Abstract
Purpose
The prognosis of upper urinary tract urothelial carcinoma (UTUC) is associated with tumour grade (G) and stage. Despite preoperative risk stratification and radical treatment, recurrence and progression are common. Thus, prognostic and monitoring biomarkers are needed. This feasibility study aimed to investigate if targeted analyses on circulating tumour DNA (ctDNA) in plasma could identify tumour-specific gene variants, and thus have potential for further evaluation as a biomarker in UTUC.
Methods
Nine UTUC patients with genetically characterised tumours were included in this prospective pilot study. Two tumour-specific variants were chosen for targeted analyses with multiplex droplet digital PCR on cell-free DNA (cfDNA) from plasma at diagnosis or from recurrence.
Results
Of six patients with diagnostic plasma samples, ctDNA was detected in four with G2 or G3 tumours and tumours > 300m2 in size. Three of these patients progressed in their disease and the fourth had the largest G3 tumour at sampling. In contrast, the two patients with undetectable ctDNA in diagnostic plasma had a G1 tumour and G3 carcinoma in situ (CIS), respectively. The patient with G3 CIS had detectable ctDNA later during follow-up and progressed thereafter with aggressive intravesical recurrence and CT-scan-verified CIS progression in the upper urinary tract. In three patients with small recurrent G1 or G2 tumours, none had detectable ctDNA in plasma and all were progression free.
Conclusion
Our early findings demonstrate that ctDNA in plasma can be detected by targeted analysis in patients with UTUC. However, further studies are needed to determine its role as a potential biomarker.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Although upper urinary tract urothelial carcinoma (UTUC) is rare, the incidence has been increasing during the last decades [1]. The prognosis is associated with tumour grade and stage where the 5-year survival for high-risk UTUC is < 50% and 80–90% for low-risk UTUC [2]. Radical nephroureterectomy is the standard treatment for high-risk patients whilst kidney-sparing surgery, which is coupled with lower complication risk but higher recurrence rate, can be considered for patients with low-risk tumours [2, 3]. In recent years, promising molecular biomarkers for diagnosis and risk stratification have been proposed, but none has yet been introduced in the routine clinical management of UTUC [4]. Hence, further studies on prognostic and monitoring biomarkers are warranted.
When cell death occurs by apoptosis or necrosis, small fragments of cell-free DNA (cfDNA) are released into body fluids such as plasma [5]. In cancer patients, circulating tumour DNA (ctDNA), which carries genetic alterations present in the tumour, constitutes a small proportion of the total cfDNA [5]. Liquid biopsies with analyses on ctDNA have emerged as a new promising method with a broad spectrum of potential clinical applications [5, 6]. Currently, only a handful of studies have evaluated ctDNA as a potential biomarker in UTUC [7,8,9,10,11]. Although the reports have highlighted the potential usefulness of ctDNA in UTUC, further research on its role as a potential biomarker is necessary. In our current pilot study, we investigated if multiplex targeted patient-specific genetic analyses on cfDNA from plasma could be a feasible approach to identify tumour-specific gene variants, and thus be a promising biomarker.
Material and methods
UTUC patient cohort and samples
This prospective study included nine patients diagnosed with UTUC at ureterorenoscopy (URS). Six patients underwent organ-sparing surgery; one patient (PP-6) received radiotherapy as palliative treatment, one patient received BCG-instillation in a solitary kidney with CIS (PP-7) and one patient (PP-8) underwent nephroureterectomy. Patients were diagnosed between 2018 and 2020 and were followed-up routinely (with regular URS, CT scans, urine cytology, cystoscopy and bladder wash cytology) to censor date (February 2023) or death. A next-generation sequencing (NGS) gene panel consisting of 387 genes was performed on barbotage specimens obtained at URS at diagnosis or local recurrence for genetic characterisation of all tumours prior to inclusion [12]. The NGS gene panel was performed as previously published [13]. Blood (plasma) samples were collected in conjunction with URS with verified UTUC at initial diagnosis before treatment for 6/9 patients and at the time of local recurrence for 3/9 patients. Additional plasma samples were collected for three patients at recurrence/stable disease (except for PP-1 who was tumour free when one extra plasma sample was collected). No patient had concurrent bladder cancer at the time of plasma sampling. Clinical and follow-up data were collected as described in Supplementary methods. Disease progression was defined as distant metastasis, progression to higher tumour grade or death from UTUC during follow-up and recurrence was defined as local recurrence in the upper urinary tract. The study was approved by Region Ethical Review Board in Stockholm. All patients gave their informed consent prior to inclusion.
Extraction of cfDNA from plasma and droplet digital PCR
Extraction of cfDNA from plasma and droplet digital PCR (ddPCR) was performed as previously published and described in Supplementary methods [14]. Targets for each patient were selected based on previous tumour results from the NGS gene panel where single nucleotide variants (SNVs) or indels with highest variant allele frequencies (VAF) were primarily chosen. ddPCR mutation assays for each target labelled with fluorophores FAM for mutant allele and HEX for wildtype (wt) allele were purchased from Bio-Rad (Hercules, CA, USA) and are listed in Supplementary Table 1. Amplitude multiplex ddPCR for two targets/patient was performed on cfDNA from plasma and tumour cell DNA. Tumour cell DNA was used as positive control whilst normal cfDNA from healthy blood donors was used as negative control. ddPCR data analyses and calculations of VAF, false positive rate and concentration of mutant and wild type allele and total cfDNA (copies/mL plasma) were then performed.
Results
Patient characteristics
All patients had verified UTUC at the time of first plasma sample collection, 6/9 at initial diagnosis of UTUC and 3/6 at recurrence. The follow-up time after UTUC diagnosis was 4–55 months and no patient was lost to follow-up. Clinical characteristics including age at diagnosis, sex, tumour grade (G) and follow-up data of each patient are summarised in Table 1. Three patients had G1 tumours whilst two had G2 and four patients had G3 tumours. Of the patients with G2 or G3 tumours, 4/6 patients progressed in their disease during follow-up with either distant metastasis, higher tumour grade or death from disease.
Droplet digital PCR
Two SNVs or indels were selected as targets for each patient based on NGS gene panel data on barbotage tumour cells. Multiplex ddPCR assays were performed on same tumour cell DNA and also cfDNA from plasma samples (Supplementary Fig. 1). VAF, false positive rate, concentration of mutant and wild type allele and total cfDNA are listed in Table 2. In tumour cell DNA, we observed that the VAF of each genetic variant determined by ddPCR followed a similar trend as the VAF determined by NGS (Supplementary Fig. 2a). In plasma samples, the median concentration of total cfDNA was observed to be slightly higher in plasma samples where at least one of the two tumour-specific variants were detected (Fig. 1a). In addition, genetic variants detected in ctDNA from plasma were also observed to have higher median VAF in tumour cells than the variants that were not detected in plasma (Supplementary Fig. 2b).
Total concentration of cfDNA and tumour size at URS at sampling in relation to ddPCR result of ctDNA in plasma. a Plasma samples where ctDNA was detected by ddPCR had higher median concentration of total cfDNA than samples with undetectable ctDNA. b Patients with detectable ctDNA in plasma had generally larger tumours at URS at sampling than the patients with undetectable ctDNA
Plasma ctDNA detection
Tumour-specific variants in cfDNA from plasma were analysed by multiplex ddPCR in 6/9 patients at initial UTUC diagnosis and at recurrent disease for the remaining 3/9 patients. In addition, more than one plasma sample was analysed for three patients. The results from ddPCR in relation to clinical status and outcome are presented in Fig. 2 and Table 3. For the diagnostic cfDNA samples, at least one of two variants were detectable in 4/6 patients, three of whom had G3 tumours at diagnosis. Two of these three patients later progressed in their disease. The remaining patient with detectable ctDNA at diagnosis had a G2 tumour but later also progressed with metastasis and died from disease. In contrast, the two patients with undetectable variants in plasma at diagnosis had a G1 tumour and a stable but BCG-resistant G3 carcinoma in situ (CIS) in a solitary kidney. The patient with G1 tumour also had a plasma sample taken during follow-up where the patient was tumour-free and ctDNA in plasma was not detected. Interestingly, the patient with G3 CIS had detectable variants in ctDNA on a third sampling time point with stable CIS and progressed 10 months thereafter with aggressive intravesical recurrence and CT scan verified CIS progression in the upper urinary tract. The remaining three patients with initial sampling at recurrence had G1 (n = 2) or G2 (n = 1) tumours and were progression free at follow-up. None of these three patients had detectable ctDNA in plasma.
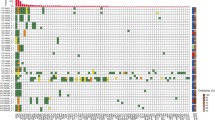
Results from ddPCR of ctDNA in plasma in relation to clinical course and outcome for all included patient with UTUC. Tumour-specific gene variants were detectable with ddPCR in plasma from five patients during their clinical course, of which four of them later progressed in their disease. In contrast, none of the patients with undetectable variants in plasma throughout the follow-up period progressed in their disease. G tumour grade
Tumour size was estimated by URS at the time point of each plasma sampling (Table 3). We observed that patients with detectable ctDNA in plasma had larger median tumour size at URS than patients with undetectable ctDNA (Fig. 1b). For patients with undetectable ctDNA in plasma, the largest tumour size at URS was 100 mm2. This specific plasma sample was taken at diagnosis in a patient with G1 tumour. In contrast, in patients where ctDNA was detected, the smallest tumour size at sampling was 300 mm2. The only exception was the third sampling time point that was positive for ctDNA in the patient with G3 CIS where the tumour was macroscopically undetectable. Amongst the patients with detectable ctDNA at diagnosis, the largest tumour size at sampling was 2491 mm2. This specific patient did not suffer disease progression, but had a large inoperable G3 tumour at the time of sampling and later received palliative treatment with radiotherapy.
Discussion
Although a number of studies have been performed assessing the utility of ctDNA as a prognostic and monitoring biomarker in urothelial carcinoma with promising results [15,16,17], only a few studies have focussed on UTUC [7,8,9,10,11]. These have either used NGS or singleplex ddPCR assays for genetic analysis of ctDNA. In our current feasibility study, UTUC patients with genetically characterised tumours by NGS on tumour cells from barbotage specimens were included to determine whether custom-designed targeted multiplex ddPCR on ctDNA in plasma is a feasible approach to identify previously known tumour-specific gene variants.
In our pilot cohort, where all had detectable tumour-specific gene variants in tumour cells received from focal barbotages, 5/9 patients had detectable ctDNA in plasma during their clinical course. Four of them, including one patient with CIS, later progressed in their disease with either distant metastasis, progression to higher tumour grade or death from UTUC 4–12 months after the sampling time point, which might suggest that ctDNA could have potential as a biomarker for disease progression. These results are consistent with previous findings where ctDNA was found in patients with metastatic UTUC and was shown to predict UTUC patients with poor prognosis [7, 8]. The remaining patient with detectable ctDNA did not progress but had the largest tumour size at URS in the entire cohort. We also observed a trend between tumour size and ctDNA detection, as all with detectable ctDNA (except the patient with CIS) had large macroscopically visible tumours at the time of plasma sampling. It is also known that tumour burden is correlated with ctDNA levels in plasma [18]. However, if this is also applicable for UTUC remains to be further explored.
In this study, targeted multiplex ddPCR was used to detect known patient-specific gene variants in plasma. This method offers a fast, high-sensitivity, minimally invasive and easy-to-interpret approach to detect a few patient-specific variants at once and could, thus, serve as a promising method for surveillance of UTUC if deemed clinically relevant. The only recurrent mutation analysed in the cohort was the TERT promoter mutation C228T, which highlights the need to perform genetic testing on tumour material to select patient-specific genetic variants for monitoring tests. NGS analysis of tumour cells will likely become part of future clinical routine as the cost of sequencing comes down which will simplify the selection of tumour-specific gene targets. Tumour genetic heterogeneity and subclonal genetic evolution during progression affect the genetic landscape and level of ctDNA [17] and are factors that could potentially influence the interpretation of results by this targeted approach. To overcome this issue, we chose to analyse two variants with high VAF in tumour cells determined by NGS for each patient as we speculated that those variants were more likely to be genetic driver events and less likely to be lost during tumour evolution. In 2/5 patients with detectable ctDNA, only one variant was detected in plasma, highlighting the need to screen for several targets. Also, based on our current observations, it is possible that the total cfDNA concentration in plasma could influence the results.
Conclusion
Detection of tumour-specific gene variants in ctDNA from plasma by targeted multiplex ddPCR is a feasible method in patients with UTUC. Our early observations suggest that detection of ctDNA by this minimally invasive approach could have potential as a biomarker in UTUC. However, no clinical conclusions can be drawn and further studies are warranted to determine its role as a biomarker.
Data availability
Not applicable.
References
Soualhi A, Rammant E, George G, Russell B, Enting D, Nair R, Van Hemelrijck M, Bosco C (2021) The incidence and prevalence of upper tract urothelial carcinoma: a systematic review. BMC Urol 21:110
Rouprêt M, Babjuk M, Burger M, Capoun O, Cohen D, Compérat EM, Cowan NC, Dominguez-Escrig JL, Gontero P, Hugh Mostafid A et al (2021) European association of urology guidelines on upper urinary tract urothelial carcinoma: 2020 update. Eur Urol 79:62–79
Cutress ML, Stewart GD, Zakikhani P, Phipps S, Thomas BG, Tolley DA (2012) Ureteroscopic and percutaneous management of upper tract urothelial carcinoma (UTUC): systematic review. BJU Int 110:614–628
Fujii Y, Sato Y, Suzuki H, Kakiuchi N, Yoshizato T, Lenis AT, Maekawa S, Yokoyama A, Takeuchi Y, Inoue Y et al (2021) Molecular classification and diagnostics of upper urinary tract urothelial carcinoma. Cancer Cell 39:793-809.e798
Corcoran RB, Chabner BA (2018) Application of cell-free DNA analysis to cancer treatment. N Engl J Med 379:1754–1765
Barbany G, Arthur C, Liedén A, Nordenskjöld M, Rosenquist R, Tesi B, Wallander K, Tham E (2019) Cell-free tumour DNA testing for early detection of cancer - a potential future tool. J Intern Med 286:118–136
Agarwal N, Pal SK, Hahn AW, Nussenzveig RH, Pond GR, Gupta SV, Wang J, Bilen MA, Naik G, Ghatalia P et al (2018) Characterization of metastatic urothelial carcinoma via comprehensive genomic profiling of circulating tumor DNA. Cancer 124:2115–2124
Nakano K, Koh Y, Yamamichi G, Yumiba S, Tomiyama E, Matsushita M, Hayashi Y, Wang C, Ishizuya Y, Yamamoto Y et al (2022) Perioperative circulating tumor DNA enables the identification of patients with poor prognosis in upper tract urothelial carcinoma. Cancer Sci 113:1830–1842
Hayashi Y, Fujita K, Matsuzaki K, Matsushita M, Kawamura N, Koh Y, Nakano K, Wang C, Ishizuya Y, Yamamoto Y et al (2019) Diagnostic potential of TERT promoter and FGFR3 mutations in urinary cell-free DNA in upper tract urothelial carcinoma. Cancer Sci 110:1771–1779
Blumendeller C, Boehme J, Frick M, Schulze M, Rinckleb A, Kyzirakos C, Kayser S, Kopp M, Kelkenberg S, Pieper N et al (2021) Use of plasma ctDNA as a potential biomarker for longitudinal monitoring of a patient with metastatic high-risk upper tract urothelial carcinoma receiving pembrolizumab and personalized neoepitope-derived multipeptide vaccinations: a case report. J Immunother Cancer 9:e001406
Yang B, Zhao X, Wan C, Ma X, Niu S, Guo A, Wang J, Wang J, Sun D, Jiao S (2021) Genomic profiling of Chinese patients with urothelial carcinoma. BMC Cancer 21:162
Axelsson T, Sydén F, Eisfeldt J, Eriksson Y, Lundberg G, Grahn A, Tham E, Brehmer M (2022) Genetic analysis of focal barbotages a complementary diagnostic tool in upper tract urothelial carcinoma. J Endourol 36:A48–A49
Grahn A, Eisfeldt J, Malm C, Foroughi Asl H, Jaremko G, Tham E, Brehmer M (2022) Genomic profile - a possible diagnostic and prognostic marker in upper tract urothelial carcinoma. BJU Int 130:92–101
Wallander K, Haider Z, Jeggari A, Foroughi-Asl H, Gellerbring A, Lyander A, Chozhan A, Cuba Gyllensten O, Hägglund M, Wirta V et al (2023) Sensitive detection of cell-free tumour DNA using optimised targeted sequencing can predict prognosis in gastro-oesophageal cancer. Cancers (Basel) 15:1160
Powles T, Assaf ZJ, Davarpanah N, Banchereau R, Szabados BE, Yuen KC, Grivas P, Hussain M, Oudard S, Gschwend JE et al (2021) ctDNA guiding adjuvant immunotherapy in urothelial carcinoma. Nature 595:432–437
Christensen E, Birkenkamp-Demtröder K, Sethi H, Shchegrova S, Salari R, Nordentoft I, Wu HT, Knudsen M, Lamy P, Lindskrog SV et al (2019) Early detection of metastatic relapse and monitoring of therapeutic efficacy by ultra-deep sequencing of plasma cell-free DNA in patients with urothelial bladder carcinoma. J Clin Oncol 37:1547–1557
Shohdy KS, Villamar DM, Cao Y, Trieu J, Price KS, Nagy R, Tagawa ST, Molina AM, Sternberg CN, Nanus DM et al (2022) Serial ctDNA analysis predicts clinical progression in patients with advanced urothelial carcinoma. Br J Cancer 126:430–439
Heitzer E, Haque IS, Roberts CES, Speicher MR (2019) Current and future perspectives of liquid biopsies in genomics-driven oncology. Nat Rev Genet 20:71–88
Acknowledgements
We thank all patients for participating. This study was supported by the Foundation in Memory of Johanna Hagstrand and Sigfrid Linnér, Region Stockholm, Barncancerfonden, Cancerfonden and the Japanese-Swedish Research Foundation.
Funding
Open access funding provided by Karolinska Institute. Region Stockholm, FoUI-961732, Emma Tham, FoUI-973659,Emma Tham, Stiftelsen Johanna Hagstrand och Sigfrid Linnérs Minne,Japanese Swedish Research Foundation, 2022-PHJ537, Emma Tham, 2021-XET421, Emma Tham, Barncancerfonden, TJ2021-0125, Emma Tham, Cancerfonden, 22 2451 Fk, Emma Tham.
Author information
Authors and Affiliations
Contributions
NM: protocol development, data management, data analysis, manuscript writing/editing. CJ: protocol development, data collection, data analysis, manuscript editing. TA: data collection, manuscript editing. FS: data collection, manuscript editing. MB: protocol/project development, data management, manuscript writing/editing. ET: protocol/project development, data management, manuscript writing/editing.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mu, N., Jylhä, C., Axelsson, T. et al. Patient-specific targeted analysis of circulating tumour DNA in plasma is feasible and may be a potential biomarker in UTUC. World J Urol 41, 3421–3427 (2023). https://doi.org/10.1007/s00345-023-04583-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-023-04583-w