Abstract
Objective
To retrospectively evaluate the long-term outcomes after percutaneous cryoablation of abdominal wall endometriosis (AWE).
Method
The Institutional Review Board approved this retrospective observational review of 40 consecutive patients, of a median age of 37 years (interquartile range [IQR] 32–40 years), presenting with a total of 52 symptomatic AWE nodules. All patients underwent cryoablation between January 2013 and May 2022 with a minimum follow-up period of 12 months. Outcomes were assessed using a visual analog scale (VAS) that measured pain, as well as by magnetic resonance imaging (MRI). The pain-free survival rates were derived using the Kaplan–Meier estimator. Adverse events were analyzed and graded using the classification system of the Cardiovascular and Interventional Radiological Society of Europe.
Results
The median follow-up time was 40.5 months (IQR 26.5–47.2 months). The median VAS score before cryoablation was 8 (IQR 7–9). Complete relief of symptoms was documented in 80% (32/40) of patients at 3 months after initial cryoablation and correlated with the absence of residual endometriosis nodules on MRI. The median pain-free survival rates were 89.2% [95% CI, 70.1–96.4%] at 36 months and 76.8% [95% CI, 55.3–83.8%] after 60 months. No patient or lesion characteristics were found to be prognostic of failure. No major adverse events or side effects were reported in long term.
Conclusion
Cryoablation safely and effectively afforded long-term pain relief for patients with AWE nodules.
Clinical relevance statement
AWE cryoablation was found to be safe and effective in the long-term.
Key Points
• Cryoablation is highly effective with 80% of patients experiencing complete relief of AWE symptoms after a single procedure.
• Cryoablation is safe without long-term adverse events or side effects.
• The median pain-free survival rates are 89.2% at 36 months and 76.8% at 60 months.



Similar content being viewed by others
Abbreviations
- AWE:
-
Abdominal wall endometriosis
- CI:
-
Confidence interval
- CT:
-
Computed tomography
- IQR:
-
Interquartile range
- MRI:
-
Magnetic resonance imaging
- US:
-
Ultrasound
- VAS:
-
Visual analog scale
References
Carsote M, Terzea DC, Valea A, Gheorghisan-Galateanu AA (2020) Abdominal wall endometriosis (a narrative review). Int J Med Sci 17:536–542
Leite GKC, de Carvalho LFP, Korkes H, Guazzelli TF, Kenj G, de VianaToledo A (2009) Scar endometrioma following obstetric surgical incisions: retrospective study on 33 cases and review of the literature. Sao Paulo Med J. 127:270–7
Horton JD, DeZee KJ, Ahnfeldt EP, Wagner M (2008) Abdominal wall endometriosis: a surgeon’s perspective and review of 445 cases. Am J Surg 196:207–212
Najdawi M, Razakamanantsoa L, Mousseaux C et al (2023) Resolution of pain after percutaneous image-guided cryoablation of extraperitoneal endometriosis. J Vasc Interv Radiol 34:1192–1198
Kumar RR (2021) Spontaneous abdominal wall endometrioma: a case report. Int J Surg Case Rep 78:180–183
Yang E, Chen GD, Liao YH (2023) Spontaneous abdominal wall endometriosis: a case report and review of the literature. Taiwan J Obstet Gynecol 62:155–157
Ideyi SC, Schein M, Niazi M, Gerst PH (2003) Spontaneous endometriosis of the abdominal wall. Dig Surg 20:246–248
Raddaoui E, Ameeri S (2010) Abdominal wall endometriosis: a report of 2 cases with primary diagnosis by fine needle aspiration. Acta Cytol 54:214–216
Barat M, Dohan A, Kohi M et al (2023) Treatment of adenomyosis, abdominal wall endometriosis and uterine leiomyoma with interventional radiology: A review of current evidences. Diagn Interv Imaging 7:S2211-5684(23)00219-X. https://doi.org/10.1016/j.diii.2023.11.005
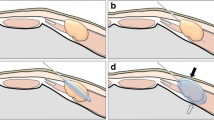
Cornelis F, Petitpierre F, Lasserre AS et al (2014) Percutaneous cryoablation of symptomatic abdominal scar endometrioma: initial reports. Cardiovasc Intervent Radiol 37:1575–1579
Maillot J, Brun JL, Dubuisson V, Bazot M, Grenier N, Cornelis FH (2017) Mid-term outcomes after percutaneous cryoablation of symptomatic abdominal wall endometriosis: comparison with surgery alone in a single institution. Eur Radiol 27:4298–4306
Dibble EH, D’Amico KC, Bandera CA, Littrup PJ (2017) Cryoablation of abdominal wall endometriosis: a minimally invasive treatment. AJR Am J Roentgenol 209:690–696
Jouffrieau C, Cazzato RL, Gabriele V et al (2023) Percutaneous imaging-guided cryoablation of endometriosis scars of the anterior abdominal wall. J Minim Invasive Gynecol 30:890-896. https://doi.org/10.1016/j.jmig.2023.06.018
Welch BT, Ehman EC, VanBuren WM et al (2020) Percutaneous cryoablation of abdominal wall endometriosis: the Mayo Clinic approach. Abdom Radiol (NY) 45(6):1813–1817
Smith KA, Welch BT, Kurup AN et al (2022) Feasibility and safety of percutaneous image-guided cryoablation of abdominal wall endometriosis. Abdom Radiol (NY) 47(8):2669–2673
Hensen JHJ, Van Breda Vriesman AC, Puylaert JBCM (2006) Abdominal wall endometriosis: clinical presentation and imaging features with emphasis on sonography. AJR Am J Roentgenol 186:616–620
Marcelin C, Brun JL, Caprais J et al (2024) Percutaneous cryoablation of symptomatic uterine adenomyomas: initial experience. J Gynecol Obstet Hum Reprod 53:102727
Havez M, Lippa N, Al-Ammari S et al (2014) Percutaneous image-guided cryoablation in inoperable extra-abdominal desmoid tumors: a study of tolerability and efficacy. Cardiovasc Intervent Radiol 37:1500–1506
Cornelis F, Neuville A, Labreze C et al (2013) Percutaneous cryotherapy of vascular malformation: initial experience. Cardiovasc Intervent Radiol 36:853–856
Filippiadis DK, Binkert C, Pellerin O, Hoffmann RT, Krajina A, Pereira PL (2017) Cirse Quality Assurance Document and Standards for Classification of Complications: The Cirse Classification System. Cardiovasc Intervent Radiol 40:1141–1146
Eisenhauer EA, Therasse P, Bogaerts J et al (2009) New response evaluation criteria in solid tumours: Revised RECIST guideline (version 1.1). Eur J Cancer j45:228–47
Barat M, Jannot AS, Dohan A, Soyer P (2022) How to report and compare quantitative variables in a radiology article. Diagn Interv Imaging 103:571–573
Littrup PJ, Bang HJ, Currier BP et al (2013) Soft-tissue cryoablation in diffuse locations: feasibility and intermediate term outcomes. J Vasc Interv Radiol 24:1817–1825
Cornelis F, Havez M, Lippa N et al (2013) Radiologically guided percutaneous cryotherapy for soft tissue tumours: a promising treatment. Diagn Interv Imaging 94:364–370
Tsoumakidou G, Buy X, Garnon J, Enescu J, Gangi A (2011) Percutaneous thermal ablation: how to protect the surrounding organs. Tech Vasc Interv Radiol 14:170–176
Kujak JL, Liu PT, Johnson GB, Callstrom MR (2010) Early experience with percutaneous cryoablation of extra-abdominal desmoid tumors. Skeletal Radiol 39:175–182
Zhao L, Deng Y, Wei Q, Chen J, Zhao C (2018) Comparison of ultrasound-guided high-intensity focused ultrasound ablation and surgery for abdominal wall endometriosis. Int J Hyperthermia 35:528–533
Carrafiello G, Fontana F, Pellegrino C et al (2009) Radiofrequency ablation of abdominal wall endometrioma. Cardiovasc Intervent Radiol 32:1300–1303
Wang Y, Wang W, Wang L, Wang J, Tang J (2011) Ultrasound-guided high-intensity focused ultrasound treatment for abdominal wall endometriosis: preliminary results. Eur J Radiol 79:56–59
Callstrom MR, Kurup AN (2009) Percutaneous ablation for bone and soft tissue metastases–why cryoablation? Skeletal Radiol 3:835–839
Cornelis FH, Labrèze C, Pinsolle V et al (2017) Percutaneous image-guided cryoablation as second-line therapy of soft-tissue venous vascular malformations of extremities: a prospective study of safety and 6-month efficacy. Cardiovasc Intervent Radiol 40:1358–1366
Melis M, Zager JS, Sondak VK (2008) Multimodality management of desmoid tumors: how important is a negative surgical margin? J Surg Oncol. 98:594–602
Horton JD, DeZee KJ, Ahnfeldt EP, Wagner M (2008) Abdominal wall endometriosis: a surgeon’s perspective and review of 445 cases. Am J Surg 196:207–212
Shafrir AL, Farland LV, Shah DK et al (2018) Risk for and consequences of endometriosis: a critical epidemiologic review. Best Pract Res Clin Obstet Gynaecol 51:1–15
Blanco RG, Parithivel VS, Shah AK, Gumbs MA, Schein M, Gerst PH (2003) 2003 Abdominal wall endometriomas. Am J Surg 185:596–598
Reddi Rani P, Soundararaghavan S, Rajaram P (1991) Endometriosis in abdominal scars - review of 27 cases. Int J Gynaecol Obstet 36(3):215–218
Bektaş H, Bilsel Y, Sari YS et al (2010) Abdominal wall endometrioma; a 10-year experience and brief review of the literature. J Surg Res 164:e77-81
Marras S, Pluchino N, Petignat P et al (2019) Abdominal wall endometriosis: an 11-year retrospective observational cohort study. Eur J Obstet Gynecol Reprod Biol X 4:100096
Encalada Soto D, Rassier S, Green IC, Burnett T, Khan Z, Cope A (2022) Endometriosis biomarkers of the disease: an update. Curr Opin Obstet Gynecol 34:210–219
Picod G, Boulanger L, Bounoua F, Leduc F, Duval G (2006) Abdominal wall endometriosis after caesarean section: report of fifteen cases. Gynecol Obstet Fertil 34:8–13
Touleimat S, Darwish B, Vassilieff M, Stochino Loi E, Hennetier C, Roman H (2017) Abdominal wall endometriosis following cesarean section: a study of the growth rate of parietal endometriosis implants. Minerva Ginecol 69:440–446
Razzouk K, Roman H, Chanavaz-Lacheray I, Scotté M, Verspyck E, Marpeau L (2007) Mixed clear cell and endometrioid carcinoma arising in parietal endometriosis. Gynecol Obstet Invest 63:140–142
Acknowledgements
MSK is funded through the NIH/NCI Cancer Center Support Grant P30 CA008748.
Funding
The authors state that this work has not received any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Francois H. Cornelis, MD, PhD.
Conflict of interest
Francois H. Cornelis is a consultant for GE HealthCare, Varian and IceCure.
The remaining authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was waived by the Institutional Review Board.
Ethical approval
Institutional Review Board approval was obtained.
Study subjects or cohorts overlap
Some study subjects or cohorts have been previously reported in Maillot J, Brun JL, Dubuisson V, Bazot M, Grenier N, Cornelis FH. Mid-term outcomes after percutaneous cryoablation of symptomatic abdominal wall endometriosis: comparison with surgery alone in a single institution. Eur Radiol. oct 2017;27(10):4298‑306.
Methodology
• retrospective
• cross-sectional study
• observational
• performed at one institution
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Marcelin, C., Maas, P., Jambon, E. et al. Long-term outcomes after percutaneous cryoablation of abdominal wall endometriosis. Eur Radiol (2024). https://doi.org/10.1007/s00330-024-10689-5
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00330-024-10689-5