Abstract
Purpose
To evaluate the long-term effect of using small intestinal submucosa (SIS) for bladder augmentation in patients with neurogenic bladder.
Materials and methods
A total of 15 patients (age range 14–65 years; mean age 29.6 years) were enrolled in our study. The patients had poor bladder capacity and compliance caused by a neurogenic disorder requiring bladder augmentation. A small intestinal submucosa (SIS) cystoplasty was performed alone or in combination with ureter reimplantation. We prospectively followed the cohort to assess the urodynamics parameters, morphologic changes and patient satisfaction and evaluate the clinical benefit of the SIS procedure in long term. The surgical indications and complications were analyzed.
Results
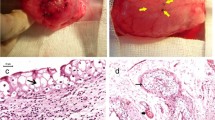
The duration of follow-up ranged from 4.5 to 8.3 years (mean 6.3 years). Nine patients had expected long-term benefit, leading to an overall success rate of 60%. Two patients experienced immediate failure, and four patients slowed decrease in bladder capacity over time. Compared with the baseline data, there were significant increases in bladder capacity (163.5 ± 80.90–275.6 ± 159.5 ml, p < 0.05) and a significant decrease in maximum detrusor pressure (45.07 ± 29.03–17.60 ± 10.34 cmH2O, p < 0.05). Histologic examinations showed a complete conversion of SIS, leaving the urothelial lining and bladder wall containing muscular, vascular, and relatively thick connective tissue. Major complications included vesicoureteral reflux in five patients, bladder stone formation in one patient, and bladder perforation in one patient.
Conclusion
Bladder augmentation with an SIS graft offers a partial long-term success rate in neurogenic bladder patients. This procedure cannot be recommended as a substitute for enterocystoplasty, especially in patients with severe upper urinary tract deterioration and/or bladder fibrosis.




Similar content being viewed by others
Abbreviations
- SIS:
-
Small intestinal submucosa
- TE:
-
Tissue engineering
- BA:
-
Bladder augmentation
- VUDS:
-
Video-urodynamics
- MBC:
-
Maximum bladder capacity
- MDP:
-
Maximum detrusor pressure
- BC:
-
Bladder compliance
- VUR:
-
Vesicoureteric reflux
- IC:
-
Intermittent catheterization
- DO:
-
Detrusor overactivity
- URI:
-
Ureter reimplantation
- UTIs:
-
Urinary tract infections
- UUT:
-
Upper urinary tract
References
Atala A, Bauer SB, Soker S (2006) Tissue engineered autologous bladders for patients needing cystoplasty. Lancet 367:1241
Campodonico F, Benelli R, Michelazzi A, Ognio E, Toncini C, Maffezzini M (2004) Bladder cell culture on small intestinal submucosa as bioscaffold: experimental study on engineered urothelial grafts. Eur Urol 46:531
Kropp BP, Rippy MK, Badylak SF et al (1996) Regenerative urinary bladder augmentation using small intestinal submucosa: urodynamic and histopathologic assessment in long-term canine bladder augmentations. J Urol 155(6):2098–2104
Zhang Y (2008) Bladder reconstruction by tissue engineeringewith or without cells? J Urol 180:10
Sloff M, Simaioforidis V, de Vries R, Oosterwijk E, Feitz W (2014) Tissue engineering of the bladder–reality or myth? A systematic review. J Urol 192(4):1035–1042
Andersson KE (2014) Words of wisdom. Re: Tissue engineering of the bladder: reality or myth? A systematic review. Eur Urol;66(3):593.
Alberti C (2016) Whyever bladder tissue engineering clinical applications still remain unusual even though many intriguing technological advances have been reached? G Chir 37(1):6–12
Wang Y, Liao L (2014) Histologic and functional outcomes of small intestine submucosa-regenerated bladder tissue. BMC Urol 14:69
Zhang F, Liao L (2014) Tissue-engineered cystoplasty augmentation for treatment of neurogenic bladder using small intestinal submucosa: an exploratory study. J Urol 192(2):544–550
Zhang Y, Kropp BP, Lin HK, Cowan R, Cheng EY (2004) Bladder regeneration with cell-seeded small intestinal submucosa. Tissue Eng 10:181
Zhang Y, Frimberger D, Cheng EY, Lin HK, Kropp BP (2006) Challenges in a larger bladder replacement with cell-seeded and unseeded small intestinal submucosa grafts in a subtotal cystectomy model. BJU Int 98(5):1100–1105
Caione P, Boldrini R, Salerno A (2012) Bladder augmentation using acellular collagen biomatrix: a pilot experience in exstrophic patients. Pediatr Surg Int 28:421
Schaefer M, Kaiser A, Stehr M (2013) Bladder augmentation with small intestinal submucosa leads to unsatisfactory long-term results. J Pediatr Urol 9:878
Dewan P (2015) Re: Tissue engineered cystoplasty augmentation for treatment of neurogenic bladder using small intestinal submucosa: an exploratory study. J Urol 193(3):1067–1068
Liao L, Zhang F, Chen G (2014) New grading system for upper urinary tract dilation using magnetic resonance urography in patients with neurogenic bladder. BMC Urol 14:38
Liao L (2015) A new comprehensive classification system for both lower and upper urinary tract dysfunction in patients with neurogenic bladder. Urol Int 94(2):244–8.
Kispal Z, Balogh D, Erdei O et al (2011) Complications after bladder augmentation or substitution in children: a prospective study of 86 patients. BJU Int 108(2):282–9.
Biers SM, Venn SN, Greenwell TJ (2012) The past, present and future of augmentation cystoplasty. BJU Int 109(9):1280–1293
Gurung PM, Attar KH, Abdul-Rahman A, Morris T, Hamid R, Shah PJ (2012) Long-term outcomes of augmentation ileocystoplasty in patients with spinal cord injury: a minimum of 10 years of follow-up. BJU Int 109(8):1236–1242
Joseph DB, Borer JG, De Filippo RE, Hodges SJ, McLorie G (2014) Autologous cell seeded biodegradable scaffold for augmentation cystoplasty: phase II study in children and adolescents with spina bifida. J Urol 191:1389–1395
Zhang Y, Lin HK, Frimberger D, Epstein RB, Kropp BP (2005) Growth of bone marrow stromal cells on small intestinal submucosa: an alternative cell source for tissue engineered bladder. BJU Int 96(7):1120–1125
Soygur T, Burgu B, Zumrutbas A, Suer E (2010) The need for ureteric re-implantation during augmentation cystoplasty: video-urodynamic evaluation. BJU Int 105:530–532
Drake MJ, Apostolidis A, Emmanuel A, Gajewski J, Harrison SC, Heesakkers J et al (2013) Neurologic urinary and faecal incontinence. In: Abrams P, Cardozo L, Khoury S, Wein A (eds) Incontinence, 5th edn. ICUD-EAU, Paris, pp 827–954
Zhang Y, Liu G, Kropp BP (2012) Re-epithelialization of demucosalized stomach patch with tissue-engineered urothelial mucosa combined with Botox A in bladder augmentation. BJU Int 110(2 Pt 2):E106–E112
Wang Z, Liao L (2018) Effectiveness and complications of augmentation cystoplasty with or without nonrefluxing ureteral reimplantation in patients with bladder dysfunction: a single center 11-year experience. J Urol 199(1):200–205
Mondalek FG, Fung KM, Yang Q, Wu W, Lu W, Palmer BW et al (2015) Temporal expression of hyaluronic acid and hyaluronic acid receptors in a porcine small intestinal submucosa-augmented rat bladder regeneration model. World J Urol 33(8):1119–1128
Acknowledgements
This study was supported by Grants from the National Natural Scientific Foundation of (no.81570688).
Author information
Authors and Affiliations
Contributions
LL: project development, manuscript editing. FZ: data collection, data analysis, manuscript writing.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
All protocols involving human participants in this study were approved by the Ethics Committee of Capital Medical University, China and had informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Zhang, F., Liao, L. Long-term follow-up of neurogenic bladder patients after bladder augmentation with small intestinal submucosa. World J Urol 38, 2279–2288 (2020). https://doi.org/10.1007/s00345-019-03008-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-019-03008-x