Abstract
Objectives
Currently, there is no standardized measurement method for evaluating cup overhang (CO) in patients undergoing total hip arthroplasty (THA). We propose a novel, standardized method of measuring overhang distance in patients following primary total hip arthroplasty (THA) on computed tomography (CT) images after multiplanar reformation and compare it to a previously proposed measurement method on sagittal CT images.
Materials and methods
This retrospective study included patients who underwent primary THA with an anterior approach. Patients with cup overhang (CO) and iliopsoas impingement (IPI) were identified by clinical and imaging data. Uncorrected overhang distance (ODu) was evaluated on orthogonal sagittal CT images while corrected overhang distance (ODc) was evaluated on reformatted sagittal CT images corrected for pelvic rotation and aligned with the plane of the cup face.
Results
Out of 220 patients with THA, 23 patients (10.4%) with CO and 16 patients (7.3%) with IPI were identified. CO was significantly associated to IPI (p < 0.001). The inter- and intrareader agreement was almost perfect for ODc (κ = 0.822, κ = 0.850), whereas it was fair and moderate for ODu (κ = 0.391, κ = 0.455), respectively. The discriminative ability of ODc was excellent (area under the curve (AUC) = 0.909 (95% confidence interval (CI) 0.784–1.000)) in the receiver operating characteristic analysis. Conversely, AUC for ODu was poor, measuring 0.677 (95% CI 0.433–0.921).
Conclusion
We implemented a novel measurement method for CT images reformatted at the plane of the cup face to assess overhang distance in patients with CO following THA.
Clinical relevance statement
While further validation is necessary, the proposed method is characterized by its high reproducibility and might be used to predict the occurrence of iliopsoas impingement in patients with cup overhang following total hip arthroplasty.
Key Points
• A novel, standardized method of measuring cup overhang distance in patients following primary total hip arthroplasty on CT images is proposed.
• Cup overhang was associated to iliopsoas impingement. The proposed method was reproducible and showed excellent prediction of iliopsoas impingement in patients with cup overhang.
• This method can be implemented in clinical practice when assessing CT images of patients with cup overhang for iliopsoas impingement.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Primary total hip arthroplasty (THA) is the most common joint replacement, with 625,000 prostheses implanted in the USA between 2012 and 2019 [1]. While most THA have an excellent outcome, iliopsoas impingement (IPI) is an underrecognized cause of persistent groin pain in THA patients, with an incidence of approximately 2–7% [2,3,4]. Cup overhang (CO) is visible on computed tomography (CT) scans as overlap of the THA cup beyond the bony surface of the acetabulum [5] and can lead to iliopsoas tendon impingement and mechanical tendon irritation during hip flexion. CO can arise from oversized cups or a version mismatch between the cup and the native acetabulum of the patient [6,7,8,9] and has been identified as a risk factor for IPI, even though there is no consensus at which overhang distance patients become symptomatic [5, 7, 9,10,11,12]. Other suspected risk factors of IPI include female sex, leg length discrepancy, and retained cement or screw protrusion [13,14,15]. The diagnosis of IPI is made by analyzing the patient’s medical history, conducting a physical examination, and reviewing plain radiographs or computed tomography (CT) scans [2]. Additionally, ultrasonography or magnetic resonance imaging (MRI) can be employed to assess the presence of iliopsoas tendonitis [16].
Currently, there is no standardized method for precisely measuring overhang distance (OD) in patients with CO. Even though one study has shown the impact of pelvic tilt on OD measurements [17], all other studies that attempted to measure OD on non-reformatted CT images or plain radiographs have not yet taken the impact of acetabular inclination as well as pelvic rotation into account [7,8,9, 11, 18, 19].
Therefore, the purpose of this study was to propose a reproducible method for measuring OD in CT images after multiplanar reformation (MPR) and to compare it to a previously proposed measurement method on orthogonal sagittal images. Additionally, we aimed to evaluate the impact of the measured OD on the occurrence of iliopsoas impingement in patients undergoing primary THA.
Materials and methods
Patient selection
This single-center, retrospective study was approved by the local ethics committee (Cantonal ethics committee Zurich). All procedures conducted in this study adhered to the ethical standards established by the institutional and/or national research committee, in accordance with the principles outlined in the 1964 Helsinki Declaration and its subsequent amendments, or other comparable ethical guidelines.
To identify patients for our study, a query of the hospital’s information system retrieved records of all THAs performed with a direct anterior approach between January 2014 and December 2021 by various surgeons within our institution (Fig. 1). Prostheses were made of either cobalt-chromium-molybdenum alloy or titanium alloy. Patients who received THA due to secondary osteoarthritis (e.g., hip dysplasia), tumor, trauma, infection, and femoral head necrosis or patients who had a history of THA revision were excluded from this study. Subsequently, we accessed the radiology information system to identify patients who had undergone CT examinations of the pelvic region after surgery. CT was performed for complications after THA (118/220; 53.6%), for postoperative assessment of positioning of THA components (45/220; 20.5%), or for other clinical indications (57/220; 25.9%). All examinations were performed with spectral shaping (tin prefiltration) according to the local clinical standard. After applying these criteria, CT examinations of 261 patients were identified for further analysis. Patients with THA revision within the time interval from surgery to imaging as well as documented infection, aseptic loosening, periprosthetic fracture, or instability as reason for groin pain were excluded. This led to a final sample size of 220 patients. We assessed surgical or clinical reports and imaging data (magnetic resonance imaging and ultrasound) of this sample to identify documented cases of IPI. IPI diagnosis followed a clinical procedure performed by orthopedic surgeons. Firstly, a detailed history was taken in patients admitted for hip pain after THA, which included inquiring about the onset of symptoms, the location of the pain, and activities or movements that alleviated or aggravated the pain. Next, a physical examination was conducted to evaluate the range of motion, including palpation for areas of tenderness or muscle tightness. Additionally, specific clinical assessments for iliopsoas tightness, such as the Thomas Test, were conducted. Diagnosis of IPI was confirmed only if imaging supported the clinical diagnosis, which was defined as the presence of either iliopectineal bursitis or iliopsoas tendinopathy on MR or ultrasound images [2]. In a subgroup of patients, diagnosis was confirmed and treated through fluoroscopy-guided corticosteroid injections. CO on CT images was considered confirmed if the cup extended beyond the bony surface of the acetabulum.
Image analysis
CT scans were acquired on 64-slice and 128-slice CT scanners (Edge Plus, or Definition AS Plus; Siemens Healthineers, or Brilliance 64; Philips Healthcare) at 120–140 kVp for different clinical indications. Eighty-four out of the 220 CT examinations (38.2%) were performed with tin prefiltration. Slice thicknesses ranged from 1 to 2 mm. Two fellowship-trained radiologists (A.A.M., C.O.) analyzed the images for CO and independently performed OD measurements. Additionally, the first reader repeated the OD measurements after 3 months to assess intrareader agreement. Both readers were blinded to demographic and clinical data and analyzed the images independently and in random order on the local Picture Archiving and Communications (PACS) viewer (Merlin, Phoenix-PACS GmbH).
For measuring MPR-corrected OD (ODc), the following approach was conducted: First, a MPR of the CT scans was performed aided by maximum intensity projection (Fig. 2). In the axial plane, images were adjusted along the anterior superior iliac spine to account for pelvic rotation [20]. Next, the coronal MPR was angled along the plane of the cup face. Afterwards, the measurement was conducted by determining the distance from a line perpendicular to the cup circumference, originating from the point of which the anterior cup surface is exposed from the bone (Fig. 3). For the uncorrected measurement of OD (ODu), the anteroposterior distance of uncovered cup was measured on orthogonal sagittal images. All distances were measured in millimeters at the slice in which the maximum distance of the uncovered cup was visible. Both readers were allowed to adjust window levels individually to assess the boundary of the bone and to minimize metal artifacts. Additionally, the time for MPR preparation and measurement of ODc was timed with a stopwatch for both readers.
Multiplanar reformation of CT scans for corrected overhang distance measurement. Maximum intensity projection in the axial plane along the anterior superior iliac spine to correct for pelvic rotation (a) and angulation in the coronal plane along the plane of the cup face (b). The corrected overhang distance (ODc) is then measured on the corrected sagittal images parallel to the blue MPR reference line, as shown in Fig. 3. MPR, multiplanar reformation
The orthogonal sagittal CT image of a patient with cup overhang without multiplanar reformation (MPR): This uncorrected overhang distance (double arrows, ODu) is measured according to the current literature (a). After MPR-aided correction for pelvic rotation and with coronal MPR angled at the plane of the cup face (b), the measurement of the overhang distance perpendicular to the cup circumference is shown in the same patient (double arrows, ODc). All measurements were carried out at the slice in which the maximum distance of uncovered cup was visible
Statistical analysis
The statistical analyses were conducted using SPSS Statistics (v25, IBM Corp.). Normal distribution and homogeneity of variances for continuous variables were confirmed using the Shapiro–Wilk test and Levene’s test, respectively. Group differences were evaluated with Student’s t test in case of normal distribution and with the Mann–Whitney U test in case of non-normal distribution, while the chi-square analysis was conducted for categorical variables. Interreader and intrareader agreement was assessed by a kappa statistic (Cohen’s kappa). Receiver operating characteristic (ROC) curves were used to measure the predictive accuracy (area under the curve, AUC) for both measurement methods. AUC values > 0.9 were classified as “excellent” and values < 0.7 as “poor” [21]. The Youden index was used to aid with the selection of the optimal sensitivity and specificity threshold. p values < 0.05 were considered statistically significant.
Results
Patient characteristics, cup overhang, and iliopsoas impingement
Mean age at surgery was 62.7 ± 12.7 years and mean time from surgery to CT imaging was 390 ± 620 days (Table 1). IPI was documented in the clinical notes in 16 patients (7.3%), while 23 patients (10.4%) revealed CO on CT imaging (Tables 1 and 2). IPI was treated with corticosteroid injection in five patients (31.3%) and with iliopsoas tenotomy in three patients (18.8%), while eight patients (50.0%) were treated conservatively. An exemplary image of a patient with IPI and CO is depicted in Fig. 4. The Mann–Whitney U test revealed no significant differences for age, BMI, and time from surgery to CT imaging between the CO group (n = 23) and the non-CO group (n = 197) as well as between the IPI group (n = 16) and the non-IPI group (n = 204) (all p ≥ 0.242, Table 1). The chi-square analysis revealed a significant association of CO to IPI (p < 0.001, OR 35.20, 95% confidence interval (CI) 10.53–117.73). However, no significant association was found between sex and IPI (p = 0.205, OR 1.95, 95% CI 0.68–5.57).
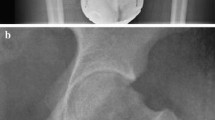
Exemplary images of a 64-year-old female patient with cup overhang and clinically diagnosed iliopsoas impingement following total hip arthroplasty. Sagittal CT images (a) clearly depicting the cup overhang. Axial STIR images of the right hip depicting fluid in the bursa iliopectinea as a sign of mechanical irritation of the iliopsoas tendon by cup overhang (b). STIR, short-tau inversion recovery
Results for corrected and uncorrected OD measurements
Mean ODu was 6.0 ± 2.8 mm, while ODc was 10.2 ± 4.1 mm. The interreader agreement was almost perfect for ODc (κ = 0.822) and fair for ODu (κ = 0.391). The intrareader agreement assessed after a time interval of 3 months was almost perfect for ODc (κ = 0.850) and moderate for ODu (κ = 0.455). The receiver operating characteristic (ROC) analysis revealed an excellent discrimination for ODc (AUC = 0.909, 95% CI 0.784–1.000) for identifying patients with IPI, whereas the discrimination ability for ODu was poor (AUC = 0.677, 95% CI 0.433–0.921; Fig. 5). The optimal cutoff value for diagnosing cup prominence was 7.5 mm (sensitivity = 90.9%, specificity = 77.8%) for ODc, whereas it was 6.4 mm (sensitivity = 80.8%, specificity = 49.1%) for ODu. The mean time for MPR preparation and ODc measurement was 10.6 ± 2.1 s.
Receiver operating characteristic curve for both overhang distance measure methods. Predictive accuracy for the presence of IPI was excellent for the MPR-corrected method (ODc: area under the curve (AUC) = 0.909, 95% CI 0.784–1.000) and poor for the uncorrected measurement method (ODu: AUC = 0.677, 95% CI 0.433–0.921). CO, cup overhang; MPR, multiplanar reformation
Discussion
This study aimed to implement a novel measurement method corrected with multiplanar reformation to assess overhang distance (OD) in patients with cup overhang (CO) following total hip arthroplasty and to compare it with a previously proposed measurement method on orthogonal sagittal CT images.
The first main finding of our study was that the proposed MPR-corrected method to measure OD (ODc) demonstrated an excellent inter- and intrareader agreement, corroborating its reliability and high reproducibility. The proposed method is easy to implement in clinical practice, since the MPR adjustment and overhang distance measurement process required only minimal time. On the other hand, uncorrected measurement of OD on orthogonal sagittal images (ODu) yielded an inter- and intrareader agreement that was much poorer. One possible explanation for this is the variability of the anterior border of the cup edge, primarily caused by variations in pelvic rotation and cup inclination. Figure 6 shows an example of the impact of different pelvic rotation and cup inclination on the measured OD, exemplified by the use of MPR.
Simulation of overhang distance measurements for didactic purposes (a, b). Uncorrected standard images, with standard orientation of the MPR reference lines on the axial (a) and coronal image (b) result in an underestimation of the cup overhang in the sagittal image (c), while MPR images corrected for pelvic rotation and angulation at the plane of the cup face (d, e) allow to measure the corrected overhang distance measurement (ODc, f). MPR, multiplanar reformation
The second main finding of this study was that cup overhang was significantly associated with the presence of IPI and that ODc was excellent at predicting IPI (AUC = 0.909 in the ROC analysis). In addition, the optimal threshold for diagnosing IPI with the corrected method demonstrated an excellent sensitivity, which is higher than in a recent study by Hardwick-Morris et al [12] that followed an approach similar to our uncorrected measurement. This finding is useful for the radiologist when evaluating CT images of patients with suspected IPI and will be valuable for the clinical decision making.
In the present study sample, IPI was observed with a relatively high frequency (7.3%), approaching the upper limit reported in the current literature [2,3,4]. This might be due to the fact that only patients receiving THA through a direct anterior approach were included in this study. The relationship between this surgical approach and the occurrence of IPI is explained by the disruption of the anterior hip capsule and resulting compromise of the important protective layer between the cup and the iliopsoas complex, possibly leading to tendon irritation [22]. This has also been reported in a study by Dora et al, in which the authors described that the iliopsoas muscle was seen through a defect of the neocapsule at the level of the uncovered cup [10].
Moreover, the present study found that female sex increased the risk of IPI by an odds ratio (OR) of 1.95, even though this finding was non-significant (p = 0.205). We believe that the lack of significance might be due to the small size of the IPI group, as in the current literature, the association between female sex and IPI has already been described [18]. This relationship is attributed to the smaller native acetabular diameters typically observed in women, which might constrain the surgeon to enlarge the acetabulum to insert a larger prosthetic femoral head, thus increasing the risk of cup overfitting [22, 23].
We acknowledge several limitations of the study. First, the retrospective design might have led to a selection bias and influenced the observed results. However, we believe that only including patients that underwent THA through a direct anterior approach and excluding patients with secondary osteoarthritis (e.g., due to hip dysplasia) strengthen the internal validity of our findings. Second, the sample size of this study was small, which may limit the generalizability of the findings. Moreover, we could only adjust for sex as a confounding variable when investigating the relationship between IPI, CO, and OD. Furthermore, given the novelty of the proposed MPR-corrected method for assessing OD following THA, we could not validate the reported measurement results with the existing literature.
In summary, this study implemented a novel, MPR-corrected measurement method to assess OD in patients with CO following THA. While further validation of the proposed method is necessary, our results indicate that it is highly reproducible and can be used to identify IPI in patients with CO and THA.
Abbreviations
- AUC:
-
Area under the curve
- CI:
-
Confidence interval
- CO:
-
Cup overhang
- IPI:
-
Iliopsoas impingement
- OD:
-
Overhang distance
- ODc :
-
Corrected overhang distance
- ODu :
-
Uncorrected overhang distance
- ROC:
-
Receiver operating characteristic
- THA:
-
Total hip arthroplasty
References
Springer BD, Levine BR, Golladay GJ (2021) Highlights of the 2020 American Joint Replacement Registry Annual Report. Arthroplast Today 9:141–142
Lachiewicz PF, Kauk JR (2009) Anterior iliopsoas impingement and tendinitis after total hip arthroplasty. J Am Acad Orthop Surg 17:337–344
Howell M, Rae FJ, Khan A, Holt G (2021) Iliopsoas pathology after total hip arthroplasty: a young person’s complication. Bone Joint J 103:305–308
Bartelt RB, Yuan BJ, Trousdale RT, Sierra RJ (2010) The prevalence of groin pain after metal-on-metal total hip arthroplasty and total hip resurfacing. Clin Orthop Relat Res 468:2346–2356
Cyteval C, Sarrabère MP, Cottin A et al (2003) Iliopsoas impingement on the acetabular component: radiologic and computed tomography findings of a rare hip prosthesis complication in eight cases. J Comput Assist Tomogr 27:183–188
Zhu J, Li Y, Chen K et al (2019) Iliopsoas tendonitis following total hip replacement in highly dysplastic hips: a retrospective study. J Orthop Surg Res 14:1–8
Ueno T, Kabata T, Kajino Y, Inoue D, Ohmori T, Tsuchiya H (2018) Risk factors and cup protrusion thresholds for symptomatic iliopsoas impingement after total hip arthroplasty: a retrospective case-control study. J Arthroplasty 33:3288-3296.e3281
Batailler C, Bonin N, Wettstein M et al (2017) Outcomes of cup revision for ilio-psoas impingement after total hip arthroplasty: retrospective study of 46 patients. Orthop Traumatol Surg Res 103:1147–1153
Tamaki Y, Goto T, Wada K, Omichi Y, Hamada D, Sairyo K (2022) Increased hip flexion angle and protrusion of the anterior acetabular component can predict symptomatic iliopsoas impingement after total hip arthroplasty: a retrospective study. Hip Int 33:985–991
Dora C, Houweling M, Koch P, Sierra RJ (2007) Iliopsoas impingement after total hip replacement: the results of non-operative management, tenotomy or acetabular revision. J Bone Joint Surg Br 89:1031–1035
Carbonell-Rosell C, Soza D, Pujol O, de Albert de Delás-Vigo M, Antón A, Barro V (2022) Iliopsoas impingement after total hip arthroplasty: does the CT-scan have any role? Our algorithm proposal. J Orthop 34:137–141
Hardwick-Morris M, Twiggs J, Miles B et al (2023) Iliopsoas tendonitis after total hip arthroplasty: an improved detection method with applications to preoperative planning. Bone Jt Open 4:3–12
Taher RT, Power RA (2003) Iliopsoas tendon dysfunction as a cause of pain after total hip arthroplasty relieved by surgical release. J Arthroplasty 18:387–388
Park HS, Lee SH, Cho HM, Choi HB, Jo S (2021) Screw penetration of the iliopsoas muscle causing late-onset pain after total hip arthroplasty: a case report. World J Clin Cases 9:10006–10012
Paraschos OA, Harris WT, Owens JS, Lall AC, Domb BG (2023) Arthroscopic peripheral compartment iliopsoas release for iliopsoas impingement after primary total hip arthroplasty. Arthrosc Tech 12:e115–e120
Rezig R, Copercini M, Montet X, Martinoli C, Bianchi S (2004) Ultrasound diagnosis of anterior iliopsoas impingement in total hip replacement. Skeletal Radiol 33:112–116
Ueno T, Kabata T, Kajino Y et al (2019) Tilt-adjusted cup anteversion in patients with severe backward pelvic tilt is associated with the risk of iliopsoas impingement: a three-dimensional implantation simulation. Clin Orthop Relat Res 477:2243–2254
Weber M, Woerner M, Messmer B, Grifka J, Renkawitz T (2017) Navigation is equal to estimation by eye and palpation in preventing psoas impingement in THA. Clin Orthop Relat Res 475:196–203
Chalmers BP, Sculco PK, Sierra RJ, Trousdale RT, Berry DJ (2017) Iliopsoas impingement after primary total hip arthroplasty: operative and nonoperative treatment outcomes. J Bone Joint Surg Am 99:557–564
Schwarz TJ, Weber M, Dornia C et al (2017) Correction of pelvic tilt and pelvic rotation in cup measurement after THA - an experimental study. Rofo 189:864–873
de Hond AAH, Steyerberg EW, van Calster B (2022) Interpreting area under the receiver operating characteristic curve. Lancet Digit Health 4:e853–e855
Buller LT, Menken LG, Hawkins EJ et al (2021) Iliopsoas impingement after direct anterior approach total hip arthroplasty: epidemiology, risk factors, and treatment options. J Arthroplasty 36:1772–1778
Vandenbussche E, Saffarini M, Taillieu F, Mutschler C (2008) The asymmetric profile of the acetabulum. Clin Orthop Relat Res 466:417–423
Acknowledgement
The authors would like to thank Sabine Schrimpf for proofreading the manuscript.
Funding
Open access funding provided by University of Zurich. The authors state that this work has not received any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Reto Sutter, MD.
Conflict of interest
Prof. Reto Sutter is receiving royalties for his position as a book editor at Breitenseher Publisher. The remaining authors do not have any conflict of interest to declare.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was obtained by all participants.
Ethical approval
This single-center, retrospective study was approved by the local ethics committee (Kantonale Ethikkommission Zürich).
Study subjects or cohorts overlap
No.
Methodology
• retrospective
• observational
• performed at one institution
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Marth, A.A., Ofner, C., Zingg, P.O. et al. Quantifying cup overhang after total hip arthroplasty: standardized measurement using reformatted computed tomography and association of overhang distance with iliopsoas impingement. Eur Radiol 34, 4300–4308 (2024). https://doi.org/10.1007/s00330-023-10479-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-023-10479-5