Abstract
Introduction and objectives
This systematic review aims to evaluate the incidence and influencing factors of urethral stricture (US) in relation to different BPH endoscopic techniques.
Materials and methods
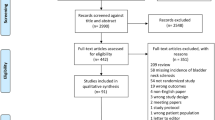
We performed a systematic literature review using MEDLINE, EMBASE, and Cochrane Central Controlled Register of Trials. The incidence of US was estimated through comparative studies between different endoscopic techniques. Patients were assigned into groups according to the type of surgery (enucleation, ablation and resection group). Incidences of US were pooled using the Cochran-Mantel-Haenszel Method with the random effect model and reported as Risk Ratio (RR), 95% Confidence Intervals (CI), and p-values.
Results
A total of 80 studies were included for meta-analysis. The pooled incidence of US was 1.7% after enucleation, 2.1% after ablation, 3.8% after monopolar (M)-TURP and 2.1% after bipolar (B)-TURP. The incidence of US was significantly lower after Enucleation than after TURP (RR 0.58 95% CI 0.39–0.84, p = 0.004). US incidence was lower for Ablation procedures than TURP, but the difference did not reach significance (RR 0.79 95% CI 0.61–1.3, p = 0.08). However, this was significant in the subgroup of M-TURP studies (RR 0.67, 95% CI, 0.49–0.91, p = 0.01). Sub-analysis showed that the risk of US was significantly lower after Enucleation than after TURP within 12 months after surgery (RR 0.51 95% CI 0.33–0.81, p = 0.004).
Conclusion
The study shows an increased incidence of US after TURP compared to enucleation and ablation procedures. The main factors related to increased US incidence are the use of monopolar energy, instrument caliber and duration of postoperative catheterization.
Similar content being viewed by others
Change history
16 June 2022
Last name of the author "Esther Garcia Rojo" was incorrect. Now, it has been corrected to "García Rojo”
References
Lumen N, Hoebeke P, Willemsen P et al (2009) Etiology of urethral stricture disease in the 21st century. J Urol 182:983–987
Chen ML, Correa AF, Santucci RA (2016) Urethral strictures and stenoses caused by prostate therapy. Rev Urol 18(2):90–102
Oelke M, Bachmann A, Descazeaud A et al (2013) EAU guidelines on the treatment and follow-up of non-neurogenic male lower urinary tract symptoms including benign prostatic obstruction. Eur Urol 64(1):118–140
Sun F, Sun X, Shi Q et al (2018) Transurethral procedures in the treatment of benign prostatic hyperplasia: A systematic review and meta-analysis of effectiveness and complications. Medicine (Baltimore) 97(51):e13360
Higgins JPT, Altman DG, Gøtzsche PC, et al (2011) The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 343:d5928.
Ahyai SA, Lehrich K, Kuntz RM (2007) Holmium laser enucleation versus transurethral resection of the prostate: 3-year follow-up results of a randomized clinical trial. Eur Urol 52:1456–1463
Basić D, Stanković J, Potić M et al (2013) Holmium laser enucleation versus transurethral resection of the prostate: a comparison of clinical results. Acta Chir Iugosl 60:15–20
Gupta N, Sivaramakrishna KR et al (2006) Comparison of standard transurethral resection, transurethral vapour resection and holmium laser enucleation of the prostate for managing benign prostatic hyperplasia of > 40 g. BJU Int 97:85–89
Habib EI, ElSheemy MS, Hossam A et al (2021) Holmium laser enucleation versus bipolar plasmakinetic resection for management of lower urinary tract symptoms in patients with large-volume benign prostatic hyperplasia: randomized-controlled trial. J Endourol 35:171–179
Hamouda A, Morsi G, Habib E et al (2014) A comparative study between holmium laser enucleation of the prostate and transurethral resection of the prostate: 12-month follow-up. J Clin Urol 7:99–104
Jhanwar A, Sinha RJ, Bansal A et al (2017) Outcomes of transurethral resection and holmium laser enucleation in more than 60 g of prostate: a prospective randomized study. Urol Ann 9:45–50
Keoghane SR, Lawrence KC, Gray AM et al (2000) A double-blind randomized controlled trial and economic evaluation of transurethral resection vs contact laser vaporization for benign prostatic enlargement: a 3-year follow-up. BJU Int 85:74–78
Luo Y-H, Shen J-H, Guan R-Y et al (2014) Plasmakinetic enucleation of the prostate vs plasmakinetic resection of the prostate for benign prostatic hyperplasia: comparison of outcomes according to prostate size in 310 patients. Urology 84:904–910
Lusuardi L, Myatt A, Sieberer M et al (2011) Safety and efficacy of Eraser laser enucleation of the prostate: preliminary report. J Urol 186:1967–1971
Mavuduru RM, Mandal AK, Singh SK et al (2009) Comparison of HoLEP and TURP in terms of efficacy in the early postoperative period and perioperative morbidity. Urol Int 82:130–135
Montorsi F, Naspro R, Salonia A et al (2004) Holmium laser enucleation versus transurethral resection of the prostate: results from a 2-center, prospective, randomized trial in patients with obstructive benign prostatic hyperplasia. J Urol 172:1926–1929
Carter, Sells, Speakman, et al (1999) A prospective randomized controlled trial of hybrid laser treatment or transurethral resection of the prostate, with a 1-year follow-up. BJU Int 83:254–259.
El-Hawy MM, Eldakhakhny A, AbdEllatif A et al (2021) Two-year follow-up after holmium laser enucleation of the prostate and bipolar transurethral resection of the prostate: a prospective randomized study. African J Urol 27:24
Shingleton WB, Farabaugh P, May W (2002) Three-year follow-up of laser prostatectomy versus transurethral resection of the prostate in men with benign prostatic hyperplasia. Urology 60:305–308
Shoji S, Hanada I, Otaki T et al (2020) Functional outcomes of transurethral thulium laser enucleation versus bipolar transurethral resection for benign prostatic hyperplasia over a period of 12 months: a prospective randomized study. Int J Urol Off J Japanese Urol Assoc 27:974–980
Sukapiriya C, Leenanupunth C (2020) Comparison of the efficacy of transurethral enucleation and resection of the prostate with transurethral resection of the prostate for medium prostate sizes. J Med Assoc Thail 103:1208–1213
Sun N, Fu Y, Tian T et al (2014) Holmium laser enucleation of the prostate versus transurethral resection of the prostate: a randomized clinical trial. Int Urol Nephrol 46:1277–1282
Świniarski PP, Stępień S, Dudzic W et al (2012) Thulium laser enucleation of the prostate (TmLEP) vs. transurethral resection of the prostate (TURP): evaluation of early results. Cent Eur J Urol 65:130–134
Jiang Y, Bai X, Zhang X, et al (2020) Comparative Study of the Effectiveness and Safety of Transurethral Bipolar Plasmakinetic Enucleation of the Prostate and Transurethral Bipolar Plasmakinetic Resection of the Prostate for Massive Benign Prostate Hyperplasia (>80 ml). Med Sci Monit Int Med J Exp Clin Res 26:e921272.
Wilson LC, Gilling PJ, Williams A et al (2006) A randomised trial comparing holmium laser enucleation versus transurethral resection in the treatment of prostates larger than 40 grams: results at 2 years. Eur Urol 50:569–573
Yang Z, Liu T, Wang X (2016) Comparison of thulium laser enucleation and plasmakinetic resection of the prostate in a randomized prospective trial with 5-year follow-up. Lasers Med Sci 31:1797–1802
Zhang K, Sun D, Zhang H et al (2015) Plasmakinetic vapor enucleation of the prostate with button electrode versus plasmakinetic resection of the prostate for benign prostatic enlargement >90 ml: perioperative and 3-month follow-up results of a prospective, randomized clinical trial. Urol Int 95:260–264
Zhang J, Wang X, Zhang Y et al (2019) 1470 nm diode laser enucleation vs plasmakinetic resection of the prostate for benign prostatic hyperplasia: a randomized study. J Endourol 33:211–217
Elshal AM, Soltan M, El-Tabey NA et al (2020) Randomised trial of bipolar resection vs holmium laser enucleation vs Greenlight laser vapo-enucleation of the prostate for treatment of large benign prostate obstruction: 3-years outcomes. BJU Int 126:731–738
Zhao Z, Zeng G, Zhong W et al (2010) A prospective, randomised trial comparing plasmakinetic enucleation to standard transurethral resection of the prostate for symptomatic benign prostatic hyperplasia: three-year follow-up results. Eur Urol 58:752–758
Zhu L, Chen S, Yang S et al (2013) Electrosurgical enucleation versus bipolar transurethral resection for prostates larger than 70 ml: a prospective, randomized trial with 5-year followup. J Urol 189:1427–1431
Eltabey MA, Sherif H, Hussein AA (2010) Holmium laser enucleation versus transurethral resection of the prostate. Can J Urol 17:5447–5452
Enikeev D, Rapoport L, Gazimiev M et al (2020) Monopolar enucleation versus transurethral resection of the prostate for small- and medium-sized (< 80 cc) benign prostate hyperplasia: a prospective analysis. World J Urol 38:167–173
Fayad AS, El SMG, Zakaria T et al (2011) Holmium laser enucleation versus bipolar resection of the prostate: a prospective randomized study. Which to choose? J Endourol 25:1347–1352
Fayad AS, Elsheikh MG, Zakaria T et al (2015) Holmium laser enucleation of the prostate versus bipolar resection of the prostate: a prospective randomized study. “pros and cons.” Urology 86:1037–1041
Geavlete B, Bulai C, Ene C et al (2015) Bipolar vaporization, resection, and enucleation versus open prostatectomy: optimal treatment alternatives in large prostate cases? J Endourol 29:323–331
Gilling PJ, Mackey M, Cresswell M et al (1999) Holmium laser versus transurethral resection of the prostate: a randomized prospective trial with 1-year followup. J Urol 162:1640–1644
Küpeli B, Yalçinkaya F, Topaloğlu H et al (1998) Efficacy of transurethral electrovaporization of the prostate with respect to standard transurethral resection. J Endourol 12:591–594
Liedberg F, Adell L, Hagberg G, Palmqvist I-B (2003) Interstitial laser coagulation versus transurethral resection of the prostate for benign prostatic enlargement–a prospective randomized study. Scand J Urol Nephrol 37:494–497
Kaplan SA, Laor E, Fatal M, Te AE (1998) Transurethral resection of the prostate versus transurethral electrovaporization of the prostate: a blinded, prospective comparative study with 1-year followup. J Urol 159:454–458
Kaya C, Ilktac A, Gokmen E et al (2007) The long-term results of transurethral vaporization of the prostate using plasmakinetic energy. BJU Int 99:845–848
Horasanli K, Silay MS, Altay B et al (2008) Photoselective potassium titanyl phosphate (KTP) laser vaporization versus transurethral resection of the prostate for prostates larger than 70 mL: a short-term prospective randomized trial. Urology 71:247–251
Hon NHY, Brathwaite D, Hussain Z et al (2006) A prospective, randomized trial comparing conventional transurethral prostate resection with PlasmaKinetic vaporization of the prostate: physiological changes, early complications and long-term followup. J Urol 176:205–209
Hoekstra RJ, Van Melick HHE, Kok ET, Ruud Bosch JLH (2010) A 10-year follow-up after transurethral resection of the prostate, contact laser prostatectomy and electrovaporization in men with benign prostatic hyperplasia; long-term results of a randomized controlled trial. BJU Int 106:822–826
Hammadeh MY, Madaan S, Hines J, Philp T (2003) 5-year outcome of a prospective randomized trial to compare transurethral electrovaporization of the prostate and standard transurethral resection. Urology 61:1166–1171
Zhang B, Wu G, Chen C et al (2011) Combination of channel-TURP and ILC versus standard TURP or ILC for elderly with benign prostatic hyperplasia: a randomized prospective trial. Urol Int 87:392–399
Geavlete B, Georgescu D, Multescu R et al (2011) Bipolar plasma vaporization vs monopolar and bipolar TURP-a prospective, randomized, long-term comparison. Urology 78:930–935
Falahatkar S, Mokhtari G, Moghaddam KG et al (2014) Bipolar transurethral vaporization: a superior procedure in benign prostatic hyperplasia: a prospective randomized comparison with bipolar TURP. Int Braz J Urol 40:346–355
Tuhkanen K, Heino A, Ala-Opas M (2001) Two-year follow-up results of a prospective randomized trial comparing hybrid laser prostatectomy with TURP in the treatment of big benign prostates. Scand J Urol Nephrol 35:200–204
Gallucci M, Puppo P, Perachino M et al (1998) Transurethral electrovaporization of the prostate vs. transurethral resection. Results of a multicentric, randomized clinical study on 150 patients. Eur Urol 33:359–364
Elsakka AM, Eltatawy HH, Almekaty KH et al (2016) A prospective randomised controlled study comparing bipolar plasma vaporisation of the prostate to monopolar transurethral resection of the prostate. Arab J Urol 14:280–286
Ekengren J, Haendler L, Hahn RG (2000) Clinical outcome 1 year after transurethral vaporization and resection of the prostate. Urology 55:231–235
Cowles RS 3rd, Kabalin JN, Childs S et al (1995) A prospective randomized comparison of transurethral resection to visual laser ablation of the prostate for the treatment of benign prostatic hyperplasia. Urology 46:155–160
Razzaghi MR, Mazloomfard MM, Mokhtarpour H, Moeini A (2014) Diode laser (980 nm) vaporization in comparison with transurethral resection of the prostate for benign prostatic hyperplasia: randomized clinical trial with 2-year follow-up. Urology 84:526–532
Cetinkaya M, Onem K, Rifaioglu MM, Yalcin V (2015) 980-Nm diode laser vaporization versus transurethral resection of the prostate for benign prostatic hyperplasia: randomized controlled study. Urol J 12:2355–2361
Cimentepe E, Unsal A, Saglam R (2003) Randomized clinical trial comparing transurethral needle ablation with transurethral resection of the prostate for the treatment of benign prostatic hyperplasia: results at 18 months. J Endourol 17:103–107
Cetinkaya M, Ulusoy E, Adsan O et al (1996) Comparative early results of transurethral electroresection and transurethral electrovaporization in benign prostatic hyperplasia. Br J Urol 78:901–903
Peng M, Yi L, Wang Y (2016) Photoselective vaporization of the prostate vs plasmakinetic resection of the prostate: a randomized prospective trial with 12-month follow-up in Mainland China. Urology 87:161–165
Koca O, Keleş MO, Kaya C et al (2014) Plasmakinetic vaporization versus transurethral resection of the prostate: Six-year results. Turkish J Urol 40:134–137
Nuhoğlu B, Balci MBC, Aydin M et al (2011) The role of bipolar transurethral vaporization in the management of benign prostatic hyperplasia. Urol Int 87:400–404
Nuhoğlu B, Ayyildiz A, Fidan V et al (2005) Transurethral electrovaporization of the prostate: is it any better than standard transurethral prostatectomy? 5-year follow-up. J Endourol 19:79–82
Capitán C, Blázquez C, Martin MD et al (2011) GreenLight HPS 120-W laser vaporization versus transurethral resection of the prostate for the treatment of lower urinary tract symptoms due to benign prostatic hyperplasia: a randomized clinical trial with 2-year follow-up. Eur Urol 60:734–739
Bouchier-Hayes DM, Van Appledorn S, Bugeja P et al (2010) A randomized trial of photoselective vaporization of the prostate using the 80-W potassium-titanyl-phosphate laser vs transurethral prostatectomy, with a 1-year follow-up. BJU Int 105:964–969
Purkait B, Sinha RJ, Srinivas KSA et al (2017) Outcome analysis of transurethral resection versus potassium titanyl phosphate-photo selective vaporization of the prostate for the treatment of benign prostatic hyperplasia; a randomized controlled trial with 4 years follow up. Turkish J Urol 43:176–182
Mohanty NK, Vasudeva P, Kumar A et al (2012) Photoselective vaporization of prostate vs. transurethral resection of prostate: a prospective, randomized study with one year follow-up. Indian J Urol 28:307–312
Thomas JA, Tubaro A, Barber N et al (2016) A multicenter randomized noninferiority trial comparing greenlight-XPS laser vaporization of the prostate and transurethral resection of the prostate for the treatment of benign prostatic obstruction: two-yr outcomes of the GOLIATH study. Eur Urol 69:94–102
Abdelwahab O, Habous M, Aziz M et al (2019) Bipolar vaporization of the prostate may cause higher complication rates compared to bipolar loop resection: a randomized prospective trial. Int Urol Nephrol 51:2143–2148
Küpeli S, Baltaci S, Soygür T et al (1998) A prospective randomized study of transurethral resection of the prostate and transurethral vaporization of the prostate as a therapeutic alternative in the management of men with BPH. Eur Urol 34:15–18
Xue B, Zang Y, Zhang Y et al (2013) GreenLight HPS 120-W laser vaporization versus transurethral resection of the prostate for treatment of benign prostatic hyperplasia: a prospective randomized trial. J Xray Sci Technol 21:125–132
Telli O, Okutucu TM, Suer E et al (2015) A prospective, randomized comparative study of monopolar transurethral resection of the prostate versus photoselective vaporization of the prostate with GreenLight 120-W laser, in prostates less than 80 cc. Ther Adv Urol 7:3–8
Sengör F, Köse O, Yücebas E et al (1996) A comparative study of laser ablation and transurethral electroresection for benign prostatic hyperplasia: results of a 6-month follow-up. Br J Urol 78:398–400
Mordasini L, Di Bona C, Klein J et al (2018) 80-W greenlight laser vaporization versus transurethral resection of the prostate for treatment of benign prostatic obstruction: 5-year outcomes of a single-center prospective randomized trial. Urology 116:144–149
Mårtenson AC, De La Rosette JJMCH (1999) Interstitial laser coagulation in the treatment of benign prostatic hyperplasia using a diode laser system: results of an evolving technology. Prostate Cancer Prostatic Dis 2:148–154
Kumar N, Vasudeva P, Kumar A, Singh H (2018) Prospective Randomized Comparison of Monopolar TURP, Bipolar TURP and Photoselective Vaporization of the Prostate in Patients with Benign Prostatic Obstruction: 36 Months Outcome. Low Urin Tract Symptoms
Hill B, Belville W, Bruskewitz R et al (2004) Transurethral needle ablation versus transurethral resection of the prostate for the treatment of symptomatic benign prostatic hyperplasia: 5-year results of a prospective, randomized, multicenter clinical trial. J Urol 171:2336–2340
Gilling P, Barber N, Bidair M et al (2020) Three-year outcomes after Aquablation therapy compared to TURP: results from a blinded randomized trial. Can J Urol 27:10072–10079
Francisca EA, d’Ancona FC, Hendriks JC et al (2000) A randomized study comparing high-energy TUMT to TURP: quality-of-life results. Eur Urol 38:569–575
Floratos DL, Kiemeney LA, Rossi C et al (2001) Long-term followup of randomized transurethral microwave thermotherapy versus transurethral prostatic resection study. J Urol 165:1533–1538
Dahlstrand C, Waldén M, Geirsson G, Pettersson S (1995) Transurethral microwave thermotherapy versus transurethral resection for symptomatic benign prostatic obstruction: a prospective randomized study with a 2-year follow-up. Br J Urol 76:614–618
Bouchier-Hayes DM, Anderson P, Van Appledorn S et al (2006) KTP laser versus transurethral resection: early results of a randomized trial. J Endourol 20:580–585
Al-Ansari A, Younes N, Sampige VP et al (2010) GreenLight HPS 120-W laser vaporization versus transurethral resection of the prostate for treatment of benign prostatic hyperplasia: a randomized clinical trial with midterm follow-up. Eur Urol 58:349–355
Akhtar MM, Orakzai N, Qureshi AM (2004) Trans urethral electric vaporisation of prostate as an alternate to trans urethral resection in benign prostatic hyperplasia. J Ayub Med Coll Abbottabad 16:16–20
Ahmed M, Bell T, Lawrence WT et al (1997) Transurethral microwave thermotherapy (Prostatron version 2.5) compared with transurethral resection of the prostate for the treatment of benign prostatic hyperplasia: a randomized, controlled, parallel study. Br J Urol 79:181–185
Michalak J, Tzou D, Funk J (2015) HoLEP: the gold standard for the surgical management of BPH in the 21(st) Century. Am J Clin Exp Urol. 25;3(1):36–42.
Gilling PJ, Cass CB, Cresswell MD, Fraundorfer MR (1996) Holmium laser resection of the prostate: preliminary results of a new method for the treatment of benign prostatic hyperplasia. Urology 47(1):48–51
Medical Advisory Secretariat (2006) Energy delivery systems for treatment of benign prostatic hyperplasia: an evidence-based analysis. Ont Health Technol Assess Ser 6(17):1–121 (Epub 2006 Aug 1)
Rassweiler J, Teber D, Kuntz R, Hofmann R (2006) Complications of transurethral resection of the prostate (TURP): incidence, management, and prevention. Eur Urol 50:969–979
Abedi A, Razzaghi MR, Rahavian A et al (2020) Is holmium laser enucleation of the prostate a good surgical alternative in benign prostatic hyperplasia management? A review article. J Lasers Med Sci 11(2):197–203
Gunes M et al (2015) Does resectoscope size play a role in formation of urethral stricture following transurethral prostate resection? Int Braz J Urol 41:744
Seki N, Mochida O, Kinukawa N et al (2003) Holmium laser enucleation for prostatic adenoma: analysis of learning curve over the course of 70 consecutive cases. J Urol 170(5):1847–1850
Shah HN, Sodha HS, Kharodawala SJ et al (2008) Influence of prostate size on the outcome of holmium laser enucleation of the prostate. BJU Int 101(12):1536–1541
Bruce A, Krishan A, Sadiq S et al (2021) Safety and efficacy of bipolar transurethral resection of the prostate vs monopolar transurethral resection of prostate in the treatment of moderate-large volume prostatic hyperplasia: a systematic review and meta-analysis. J Endourol 35(5):663–673
Author information
Authors and Affiliations
Contributions
GMP: study design, manuscript drafting, data collection. DC: data management, data analysis and interpretation. EJL: data collection, manuscript drafting and graphic illustration. MLW: data collection. DLQN: data collection. MG: data collection, critical revision of the manuscript. ER: data collection, critical revision of the manuscript. VWSC: statistical analysis. MC: data collection. EGR: data collection. TRWH: critical revision of the manuscript for important intellectual content, supervision. JYCT: study concept, data interpretation, supervision. V: study concept and design, overall work supervision, manuscript editing and data interpretation.
Corresponding author
Ethics declarations
Conflict of interest
GM Pirola, D Castellani, EJ Lim, ML Wroclawski, DLQ Nguyen, M Gubbiotti, E Rubilotta, VWS Chan, M Corrales, EG Rojo, JYC Teoh, V Gauhar have no conflicts of interest to declare. TRW Herrmann is company consultant for Karl Storz.
Human and animal rights
Neither human participants nor animals were involved in this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Pirola, G.M., Castellani, D., Lim, E.J. et al. Urethral stricture following endoscopic prostate surgery: a systematic review and meta-analysis of prospective, randomized trials. World J Urol 40, 1391–1411 (2022). https://doi.org/10.1007/s00345-022-03946-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-022-03946-z