, safe, and accessible treatment modality for palliation as well as disease control in various clinical settings of metastatic bladder cancer. Its role in oligometastatic stage in combination with systemic therapy is expected to expand with emerging evidence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bladder cancer causes nearly 200,000 deaths each year globally [1]. About 10–15% patients with diagnosed with bladder cancer have metastatic spread at presentation [1, 2]. In the UK, bladder cancer causes about 5000 deaths annually [3]. Lower socioeconomic strata are disproportionately affected, with 5-year overall survival of 46% versus 56% in the highest socioeconomic group [4]. Metastatic bladder cancer (MetBC) includes involvement of lymph nodes beyond the pelvis, or other visceral organs. The prognosis at this stage is dismal, with less than 10% patients surviving at five years from the diagnosis [5]. It also causes considerable morbidity, with urinary symptoms of recurrent or intractable haematuria, pelvic pain, dysuria, and obstructive renal failure. First-line treatment is platinum-based chemotherapy, cisplatin and gemcitabine combination recommended for patients with good renal function (glomerular filtration rate, GFR < 60 mL/min) and performance status of 0–1. Carboplatin is an accepted compromise for those with impaired renal function or worse performance status [3]. Five-year survival of up to 15% can be expected with cisplatin-based chemotherapy [6]. If the disease responds or stabilises with first-line chemotherapy, further maintenance immunotherapy using avelumab has shown to prolong overall survival [7]. First-line immunotherapy as a single agent or within chemotherapy combination has not shown survival benefit [8, 9].
Radiotherapy is a curative treatment for localised and node-positive muscle-invasive bladder cancer, using high-energy ionising radiation to induce cancer cell death [3, 10,11,12,13]. For MetBC, it is an effective treatment for palliation of symptoms such as pelvic pain and haematuria from advanced primary disease, usually requiring 1–5 fractions [14]. Radiotherapy for alleviating painful or symptomatic metastases is a non-invasive, inexpensive, and accessible palliative treatment. Technological advances such as stereotactic ablative radiotherapy (SABR) have made it possible to accurately and safely irradiate tumour lesions to high dose within a few fractions. As the evidence for safety and effectiveness of SABR for metastases has emerged, there is growing interest in pushing the boundaries of curative treatment. Patients with a small number of discrete metastases (oligometastases) are being recognised as a separate group to those presenting with widespread disease [15]. Simultaneously, survival benefit with radiotherapy to the primary tumour has been observed in metastatic stage in malignancies such as prostate cancer [16]. This review considers the role of radiotherapy in symptom management and overall disease control in metastatic bladder cancer. A literature search and subsequent cross-referencing was undertaken for articles in the Pubmed and Scopus databases using terms ‘radiotherapy’ OR ‘palliative radiation therapy’ with ‘metastatic bladder cancer’ OR ‘advanced bladder cancer’ between 1990 and 2023, excluding articles with no English translation.
Radiotherapy for symptom palliation
Effectiveness of radiotherapy for relief of urinary symptoms caused by locally advanced cancer is well established. Table 1 summarises the evidence for palliative radiotherapy for bladder cancer [14, 17,18,19,20,21,22,23]. The earliest of these studies suggests that hypofractionated radiotherapy provides almost universal relief in haematuria, with complete symptom control in over half of the patients [17]. The MRC-BA09 randomised trial established the efficacy of 3-fraction schedule for palliative bladder radiotherapy [14]. For patients without metastatic cancer but considered unsuitable for radical treatment, hypofractionated radiotherapy of 36 Gy in six weekly fractions achieved disease control in 92% of the assessable patients at three months [19]. Cumulative rate of local progression post-radiotherapy was low, being 7% at one year and 17% at 2 years. Grade 3 urinary toxicity and gastrointestinal toxicity were seen in 18% and 4% patients, respectively, during treatment, but at 6 months only 6.5% patients reported any grade 3 toxicity. A more recent study observed clinical outcomes with commonly used schedules of palliative radiotherapy, such as 8 Gy in 1 fraction, 21 Gy in 3 fractions, 20 Gy in 5 fractions, 36 Gy in 6 fractions, or 27.5–30 Gy in 8–10 fractions [20]. Symptomatic improvement such as resolution of haematuria (in 54% patients), dysuria or urinary frequency (57%), and pain control (48%) was observed. Patients treated with 36 Gy dose had better overall survival on univariable analysis (hazard ratio, HR 0.45, p < 0.001), which did not remain significant in multivariable analysis (HR 0.81, p = 0.3) suggesting potential confounding by patient selection for different schedules. More importantly, about a quarter of patients treated with palliative bladder radiotherapy either discontinued treatment or died with a month of starting radiotherapy. This study emphasised the importance of patient selection for palliative radiotherapy based on performance status, disease stage, severity of symptoms, and expected prognosis, to optimise the palliative benefit.
Reliable comparison of efficacy among various palliative schedules is difficult due to small patient cohorts. Biologically effective dose (BED) of ≥ 36 Gy (a/b = 10) was associated with longer and better control of haematuria in two studies [22, 23]. Haematuria in patients treated with BED ≥ 36 Gy responded better than < 36 Gy (77% vs 61%), remained controlled for longer (median control 8.4 months vs 0.7 months, HR 0.39, p = 0.02), and recurred less (HR 5.76 for < 36 Gy vs > 36 Gy, p = 0.01). However, no difference was observed on overall survival [20, 22]. The schedule of 36 Gy in six fractions once-weekly has shown durable symptom palliation in 50–90% patients as well as local disease control up to 90% at one year, with about 38–42% grade 2 and 4–20% grade 3 acute toxicity [17, 19, 21] even if it has never been compared prospectively to other established radiotherapy schedules. For patients with life expectancy of less than six months, one to three fractions appear convenient to provide adequate symptom relief. A higher dose may be preferable for patients with lower disease burden, better performance status and relatively longer life expectancy, although MRC BA06 confirmed similar clinical outcomes of 21 Gy in 3 fractions to 35 Gy in 10 fractions.
Metastases-directed radiotherapy for oligometastatic bladder cancer
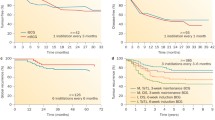
MetBC includes loco-regional and distant metastases of varying disease burden. Oligometastatic stage has been suggested as a transition between limited and extensive spread, which has been further refined into oligoprogression (for metastatic progression), oligopersistence (residual during treatment), or oligorecurrence (during a treatment free interval) [15]. Early clinical trials suggest that targeting oligometastases with SABR for selected patients prolongs disease control with few adverse effects. The prospective trials recruited oligometastases of mixed primary origin, of which bladder cancer comprised a small proportion [24,25,26]. Specifically for bladder or urothelial cancer, a few retrospective studies (Table 2) have reported clinical outcomes with SABR for oligometastases [27,28,29,30,31,32]. Lymph nodes were the most commonly treated lesions in these case series [27,28,29, 31]. A retrospective case series of 91 patients with up to 5 metastases reported improved overall survival (HR 0.48, p = 0.026) and progression free survival at 6 months (HR 0.57, p = 0.083) for those who received consolidative radiotherapy to the bladder and residual metastases compared with those in an observation group, with local nodes treated most commonly (64%) [29]. Another multicentre retrospective analysis of 61 patients with ≤ 5 metastases at diagnosis reported on outcomes after SABR to total 82 lesions, commonest being lung (40%) [30]. After a median follow-up of 17 months, local control of 92% at 1 year and 89% at 2 years was observed. Patients benefitted from systemic therapy before SABR (local control HR 2.62, p = 0.034) and higher total dose (OS HR 0.93, p = 0.003), and number of metastases was predictive for progression-free survival (HR 2.65, p = 0.008). Importantly, consolidative radiotherapy was overall well tolerated in these studies, with 0–3% grade 3 toxicity and no grade 4 toxicity. To note, two cohorts had local treatment to the bladder primary in addition to metastases-directed radiotherapy [29, 32]. First study had 15 patients treated with primary cystectomy followed by metastatic recurrence and first-line chemotherapy, with radiotherapy to oligoresidual lesions [32], and the second study had 91 patients treated with radiotherapy to bladder and oligometastases [29]. Median progression-free survival in these cohorts was 13–15 months, in contrast to 3–6 months for other cohorts of metastases-directed radiotherapy. With the caveats of heterogeneous inclusion criteria and treatment approaches, treatment of both the oligometastases and the bladder primary may result in more durable disease control.
Recently, oligometastatic bladder cancer (OMBC) was formally recognised by a consensus of the European academic oncologists and urologists [33]. The consensus definition for OMBC was based on feasibility of SABR, as “a maximum of three metastatic sites, all resectable or amenable to stereotactic therapy”. A few important aspects of this definition relevant to clinical practice are as follows:
-
Applicability—The same definition has been agreed upon for all three OMBC subgroups, i.e. synchronous OMBC, metachronous oligorecurrence, and metachronous oligoprogression.
-
Staging imaging—In contrast to traditional imaging-based staging, no consensus was reached on the imaging modality to be used for staging OMBC. Utility of fluorodeoxyglucose (FDG) positron emission tomography/computed tomography (PET/CT) is yet to be established pending prospective evidence [34], and contrast-enhanced CT and/or magnetic resonance imaging (MRI) remain the diagnostic standard.
-
Organ sites—Pelvic lymph nodes were not specifically recognised as a separate organ site for metastasis. This aligns with the American Joint Committee on Cancer (AJCC) staging, where pelvic nodal positivity is staged as non-metastatic. Extra-pelvic lymph nodes are considered metastatic by the AJCC as well as the OMBC consensus definition.
-
Patient selection—Favourable response to systemic treatment is a key criterion to be considered for metastasis-directed therapy, emphasising the importance of tumour biology and systemic control before the feasibility of local treatment.
Hopefully, this definition would provide a common standard for future research in OMBC. It also leaves the door open for future advancements in radiotherapy technology, to push the limits of number of metastatic sites which can be treated safely. As the ablative radiotherapy evolves in OMBC, exploring the utility of metastasectomy vis-à-vis radiotherapy for disease control would likely be of interest for the urologists [35].
Bladder radiotherapy for metastatic bladder cancer
Apart from symptom control, radiotherapy to the bladder primary is being explored for benefits of disease control and survival. This hypothesis is being extrapolated from recent evidence from other cancers. A recent meta-analysis of about 5000 patients with metastatic cancer, who received local treatment (surgery or radiotherapy) for the primary disease site, observed that radiotherapy to the primary was associated with significant improvement in overall survival (HR 0.67, 95% CI 0.52–0.85) in patients with low metastatic burden [36]. This benefit was not observed for high metastatic burden, nor with surgery for oligometastatic disease. The strongest evidence for survival benefit of radiotherapy in oligometastatic cancer is in prostate cancer and nasopharyngeal cancer [16, 37, 38]. Proposed biological rationale are reduced seeding of metastases by irradiating the prostate primary, and improved local control leading to reduced morbidity and mortality for nasopharyngeal cancer [36]. It is yet unclear if any or both hypotheses would be applicable to bladder cancer.
Morbidity of locally advanced disease in MetBC is well known, with neuromuscular and visceral progression within the pelvis causing intractable pain, bleeding, fistulae, and sepsis leading to eventual death. Local disease control by early radiotherapy to the bladder in OMBC may prevent this mortality. Studies addressing this question (Table 3) are mainly retrospective, single or multi-institutional series [39,40,41]. While the largest cohorts are from National Cancer Database (NCDB), their results are hampered by inherent shortcomings of this database such as selection bias and inability to extract treatment details of radiotherapy or chemotherapy. There are also a few case series of cystectomy as a consolidative local treatment instead of radiotherapy for patients with favourable response after systemic therapy [39, 42, 43]. A systematic review observed 5-year OS of 28% with a combined approach of complete surgical removal of primary as well as oligometastases after partial response with chemotherapy [44]. The role of these local treatment modalities for de novo or post-chemotherapy OMBC will need to be prospectively studied to reliably determine a clinical benefit.
Combination of radiotherapy and immune checkpoint inhibitors
Immune checkpoint inhibitors (ICI) have been integrated into first-line management of MetBC [3, 45]. Radiation-induced DNA damage causes tumour cell apoptosis, releasing tumour antigens and facilitating immunogenic cell death [46]. Early studies suggest that high-dose radiotherapy or SABR can induce immunostimulatory as well as immunosuppressive changes, leading to unpredictable results when combined with ICI therapy. Tumour irradiation was observed to increase the expression of programmed death ligand 1 (PD-L1) in bladder cancer cells in vitro [47]. On its own, higher PD-L1 is associated with treatment resistance and tumour progression, but PD-L1 blockade by ICIs can synergistically increase tumour cell death. Conversely, late effects of pelvic radiotherapy can be immunosuppressive by selectively decreasing CD4+ T cells and B cells (radiation-induced lymphopenia) and affect response to ICI therapy [46]. In a phase I trial of SABR with immunotherapy for MetBC, tumour response rate was 0% with sequential SABR versus 44% with concurrent pembrolizumab and SABR, suggesting the importance of timing and sequencing of therapies on the immune response [48]. Ongoing phase II ART trial is comparing atezolizumab with or without concurrent SABR in MetBC. Another phase II trial BLAD-RAD01/GETUG-AFU V07 for oligoresidual MetBC stable after first-line chemotherapy is randomising participants to maintenance avelumab alone or with consolidative SABR to bladder and residual metastases. Early experience in non-muscle invasive bladder cancer indicates that determining an appropriate radiotherapy dose in combination with ICI can also be difficult [49]. Dose-limiting urinary toxicity was observed in a phase I trial of pembrolizumab with 36 Gy in 6 weekly fractions to the bladder [50], a radiotherapy dose determined to be safe on its own in an elderly cohort of advanced bladder cancer [19]. Another phase I trial using a lower dose of 18 Gy in 3 fractions with durvalumab observed less adverse effects and considerably reduced efficacy [51]. Delivering an adequately ablative radiotherapy dose to the tumour sites, minimising dose-limiting adverse effects, and establishing optimal sequencing of therapies are major challenges for ongoing and future clinical trials testing radiotherapy-ICI regimens for MetBC.
Future directions
MetBC is almost universally associated with a dismal prognosis, but its biological heterogeneity is gaining recognition [52, 53]. Within and outside the clinical trials, a proportion of patients show exceptional response to systemic therapies, and eventually survive much longer than expected. These patients should be selected early for intensified treatment to have an opportunity for durable cancer control. Using serum proteomic analysis, antitumour immunity has been suggested as a potential explanation for such exceptional response [54]. Circulating tumour DNA (ctDNA) in the plasma, measurable by a blood test, has shown > 80% mutation concordance with the tumour genome in metastatic urothelial cancer and can be a prognostic biomarker after first-line systemic therapy [52]. Serial assessment of plasma ctDNA can complement tumour biopsy by reflecting mutational changes as the disease progresses, identifying additional targetable mutations [53]. Ongoing trials are collecting biological samples with the aim of discovering reliable biomarkers to identify driver mutations, assess tumour burden, find actionable targets, and monitor treatment response.
Conclusion
Radiotherapy for metastatic bladder cancer provides effective symptomatic palliation with minimal added toxicity. Advanced treatment techniques have encouraged its evolution as a consolidative therapy to prolong disease control. SABR to metastases and bladder primary, especially for oligometastatic state, is being explored as a feasible and non-invasive ablative treatment. Presently, studies reporting on clinical outcomes with SABR to the bladder primary and/or oligometastases from bladder cancer are retrospective in nature, with small numbers of patients. Randomised trials may be ideal, but impractical for a relatively rare clinical setting of oligometastatic bladder cancer. High-quality evidence may be obtained from innovations in trial designs, such as the OligoRARE phase III basket trial [NCT04498767] randomising patients with oligometastatic cancer to SABR versus palliative radiotherapy, excluding common primaries of prostate, breast, lung, and colorectal cancer [55]. Early clinical trials are also underway to enhance the understanding of the immunomodulatory role of radiotherapy in conjunction with targeted systemic therapies. Prospective evidence from ongoing research will determine the role of radiotherapy in improving clinical outcomes for metastatic bladder cancer.
Data availability
This article reports no unpublished data, hence data availability statement is not applicable.
References
Richters A, Aben KKH, Kiemeney LALM (2020) The global burden of urinary bladder cancer: an update. World J Urol 38:1895–1904. https://doi.org/10.1007/s00345-019-02984-4
Öztürk H (2015) Detecting metastatic bladder cancer using 18F-fluorodeoxyglucose positron-emission tomography/computed tomography. Cancer Res Treat 47:834–843. https://doi.org/10.4143/crt.2014.157
Bladder cancer: diagnosis and management of bladder cancer: © NICE (2015) Bladder cancer: diagnosis and management of bladder cancer. BJU Int 120:755–765. https://doi.org/10.1111/bju.14045
Jubber I, Mitchell S, Hussain S et al (2022) Social deprivation and bladder cancer: cause or effect for disparities in survival for affected women. BJU Int 130:301–302. https://doi.org/10.1111/bju.15832
National Cancer Institute Bladder Cancer prognosis and Survival Rates. https://www.cancer.gov/types/bladder/survival. Accessed 24 Apr 2023
Von Der Maase H, Hansen SW, Roberts JT et al (2000) Gemcitabine and cisplatin versus methotrexate, vinblastine, doxorubicin, and cisplatin in advanced or metastatic bladder cancer: results of a large, randomized, multinational, multicenter, phase III study. JCO 18:3068–3077. https://doi.org/10.1200/JCO.2000.18.17.3068
Powles T, Park SH, Voog E et al (2020) Avelumab maintenance therapy for advanced or metastatic urothelial carcinoma. N Engl J Med 383:1218–1230. https://doi.org/10.1056/NEJMoa2002788
Powles T, Csőszi T, Özgüroğlu M et al (2021) Pembrolizumab alone or combined with chemotherapy versus chemotherapy as first-line therapy for advanced urothelial carcinoma (KEYNOTE-361): a randomised, open-label, phase 3 trial. Lancet Oncol 22:931–945. https://doi.org/10.1016/S1470-2045(21)00152-2
Powles T, Van Der Heijden MS, Castellano D et al (2020) Durvalumab alone and durvalumab plus tremelimumab versus chemotherapy in previously untreated patients with unresectable, locally advanced or metastatic urothelial carcinoma (DANUBE): a randomised, open-label, multicentre, phase 3 trial. Lancet Oncol 21:1574–1588. https://doi.org/10.1016/S1470-2045(20)30541-6
National Comprehensive Cancer Network Bladder Cancer Version 3.2023. https://www.nccn.org/professionals/physician_gls/pdf/bladder.pdf
Song YP, Mistry H, Irlam J et al (2021) Long-term outcomes of radical radiation therapy with hypoxia modification with biomarker discovery for stratification: 10-year update of the BCON (bladder carbogen nicotinamide) phase 3 randomized trial (ISRCTN45938399). Int J Radiat Oncol Biol Phys 110:1407–1415. https://doi.org/10.1016/j.ijrobp.2021.03.001
Zlotta AR, Ballas LK, Niemierko A et al (2023) Radical cystectomy versus trimodality therapy for muscle-invasive bladder cancer: a multi-institutional propensity score matched and weighted analysis. Lancet Oncol 24:669–681. https://doi.org/10.1016/S1470-2045(23)00170-5
Swinton M, Mariam NBG, Tan JL et al (2023) Bladder-sparing treatment with radical dose radiotherapy is an effective alternative to radical cystectomy in patients with clinically node-positive nonmetastatic bladder cancer. JCO. https://doi.org/10.1200/JCO.23.00725
Duchesne GM, Bolger JJ, Griffiths GO et al (2000) A randomized trial of hypofractionated schedules of palliative radiotherapy in the management of bladder carcinoma: results of medical research council trial BA09. Int J Radiat Oncol Biol Phys 47:379–388. https://doi.org/10.1016/S0360-3016(00)00430-2
Guckenberger M, Lievens Y, Bouma AB et al (2020) Characterisation and classification of oligometastatic disease: a European Society for Radiotherapy and Oncology and European Organisation for Research and Treatment of Cancer consensus recommendation. Lancet Oncol 21:e18–e28. https://doi.org/10.1016/S1470-2045(19)30718-1
Parker CC, James ND, Brawley CD et al (2018) Radiotherapy to the primary tumour for newly diagnosed, metastatic prostate cancer (STAMPEDE): a randomised controlled phase 3 trial. The Lancet 392:2353–2366. https://doi.org/10.1016/S0140-6736(18)32486-3
McLaren DB, Morrey D, Mason MD (1997) Hypofractionated radiotherapy for muscle invasive bladder cancer in the elderly. Radiother Oncol 43:171–174. https://doi.org/10.1016/S0167-8140(97)01943-9
Jose CC, Price A, Norman A et al (1999) Hypofractionated radiotherapy for patients with carcinoma of the bladder. Clin Oncol 11:330–333. https://doi.org/10.1053/clon.1999.9075
Hafeez S, McDonald F, Lalondrelle S et al (2017) Clinical outcomes of image guided adaptive hypofractionated weekly radiation therapy for bladder cancer in patients unsuitable for radical treatment. Int J Radiat Oncol Biol Phys 98:115–122. https://doi.org/10.1016/j.ijrobp.2017.01.239
Ali A, Song YP, Mehta S et al (2019) Palliative radiation therapy in bladder cancer—importance of patient selection: a retrospective multicenter study. Int J Radiat Oncol Biol Phys 105:389–393. https://doi.org/10.1016/j.ijrobp.2019.06.2541
Dirix P, Vingerhoedt S, Joniau S et al (2016) Hypofractionated palliative radiotherapy for bladder cancer. Support Care Cancer 24:181–186. https://doi.org/10.1007/s00520-015-2765-y
Tey J, Soon YY, Cheo T et al (2019) Efficacy of palliative bladder radiotherapy for hematuria in advanced bladder cancer using contemporary radiotherapy techniques. In Vivo 33:2161–2167. https://doi.org/10.21873/invivo.11718
Ogita M, Kawamori J, Yamashita H, Nakagawa K (2021) Palliative radiotherapy for gross hematuria in patients with advanced cancer. Sci Rep 11:9533. https://doi.org/10.1038/s41598-021-88952-8
Palma DA, Olson R, Harrow S et al (2019) Stereotactic ablative radiotherapy versus standard of care palliative treatment in patients with oligometastatic cancers (SABR-COMET): a randomised, phase 2, open-label trial. Lancet 393:2051–2058. https://doi.org/10.1016/S0140-6736(18)32487-5
Sutera P, Clump DA, Kalash R et al (2019) Initial results of a multicenter phase 2 trial of stereotactic ablative radiation therapy for oligometastatic cancer. Int J Radiat Oncol Biol Phys 103:116–122. https://doi.org/10.1016/j.ijrobp.2018.08.027
Chalkidou A, Macmillan T, Grzeda MT et al (2021) Stereotactic ablative body radiotherapy in patients with oligometastatic cancers: a prospective, registry-based, single-arm, observational, evaluation study. Lancet Oncol 22:98–106. https://doi.org/10.1016/S1470-2045(20)30537-4
Leonetti A, D’Abbiero N, Baldari G et al (2018) Radiotherapy for the treatment of distant nodes metastases from oligometastatic urothelial cancer: a retrospective case series. Int J Urol 25:879–886. https://doi.org/10.1111/iju.13773
Augugliaro M, Marvaso G, Ciardo D et al (2019) Recurrent oligometastatic transitional cell bladder carcinoma: is there room for radiotherapy? Neo 66:160–165. https://doi.org/10.4149/neo_2018_180522N333
Aboudaram A, Chaltiel L, Pouessel D et al (2023) Consolidative radiotherapy for metastatic urothelial bladder cancer patients with no progression and with no more than five residual metastatic lesions following first-line systemic therapy: a retrospective analysis. Cancers 15:1161. https://doi.org/10.3390/cancers15041161
Franzese C, Francolini G, Nicosia L et al (2021) Stereotactic body radiation therapy in the management of oligometastatic and oligoprogressive bladder cancer and other urothelial malignancies. Clin Oncol 33:50–56. https://doi.org/10.1016/j.clon.2020.07.008
Francolini G, Desideri I, Detti B et al (2019) Stereotactic radiotherapy in oligoprogressive and oligorecurrent urothelial cancer patients: a retrospective experience. Cancer Treat Res Commun 19:100124. https://doi.org/10.1016/j.ctarc.2019.100124
Shah S, Zhang CA, Hancock S et al (2017) Consolidative radiotherapy in metastatic urothelial cancer. Clin Genitourin Cancer 15:685–688. https://doi.org/10.1016/j.clgc.2017.04.007
Bamias A, Stenzl A, Brown SL et al (2023) Definition and diagnosis of oligometastatic bladder cancer: a Delphi consensus study endorsed by the European Association of Urology, European Society for Radiotherapy and Oncology, and European Society Of Medical Oncology Genitourinary Faculty. Eur Urol. https://doi.org/10.1016/j.eururo.2023.05.005
Verghote F, Poppe L, Verbeke S et al (2021) Evaluating the impact of 18F-FDG-PET-CT on risk stratification and treatment adaptation for patients with muscle-invasive bladder cancer (EFFORT-MIBC): a phase II prospective trial. BMC Cancer 21:1113. https://doi.org/10.1186/s12885-021-08861-x
Ogihara K, Kikuchi E, Watanabe K et al (2017) Can urologists introduce the concept of “oligometastasis” for metastatic bladder cancer after total cystectomy? Oncotarget 8:111819–111835. https://doi.org/10.18632/oncotarget.22911
Ryckman JM, Thomas TV, Wang M et al (2022) Local treatment of the primary tumor for patients with metastatic cancer (PRIME-TX): a meta-analysis. Int J Radiat Oncol Biol Phys 114:919–935. https://doi.org/10.1016/j.ijrobp.2022.06.095
Boevé LMS, Hulshof MCCM, Vis AN et al (2019) Effect on survival of androgen deprivation therapy alone compared to androgen deprivation therapy combined with concurrent radiation therapy to the prostate in patients with primary bone metastatic prostate cancer in a prospective randomised clinical trial: data from the HORRAD trial. Eur Urol 75:410–418. https://doi.org/10.1016/j.eururo.2018.09.008
You R, Liu Y-P, Huang P-Y et al (2020) Efficacy and safety of locoregional radiotherapy with chemotherapy vs chemotherapy alone in de novo metastatic nasopharyngeal carcinoma: a multicenter phase 3 randomized clinical Trial. JAMA Oncol 6:1345. https://doi.org/10.1001/jamaoncol.2020.1808
Seisen T, Sun M, Leow JJ, et al (2016) Efficacy of High-Intensity Local Treatment for Metastatic Urothelial Carcinoma of the Bladder: A Propensity Score–Weighted Analysis From the National Cancer Data Base. J Clin Oncol 34:3529–3536. https://doi.org/10.1200/JCO.2016.66.7352
Fischer-Valuck BW, Patel SA, Brenneman RJ et al (2022) Association between local radiation therapy to the primary bladder tumor and overall survival for patients with metastatic urothelial cancer receiving systemic chemotherapy. Eur Urol Oncol 5:246–250. https://doi.org/10.1016/j.euo.2022.02.001
Passaperuma K, Ash R, Venkatesan V et al (2006) Pelvic chemoradiotherapy after chemotherapy for metastatic bladder cancer. Can J Urol 13:3009–3015
Sweeney P, Millikan R, Donat M et al (2003) Is there a therapeutic role for post-chemotherapy retroperitoneal lymph node dissection in metastatic transitional cell carcinoma of the bladder? J Urol 169:2113–2117. https://doi.org/10.1097/01.ju.0000067601.29966.4a
Ho PL, Willis DL, Patil J et al (2016) Outcome of patients with clinically node-positive bladder cancer undergoing consolidative surgery after preoperative chemotherapy: the M.D. Anderson Cancer Center Experience. Urol Oncol: Semin Origin Investig 34:59.e1-59.e8. https://doi.org/10.1016/j.urolonc.2015.08.012
Neuzillet Y, Larré S, Comperat E et al (2013) Traitement chirurgical du carcinome urothélial de vessie métastatique : revue du Comité de cancérologie de l’Association française d’urologie. Prog Urol 23:951–957. https://doi.org/10.1016/j.purol.2013.03.004
National Comprehensive Cancer Network NCCN Bladder Cancer Version2.2021
Daro-Faye M, Kassouf W, Souhami L et al (2021) Combined radiotherapy and immunotherapy in urothelial bladder cancer: harnessing the full potential of the anti-tumor immune response. World J Urol 39:1331–1343. https://doi.org/10.1007/s00345-020-03440-4
Wu C-T, Chen W-C, Chang Y-H et al (2016) The role of PD-L1 in the radiation response and clinical outcome for bladder cancer. Sci Rep 6:19740. https://doi.org/10.1038/srep19740
Sundahl N, Vandekerkhove G, Decaestecker K et al (2019) Randomized phase 1 trial of pembrolizumab with sequential versus concomitant stereotactic body radiotherapy in metastatic urothelial carcinoma. Eur Urol 75:707–711. https://doi.org/10.1016/j.eururo.2019.01.009
Maitre P, Sangar V, Choudhury A (2023) ADAPT and improvise: overcoming Bacillus Calmette-Guérin unresponsiveness in non–muscle-invasive bladder cancer. Eur Urol. https://doi.org/10.1016/j.eururo.2023.02.018
Tree AC, Jones K, Hafeez S et al (2018) Dose-limiting urinary toxicity with pembrolizumab combined with weekly hypofractionated radiation therapy in bladder cancer. Int J Radiat Oncol Biol Phys 101:1168–1171. https://doi.org/10.1016/j.ijrobp.2018.04.070
Hahn NM, O’Donnell MA, Efstathiou JA et al (2023) A phase 1 trial of durvalumab in combination with Bacillus Calmette-Guerin (BCG) or external beam radiation therapy in patients with BCG-unresponsive non-muscle-invasive bladder cancer: the hoosier cancer research network GU16-243 ADAPT-BLADDER study. Eur Urol 83:486–494. https://doi.org/10.1016/j.eururo.2023.01.017
Vandekerkhove G, Lavoie J-M, Annala M et al (2021) Plasma ctDNA is a tumor tissue surrogate and enables clinical-genomic stratification of metastatic bladder cancer. Nat Commun 12:184. https://doi.org/10.1038/s41467-020-20493-6
Clinton TN, Chen Z, Wise H et al (2022) Genomic heterogeneity as a barrier to precision oncology in urothelial cancer. Cell Rep 41:111859. https://doi.org/10.1016/j.celrep.2022.111859
Anker J, Pal SK, Kim-Schulze S et al (2023) Antitumor immunity as the basis for durable disease-free treatment-free survival in patients with metastatic urothelial cancer. J Immunother Cancer 11:e007613. https://doi.org/10.1136/jitc-2023-007613
Stereotactic body radiotherapy in addition to standard of care treatment in patients with rare oligometastatic cancers (OligoRARE): a randomized, phase 3, open-label trial. https://clinicaltrials.gov/study/NCT04498767. Accessed 16 Oct 2023
Acknowledgements
A.C. and P.H. are supported by the NIHR Manchester Biomedical Research Centre.
Funding
No funding was received to assist with the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
SA was involved in the project development, data collection, data analysis, and manuscript writing. AC contributed to the project development, data analysis, manuscript writing and editing. PH assisted in the data analysis and manuscript editing. YPS contributed to the data analysis and manuscript editing. PM was responsible for the project development, data collection, data analysis, manuscript writing and editing.
Corresponding author
Ethics declarations
Conflict of interest
A.C is the Editor-in-chief of BMJ Oncology.
Research involving human participants and/or animals
This is an observational review and does not involve human or animal participants.
Informed consent
This review does not involve individual participant data, and therefore, consent is not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ashley, S., Choudhury, A., Hoskin, P. et al. Radiotherapy in metastatic bladder cancer. World J Urol 42, 47 (2024). https://doi.org/10.1007/s00345-023-04744-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00345-023-04744-x