Abstract
Purpose
To investigate the inhibitory effects of electrical stimulation of sacral dorsal root ganglion (DRG) on bladder activity under non-nociceptive and nociceptive bladder conditions in cats.
Materials and methods
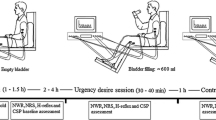
12 cats were divided into non-nociceptive and nociceptive groups. Saline was used to distend the bladder and induce non-nociceptive bladder activity, while acetic acid (AA, 0.25%) was used to induce nociceptive bladder overactivity, S1 or S2 DRG stimulation was applied via a pair of hook electrodes placed in the right S1 and S2 DRG.
Results
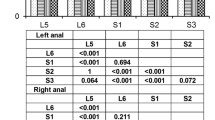
In both non-nociceptive and nociceptive groups, stimulation at 3 and 5 Hz significantly increased bladder capacity (BC) and no significantly different between the two frequencies. In non-nociceptive group, S1 DRG stimulation at 3 Hz was as effective (increasing BC to 139.7 ± 5.6 and 166.9 ± 12.21% of control at 1T and 3/2T, respectively) as S2 DRG stimulation (increases BC to 129.2 ± 5.6 and 160.5 ± 13.3% of control). In nociceptive group, AA reduced the BC to 62.6 ± 11.7% of saline control. S1 DRG stimulation at 3 Hz was also as effective (increasing BC to 54.9 ± 5.5 and 61.9 ± 6.0% of saline control at 1T and 3/2T, respectively) as S2 DRG stimulation (increases BC to 58.3 ± 3.7 and 65.6 ± 3.7% of control).
Conclusion
This study showed the effective inhibition on bladder activity under both non-nociceptive and nociceptive conditions, suggesting the possibility of sacral DRG stimulation to treat bladder overactivity.






Similar content being viewed by others
References
Abrams P, Cardozo L, Fall M et al (2003) The standardisation of terminology in lower urinary tract function: report from the standardisation sub-committee of the International Continence Society. Urology 61:37–49
van Kerrebroeck PE, van Voskuilen AC, Heesakkers JP (2007) Results of sacral neuromodulation therapy for urinary voiding dysfunction: outcomes of a prospective, worldwide clinical study. J Urol 178:2029–2034
Peters KM, Killinger KA, Boguslawski BM, Boura JA (2010) Chronic pudendal neuromodulation: expanding available treatment options for refractory urologic symptoms. Neurourol Urodyn 29:1267–1271
Macdiarmid SA, Peters KM, Shobeiri SA (2010) Long-term durability of percutaneous tibial nerve stimulation for the treatment of overactive bladder. J Urol 183:234–240
Yoshimura N, de Groat WC (1997) Neural control of the lower urinary tract. Int J Urol 4:111–125
Häbler HJ, Jänig W, Koltzenburg M (1990) Activation of unmyelinated afferent fibres by mechanical stimuli and inflammation of the urinary bladder in the cat. J Physiol 425:545–562
Liem L (2015) Stimulation of the dorsal root ganglion. Prog Neurol Surg 29:213–224
Pope JE, Deer TR, Kramer J (2013) A systematic review: current and future directions of dorsal root ganglion therapeutics to treat chronic pain. Pain Med 14:1477–1496
Bremer N, Ruby J, Weyker PD, Webb CA (2016) Neuromodulation: a focus on dorsal root ganglion stimulation. Pain Manag 6:205–209
Krames ES (2015) The dorsal root ganglion in chronic pain and as a target for neuromodulation: a review. Neuromodulation 18:24–32
Bruns TM, Weber DJ, Gaunt RA (2015) Microstimulation of afferents in the sacral dorsal root ganglia can evoke reflex bladder activity. Neurourol Urodyn 34:65–71
Yoo PB, Woock JW, Grill WM (2008) Bladder activation by selective stimulation of pudendal nerve afferents in the cat. Exp Neurol 212:218–225
Tai C, Wang J, Wang X, de Groat WC, Roppolo JR (2007) Bladder inhibition or voiding induced by pudendal nerve stimulation in chronic spinal cord injured cats. Neurourol Urodyn 26:570–577
Woock JP, Yoo PB, Grill WM (2008) Activation and inhibition of the micturition reflex by penile afferents in the cat. Am J Physiol Regul Integr Comp Physiol 294:1880–1889
Zhang F, Zhao S, Shen B et al (2013) Neural pathways involved in sacral neuromodulation of reflex bladder activity in cats. Am J Physiol Renal Physiol 304:710–717
Jänig W, Morrison JF (1986) Functional properties of spinal visceral afferents supplying abdominal and pelvic organs, with special emphasis on visceral nociception. Prog Brain Res 67:87–114
Fowler CJ, Griffiths D, de Groat WC (2008) The neural control of micturition. Nat Rev Neurosci 9:453–466
Häbler HJ, Jänig W, Koltzenburg M (1990) Activation of unmyelinated afferent fibres by mechanical stimuli and inflammation of the urinary bladder in the cat. J Physiol 425:545–562
Mally AD, Matsuta Y, Zhang F et al (2013) Role of opioid and metabotropic glutamate 5 receptors in pudendal inhibition of bladder overactivity in cats[J]. J Urol 189(4):1574
Tai C, Larson JA, Ogagan PD et al (2012) Differential role of opioid receptors in tibial nerve inhibition of nociceptive and nonnociceptive bladder reflexes in cats. Am J Physiol Renal Physiol 302:1090–1097
Chen ML, Shen B, Wang J et al (2010) Influence of naloxone on inhibitory pudendal-to-bladder reflex in cats. Exp Neurol 224:282–291
Xiao Z, Reese J, Schwen Z et al (2014) Role of spinal GABAA receptors in pudendal inhibition of nociceptive and nonnociceptive bladder reflexes in cats. Am J Physiol Renal Physiol 306:781–789
Jiang X, Fuller TW, Bandari J et al (2016) Contribution of GABAA, glycine, and opioid receptors to sacral neuromodulation of bladder overactivity in cats. J Pharmacol Exp Ther 359:436–441
Tai C, Chen M, Shen B (2011) Plasticity of urinary bladder reflexes evoked by stimulation of pudendal afferent nerves after chronic spinal cord injury in cats. Exp Neurol 228:109–117
Tai C, Shen B, Chen M, Wang J, Roppolo JR, de Groat WC (2011) Prolonged poststimulation inhibition of bladder activity induced by tibial nerve stimulation in cats. Am J Physiol Renal Physiol 300:385–392
Zhang Z, Bandari J, Bansal U et al (2017) Sacral neuromodulation of nociceptive bladder overactivity in cats. Neurourol Urodyn 36:1270–1277
Tai C, Shen B, Chen M et al (2011) Suppression of bladder overactivity by activation of somatic afferent nerves in the foot. Bju Int 107:303–309
Acknowledgements
This study were funded by the National Natural Science Foundation of China (No. 81570688) and Research Projects of China Rehabilitation Research Centre (2017ZX-31).
Author information
Authors and Affiliations
Contributions
Protocol/project development: LL and ZW; data collection or management: ZW, XL, GC, and HD; data analysis: ZW; and manuscript writing/editing: ZW.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical/IRB approval
Human subjects were not used in this study. All animal experiments were performed ethically in accordance with Capital Medical University guidelines for animal care and use.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Wang, Z., Liao, L., Deng, H. et al. The inhibitory effect of sacral dorsal root ganglion stimulation on nociceptive and nonnociceptive bladder reflexes in cats. World J Urol 36, 829–836 (2018). https://doi.org/10.1007/s00345-018-2198-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-018-2198-6