Abstract
Purpose
Leydig-cell tumours (LCT) of the testis are poorly understood clinically. The aim of this report is to analyse the clinical characteristics of LCT in a large patient sample and to compare these findings with corresponding data of germ-cell tumours (GCT).
Methods
In a sample of 208 patients treated during 1995–2017 in 33 institutions, the following characteristics were registered: age, presenting symptoms, primary tumour size, testis-sparing surgery (TSS) or orchiectomy, malignancy, laterality, medical history, and outcome. Data analysis included descriptive statistical methods and logistic regression analysis.
Results
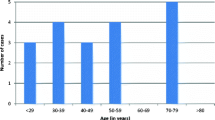
The ratio LCT:GCT is 1:23 (4.4%). The findings are as follows: median age 41 years, undescended testis 8%, bilateral LCTs 3%, malignant LCT 2.5%, contralateral GCT 2.5%, incidental detection 28%, scrotal symptoms 43%, infertility 18%, elevated estradiol levels 29%. TSS was performed in 56% with no local relapse. Of the patients with malignant LCT, one was cured through surgery.
Conclusion
LCT is rare, with a relative frequency (relative to GCT) of 1:23. Malignancy is found in 2.5%. LCT and GCT share a number of clinical features, e.g. bilaterality, history of undescended testis, and presenting age. TSS is safe in benign LCT. Surgery is the treatment of choice in malignant LCT.


Similar content being viewed by others
References
Idrees MT, Ulbright TM, Oliva E, Young RH, Montironi R, Egevad L et al (2017) The World Health Organization 2016 classification of testicular non-germ cell tumours: a review and update from the International Society of Urological Pathology Testis Consultation Panel. Histopathology 70:513–521
Kim I, Young RH, Scully RE (1985) Leydig cell tumors of the testis. A clinicopathological analysis of 40 cases and review of the literature. Am J Surg Pathol 9:177–192
Di Tonno F, Tavolini IM, Belmonte P, Bertoldin R, Cossaro E, Curti P et al (2009) Lessons from 52 patients with Leydig cell tumor of the testis: the GUONE (North-Eastern Uro-Oncological Group, Italy) experience. Urol Int 82:152–157
Masur Y, Steffens J, Ziegler M, Remberger K (1996) Leydigzell-Tumoren des Hodens—klinische und morphologische Aspekte. Urologe A 35:468–471
Calleja RK, Rice A, Bullock KN (1999) Unilateral Leydig cell tumour associated with a contralateral undescended testis. BJU Int 83:152
Dieckmann KP, Loy V (1993) Metachronous germ-cell and Leydig cell tumors of the testis. Do testicular germ cell tumors and Leydig cell tumors share risk factors? Cancer 72:1305–1307
Cheville JC, Sebo TJ, Lager DJ, Bostwick DG, Farrow GM (1998) Leydig cell tumor of the testis: a clinicopathologic, DNA content, and MIB-1 comparison of nonmetastasizing and metastasizing tumors. Am J Surg Pathol 22:1361–1367
Suardi N, Strada E, Colombo R, Freschi M, Salonia A, Lania C et al (2009) Leydig cell tumour of the testis: presentation, therapy, long-term follow-up and the role of organ-sparing surgery in a single-institution experience. BJU Int 103:197–200
Loeser A, Vergho DC, Katzenberger T, Brix D, Kocot A, Spahn M et al (2009) Testis-sparing surgery versus radical orchiectomy in patients with Leydig cell tumors. Urology 74:370–372
Leonhartsberger N, Pichler R, Stoehr B, Horninger W, Steiner H (2014) Organ-sparing surgery is the treatment of choice in benign testicular tumors. World J Urol 32:1087–1091
Nicolai N, Necchi A, Raggi D, Biasoni D, Catanzaro M, Piva L et al (2015) Clinical outcome in testicular sex cord stromal tumors: testis sparing vs radical orchiectomy and management of advanced disease. Urology 85:402–406
Bozzini G, Picozzi S, Gadda F, Colombo R, Decobelli O, Palou J et al (2013) Long-term follow-up using testicle-sparing surgery for Leydig cell tumor. Clin Genitourin Cancer 11:321–324
Rothermundt C, Thurneysen C, Cathomas R, Müller B, Mingrone W, Hirschi-Blickenstorfer A et al (2018) Baseline characteristics and patterns of care in testicular cancer patients: first data from the Swiss Austrian German Testicular Cancer Cohort Study (SAG TCCS). Swiss Med Wkly 148:w14640
Dieckmann KP, Richter-Simonsen H, Kulejewski M, Ikogho R, Zecha H, Anheuser P et al (2018) Testicular germ-cell tumours: a descriptive analysis of clinical characteristics at first presentation. Urol Int 100:409–419
Ruf CG, Isbarn H, Wagner W, Fisch M, Matthies C, Dieckmann KP (2014) Changes in epidemiologic features of testicular germ cell cancer: age at diagnosis and relative frequency of seminoma are constantly and significantly increasing. Urol Oncol 32(33):e1–6
Dieckmann KP, Hartmann JT, Classen J, Lüdde R, Diederichs M, Pichlmeier U (2008) Tallness is associated with risk of testicular cancer: evidence for the nutrition hypothesis. Br J Cancer 99:1517–1521
Heer R, Jackson MJ, El-Sherif A, Thomas DJ (2010) Twenty-nine Leydig cell tumors: histological features, outcomes and implications for management. Int J Urol. 17:886–889
Dieckmann KP, Kulejewski M, Pichlmeier U, Loy V (2007) Diagnosis of contralateral testicular intraepithelial neoplasia (TIN) in patients with testicular germ cell cancer: systematic two-site biopsies are more sensitive than a single random biopsy. Eur Urol 51:175–185
Banks K, Tuazon E, Berhane K, Koh CJ, De Filippo RE, Chang A et al (2012) Cryptorchidism and testicular germ cell tumors: comprehensive meta-analysis reveals that association between these conditions diminished over time and is modified by clinical characteristics. Front Endocrinol (Lausanne). 3:182. https://doi.org/10.3389/fendo.2012.00182
Heidenreich A, Moul JW, Srivastava S, Engelmann UH (1997) Synchronous bilateral testicular tumour: nonseminomatous germ cell tumours and contralateral benign tumours. Scand J Urol Nephrol 31:389–392
Dieckmann KP, Becker T, Bauer HW (1987) Testicular tumors: presentation and role of diagnostic delay. Urol Int 42:241–247
Moul JW (2007) Timely diagnosis of testicular cancer. Urol Clin North Am. 34:109–117
Carmignani L, Salvioni R, Gadda F, Colecchia M, Gazzano G, Torelli T et al (2006) Long-term follow up and clinical characteristics of testicular Leydig cell tumor: experience with 24 cases. J Urol 176:2040–2403
Germa-Lluch JR, Garcia del Muro X, Maroto P, Paz-Ares L, Arranz JA, Guma J et al (2002) Clinical pattern and therapeutic results achieved in 1490 patients with germ-cell tumours of the testis: the experience of the Spanish germ-cell cancer group (GG). Eur Urol 42:553–563
Andreassen KE, Grotmol T, Cvancarova MS, Johannesen TB, Fossa SD (2011) Risk of metachronous contralateral testicular germ cell tumors: a population-based study of 7102 Norwegian patients (1953–2007). Int J Cancer 129:2867–2874
Bandak M, Jørgensen N, Juul A, Lauritsen J, Gundgaard-Kier MG, Mortensen MS et al (2017) Preorchiectomy Leydig cell dysfunction in patients with testicular cancer. Clin Genitourin Cancer 15:e37–e43
Wegner HE, Dieckmann KP, Herbst H, Andresen R, Miller K (1997) Leydig cell tumor—comparison of results of radical and testis-sparing surgery in a single center. Urol Int 59:170–173
Nason GJ, Redmond EJ, Considine SW, Omer SI, Power D, Sweeney P (2017) The natural history of Leydig cell testicular tumours: an analysis of the National Cancer Registry. Ir J Med Sci 187:323–326
Al-Agha OM, Axiotis CA (2007) An in-depth look at Leydig cell tumor of the testis. Arch Pathol Lab Med 131:311–317
Farkas LM, Székely JG, Pusztai C, Baki M (2000) High frequency of metastatic Leydig cell testicular tumours. Oncology 59:118–121
Bokemeyer C, Harstrick A, Gonnermann O, Schöber C, Kuczyk M, Poliwoda H et al (1993) Metastatic Leydig cell tumours of the testis: report of four cases and review of the literature. Int J Oncol 2:241–244
Author information
Authors and Affiliations
Contributions
CGR: project development, data collection, data analysis, manuscript editing. NS: data collection, data analysis, project development. HI: data management, data analysis, manuscript writing. BR: data collection, data analysis, JS: manuscript writing and editing, data management. CDF: project development, data collection. KPD: project development, data collection, data analysis, manuscript writing and editing.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Ruf, C.G., Sanatgar, N., Isbarn, H. et al. Leydig-cell tumour of the testis: retrospective analysis of clinical and therapeutic features in 204 cases. World J Urol 38, 2857–2862 (2020). https://doi.org/10.1007/s00345-020-03079-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-020-03079-1