Abstract
Purpose
The objective of the current study was to assess whether and how preoperative risk group distribution and pathological outcomes have changed in men treated with radical prostatectomy (RP) over the past 25 years.
Methods
11,071 patients from a large contemporary registry-based nationwide cohort with RP as primary treatment between 1995 and 2019 were included. Preoperative risk stratification, postoperative outcomes, and 10 years other-cause mortality (OCM) were analyzed.
Results
After 2005, the proportion of low-risk prostate cancer (PCa) decreased from 39.6% to 25.5% in 2010 and decreased further to 15.5% in 2015, and 9.4% in 2019 (p < 0.001). The proportion of high-risk cases increased from 13.1% in 2005 to 23.1% in 2010 and 36.7% in 2015, and 40.4% in 2019 (p < 0.001). After 2005, the proportion of cases with favorable localized PCa decreased from 37.3% to 24.9% in 2010 and decreased further to 13.9% in 2015, and 1.6% in 2019 (p < 0.001). The overall 10 years OCM was 7.7%.
Conclusion
The current analysis documents a clear shift in utilization of RP toward higher-risk PCa in men with long life expectancy. Patients with low-risk PCa or favorable localized PCa are rarely operated. This suggests a shift in applying surgery only to patients who may really benefit from RP and the long-standing discussion of overtreatment might become outdated.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Radical prostatectomy (RP) remains one of the most commonly used first-line treatments for patients with clinically localized prostate cancer (PCa) [1]. However, the benefit concerning oncological outcome of RP is highly dependent on patient- and tumor-specific characteristics [2]. In patients at low-risk RP has no impact on overall or cancer-specific survival, whereas in men with intermediate or high-risk disease, RP significantly decreases mortality due to PCa [3, 4].
The advent of prostate-specific antigen (PSA) testing and its use for early detection and screening for PCa increased stage migration toward more favorable stages [5]. However, substantial rates of overdiagnosis and subsequent overtreatment have been identified as major downsides of PSA testing. Therefore, active surveillance (AS), with the intent to initiate definitive treatment if there is evidence of disease progression, is currently the preferential initial management strategy in low-risk PCa to reduce overtreatment [6]. Conversely, patients with high-risk diseases appear to benefit the most from definitive therapy [7]. About 40% of high-risk patients have organ-confined disease following RP with excellent long-term outcomes while avoiding long-term androgen deprivation therapy [8].
In the last decade, the risk profile of patients showed an inverse trend towards more high-risk disease in RP-treated patients [9, 10]. This is related to multiple evolving factors such as the introduction of AS for low-risk PCa as well as the increased use of RP in multidisciplinary treatment approaches complemented by radiation, androgen deprivation, or chemotherapy in locally advanced or metastatic PCa patients [11,12,13,14].
The aim of the current study was to assess whether and how preoperative risk group distribution and pathological outcomes have changed in men treated with RP over the past 25 years based on above-mentioned developments in a large contemporary registry-based nationwide cohort.
Patients and methods
Data for the current analysis were obtained from the nationwide multicenter German Familial Prostate Cancer study and its database [15, 16]. Since 1994, PCa patients have been prospectively recruited by collaborating clinics and urologists throughout Germany. The database comprises more than 40,000 PCa patients and collects a range of sociodemographic, diagnostic, clinicopathological, and treatment outcome data on PCa patients in Germany. Patient information are updated annually via questionnaires. Informed consent is obtained from each patient. The study was reviewed and approved by the ethical review committee of the Technical University of Munich. For the current analysis, patients were eligible if they had RP between January 1995 and December 2019. Patients after salvage RP were excluded.
Patient characteristics were stratified by year of RP. Clinicopathological characteristics included age at RP, prostate-specific antigen (PSA) level at diagnosis, neoadjuvant or adjuvant therapy, clinical and pathological TNM classification, Gleason Grade Group (GG) of biopsy and RP specimen, and surgical margin. Pathological staging was classified or reclassified for patients diagnosed before 2002 using the UICC TNM classification 2002. Preoperative risk group distribution was applied according to the current European Association of Urology (EAU) guidelines [17]. Following precedents in the literature [13], the definition of favorable localized PCa (defined as ≤ pT2c disease, Gleason GG 1, pN0/X, cM0/X, no adjuvant or neoadjuvant therapy, and PSA ≤ 20 ng/ml) was used as a surrogate to label the patients that are most likely to not have benefitted of RP and likely to have been overtreated, at least from an oncological point of view [13]. Additionally to suitable cancer selection, adequate patient selection based on age, comorbidities, and life expectancy is the other instrument used to avoid overtreatment and can be estimated by the rate of other-cause mortality (OCM) in the RP series.
Data analyses were conducted using the Statistical Analysis System (SAS), version 9.4 (SAS Institute Inc., Cary, NC, USA). Descriptive statistics were used to present participant characteristics. Comparison of risk group distribution and a fraction of favorable localized PCa between years of surgery were conducted using chi-square tests. Differences in age at surgery over the years were examined with linear regression for each risk group separately. p values < 0.05 were considered statistically significant (2-sided test).
Results
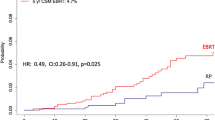
Table 1 presents clinical and pathological patient characteristics as well as risk group distribution of the 11,071 patients included in the study. In general, the cohort is typical of patients undergoing RP in Germany over the last decades. The overall 10 years OCM was 7.7% and men < 65 years at diagnosis had a 10 years OCM of 5.0%.
Figure 1 presents the risk group distribution according to EAU guidelines, per year of surgery. After 2005, the proportion of low-risk PCa decreased from 39.6 to 25.5% in 2010 and decreased further to 15.5% in 2015, and 9.4% in 2019 (p < 0.001). In the same period, the proportion of cases considered high-risk PCa increased from 13.1% in 2005 to 23.1% in 2010 and 36.7% in 2015 and 40.4% in 2019 (p < 0.001).
Preoperative risk group distribution according to the European Association of Urology guidelines [17], per year of surgery
Figure 2 presents the clinicopathological distribution of men with favorable localized PCa (≤ pT2c, Gleason GG 1, pN0/X, cM0/X, no adjuvant or neoadjuvant therapy, and PSA ≤ 20 ng/ml) after RP, per year of surgery. After 2005, the proportion of cases with favorable localized PCa decreased from 37.3 to 24.9% in 2010 and decreased further to 13.9% in 2015, and 1.6% in 2019 (p < 0.001).
Postoperative distribution of favorable localized PCa (≤ pT2c disease, Gleason Grade Group 1, pN0/X, cM0/X, no adjuvant or neoadjuvant therapy, and PSA ≤ 20 ng/ml) [13], per year of surgery
The abovementioned trends were confirmed in further analyses of PSA levels, tumor stage, and Gleason GG, respectively, per year of surgery (Supplementary Figs. 1, 2, 3).
The median age of high, intermediate, and low-risk PCa patients, per year of surgery, is depicted in Fig. 3. While the age of low-risk PCa patients remained stable (p = 0.064), it increased in intermediate and high-risk patients (both p < 0.001). Men who chose RP as the primary treatment of low-risk PCa were younger than RP candidates with higher risk profiles (Fig. 3).
Discussion
The current study reports contemporary RP outcome data of a nationwide registry-based cohort to analyze trends in risk group distribution and oncological outcomes of patients undergoing surgery for PCa in Germany.
Main results showed an important decrease in patients with preoperative low-risk PCa after 2005 (from more than 1 in 3 patients to 1 in 10 patients) of all patients. At the same time, the proportion of high-risk PCa patients increased from around 1 in 10 patients to more than 1 in 3. Further, the number of patients with favorable localized PCa in the final histopathological RP specimen, used as a surrogate to label the patients that are most likely to not have benefitted from RP and therefore oncologically may be considered overtreated, decreased from more than 1 in 3 to even less than 1 in 20 patients. The reason for such changes in risk group distribution and inverse stage and grade migration can only be hypothesized since patient selection is mostly done in the outpatient sector. Especially the advent of magnetic resonance imaging (MRI) and subsequent performed MRI-targeted biopsies in later years might have contributed substantially to stage and grade migration and might be one reason for the decreasing share of low-risk PCa patients. In both PROMIS and PRECISION, the detection rate of clinically insignificant PCa was lower in MRI-targeted biopsies compared to standard biopsies, whereas clinically significant cancers were more often detected [18, 19]. Another reason for the decreasing share of low-risk PCa patients could be the increasing use and acceptance of AS developed among urologists, since active therapy may be considered overtreatment in some low-risk PCa cases and several guidelines including the EAU guidelines strongly recommend the use of AS in low-risk PCa [17]. Indeed, the first reports on AS from the European Randomized Study of Screening for Prostate Cancer and initiation of the Prostate Cancer Research International Active Surveillance (PRIAS) study stem from 2006 to 2007 [20, 21]. The decreasing share among patients having favorable localized PCa who still underwent RP is primarily due to a shift away from GGG 1, whereas pathological tumor stage and PSA levels remained stable within years (see Supplementary Figs. 1, 2, 3). This suggests also an increased use of MRI-targeted biopsies and a better application of AS and risk-driven decisions between patients and urologists. The increase in the use of AS from 57 to 91% for very low-risk PCa and from 40 to 74% for low-risk PCa from 2009 to 2014, respectively, was reported in a population-based study in Sweden [23]. A further Australian study showed an increase in the use of AS from 24 to 39% from 2009 to 2012 [24]. On the other hand, the increasing share of higher-risk cases undergoing surgery may be due to improvements in surgical treatment options and the increasing use of RP in multidisciplinary treatment approaches complemented by radiation, androgen deprivation, or chemotherapy [11, 12, 14, 22].
While the results of the current study assume an evolution in the increasing use of AS in patients with favorable PCa disease characteristics in the last 25 years throughout Germany, the use of other treatments was not considered in the current analysis. However, other treatments such as radiotherapy have also been changing in recent years. For instance, the use of brachytherapy in low-risk PCa decreased over the past decades [25, 26].
A similar analysis in a large German high-volume center cohort was already performed in 2015 (Martini Klinik, Hamburg). In their brief correspondence, the authors encouraged other centers to do similar analyses [27]. Their findings were later confirmed on a European level, however, these results were likewise limited to high-volume center data [13]. The current study additionally presents contemporary data of a representative cross-section of patients in Germany not only limiting to high-volume center patients, since data were derived from high and low volume center, rehabilitation clinics, and primary care urologists throughout Germany.
There are several possibilities to avoid overtreatment such as suitable cancer selection as well as adequate patient selection based on age, performance status, comorbidities, and life expectancy. Adequate patient selection can be estimated by a low rate of OCM in surgical series. The overall 10 years OCM was 7.7% in this population. For instance, the OCM rate in the Prostate Cancer Intervention Versus Observation Trial (PIVOT) at the same point in time was 40% in both the control group and the surgical group [3]. However, these findings cannot be extrapolated to current clinical practice, since the patient selection was obviously inadequate in this cohort and might be, therefore, misleading. Conversely, the aforementioned German single-center study reported a lower rate of OCM compared to PIVOT. After a follow-up of 15 years, the overall OCM rate was low at 14.8%. This supports the findings of the current study and shows that contemporary patient selection is more than appropriate and has the potential to avoid overtreatment. Increasing life expectancy and consideration of comorbidities have the potential to further decrease overtreatment [28].
Strengths of the current analysis include the heterogeneity and the representative cross-section of the patient population as well as the large patient numbers, providing a good overview of the developments over the past 25 years. However, the use of other treatments was not assessed and risk group distribution within the current RP database only provides indirect evidence and no causal conclusions can be drawn from the observed results. For instance, patients might have chosen radiotherapy instead of surgery, which could lead to an overestimation of the reduction of definitive therapy in AS candidates. In addition, changes in diagnostics or treatment possibilities cannot be excluded as further potential causes of changes in risk group distribution.
Conclusions
In the current analysis, a clear shift in the utilization of surgery toward high-risk PCa in men with long life expectancy is shown, whereas patients with low-risk PCa or favorable localized PCa are rarely operated. This confirms a shift in applying RP primarily to patients who may really benefit oncologically, whereas side effects are reduced in patients with the most favorable disease spectrum. Based on these developments, the long-standing discussion of overtreatment with RP might become outdated.
Code availability
Not applicable.
References
Bill-Axelson A, Holmberg L, Garmo H et al (2018) Radical prostatectomy or watchful waiting in prostate cancer—29-year follow-up. N Engl J Med 379:2319–2329
Vickers A, Bennette C, Steineck G et al (2012) Individualized estimation of the benefit of radical prostatectomy from the Scandinavian Prostate Cancer Group randomized trial. Eur Urol 62:204–209
Wilt TJ, Brawer MK, Jones KM et al (2012) Radical prostatectomy versus observation for localized prostate cancer. N Engl J Med 367:203–213
Hamdy FC, Donovan JL, Lane JA et al (2016) 10-year outcomes after monitoring, surgery, or radiotherapy for localized prostate cancer. N Engl J Med 375:1415–1424
Bokhorst LP, Kranse R, Venderbos LD et al (2015) Differences in treatment and outcome after treatment with curative intent in the screening and control arms of the ERSPC rotterdam. Eur Urol 68:179–182
Klotz L, Zhang L, Lam A, Nam R, Mamedov A, Loblaw A (2010) Clinical results of long-term follow-up of a large, active surveillance cohort with localized prostate cancer. J Clin Oncol 28:126–131
Abdollah F, Sun M, Schmitges J et al (2012) Survival benefit of radical prostatectomy in patients with localized prostate cancer: estimations of the number needed to treat according to tumor and patient characteristics. J Urol 188:73–83
Briganti A, Joniau S, Gontero P et al (2012) Identifying the best candidate for radical prostatectomy among patients with high-risk prostate cancer. Eur Urol 61:584–592
Leyh-Bannurah SR, Karakiewicz PI, Pompe RS et al (2019) Inverse stage migration patterns in North American patients undergoing local prostate cancer treatment: a contemporary population-based update in light of the 2012 USPSTF recommendations. World J Urol 37:469–479
Afferi L, Moschini M, Baumeister P et al (2021) Trends in risk-group distribution and Pentafecta outcomes in patients treated with nerve-sparing, robot-assisted radical prostatectomy: a 10-year low-intermediate volume single-center experience. World J Urol 39:389–397
Leyh-Bannurah SR, Gazdovich S, Budäus L et al (2017) Local therapy improves survival in metastatic prostate cancer. Eur Urol 72:118–124
Mathieu R, Korn SM, Bensalah K, Kramer G, Shariat SF (2017) Cytoreductive radical prostatectomy in metastatic prostate cancer: Does it really make sense? World J Urol 35:567–577
van den Bergh R, Gandaglia G, Tilki D et al (2019) Trends in radical prostatectomy risk group distribution in a European multicenter analysis of 28 572 patients: towards tailored treatment. Eur Urol Focus 5:171–178
Albisinni S, Aoun F, Diamand R et al (2019) Cytoreductive prostatectomy: what is the evidence? A systematic review. Minerva Urol Nefrol 71:1–8
Meissner VH, Strüh JGH, Kron M et al (2020) The role of fatal family history and mode of inheritance in prostate cancer for long-term outcomes following radical prostatectomy. World J Urol. https://doi.org/10.1007/s00345-020-03147-6
Paiss T, Herkommer K, Chab A et al (2002) [Familial prostate carcinoma in Germany]. Urologe A 41:38–43
Mottet N, van den Bergh RCN et al (2021) EAU-EANM-ESTRO-ESUR-SIOG guidelines on prostate cancer-2020 update. Part 1: screening, diagnosis, and local treatment with curative intent. Eur Urol 79:243–62
Ahmed HU, El-Shater Bosaily A, Brown LC et al (2017) Diagnostic accuracy of multi-parametric MRI and TRUS biopsy in prostate cancer (PROMIS): a paired validating confirmatory study. Lancet 389(10071):815–822
Kasivisvanathan V, Rannikko AS, Borghi M et al (2018) MRI-targeted or standard biopsy for prostate-cancer diagnosis. N Engl J Med 378(19):1767–1777
van den Bergh RC, Roemeling S, Roobol MJ, Roobol W, Schröder FH, Bangma CH (2007) Prospective validation of active surveillance in prostate cancer: the PRIAS study. Eur Urol 52:1560–1563
Roemeling S, Roobol MJ, Postma R et al (2006) Management and survival of screen-detected prostate cancer patients who might have been suitable for active surveillance. Eur Urol 50:475–482
Yuh B, Artibani W, Heidenreich A et al (2014) The role of robot-assisted radical prostatectomy and pelvic lymph node dissection in the management of high-risk prostate cancer: a systematic review. Eur Urol 65:918–927
Loeb S, Folkvaljon Y, Curnyn C, Robinson D, Bratt O, Stattin P (2017) Uptake of active surveillance for very-low-risk prostate cancer in Sweden. JAMA Oncol 3:1393–1398
Weerakoon M, Papa N, Lawrentschuk N et al (2015) The current use of active surveillance in an Australian cohort of men: a pattern of care analysis from the Victorian Prostate Cancer Registry. BJU Int 115(Suppl 5):50–56
Malouff T, Mathy NW, Marsh S, Walters RW, Silberstein PT (2017) Trends in the use of radiation therapy for stage IIA prostate cancer from 2004 to 2013: a retrospective analysis using the National Cancer Database. Prostate Cancer Prostatic Dis 20:334–338
Evers J, Kerkmeijer LGW, van den Bergh RCN et al (2022) Trends and variation in the use of radiotherapy in non-metastatic prostate cancer: a 12-year nationwide overview from the Netherlands. Radiother Oncol 177:134–142
Huland H, Graefen M (2015) Changing trends in surgical management of prostate cancer: the end of overtreatment? Eur Urol 68:175–178
Froehner M, Koch R, Wirth MP et al (2014) Does increasing life expectancy affect competing mortality after radical prostatectomy? Urol Oncol 32:413–418
Funding
Open Access funding enabled and organized by Projekt DEAL. There was no funding provided for this study.
Author information
Authors and Affiliations
Contributions
VHM: Protocol development, project development, data collection, data management, data analysis, manuscript writing, manuscript editing; VG: Data collection, data management, manuscript editing; MJ: Data analysis, manuscript editing; SS: Data management, data analysis, manuscript editing; JEG: Protocol development, project development, manuscript editing; KH: Protocol development, project development, data collection, data management, manuscript editing.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Research involving human participants and/or animals
Anonymous data of human participants were involved in this study. Animals were not included in this study.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
345_2023_4418_MOESM3_ESM.png
Supplementary file3 (PNG 109 KB) Postoperative distribution of Gleason Grade Group (GGG) of the radical prostatectomy specimen, per year of surgery
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Meissner, V.H., Glöckler, V., Jahnen, M. et al. Changing nationwide trends away from overtreatment among patients undergoing radical prostatectomy over the past 25 years. World J Urol 41, 1497–1502 (2023). https://doi.org/10.1007/s00345-023-04418-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-023-04418-8