Abstract
Objective
The study aimed to compare ZOOMit diffusion-weighted imaging (DWI) MRI with conventional DWI MRI for visualizing small bones in the foot, soft tissue abscesses, and osteomyelitis.
Materials and methods
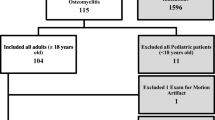
The cohort consisted of a consecutive series of patients with potential foot and ankle infections referred for MR imaging. Patients were imaged using both conventional and ZOOMit DWI in the same setting. Blinded reads were then conducted in separate settings and independent of known clinical diagnosis by two expert radiologists. The results from the reads were compared statistically using paired t-tests and with biopsy specimen analysis, both anatomopathological and microbiological.
Results
There was improvement in fat suppression using ZOOMit sequence compared to conventional DWI (p = .001) with no significant difference in motion artifacts (p = .278). ZOOMit had a higher rate of concordance with pathology findings for osteomyelitis (72%, 31/43 cases) compared with conventional DWI (60%, 26/43 cases). ZOOMit also identified 46 additional small bones of the foot and ankle (405/596, 68.0%) than conventional DWI (359/596, 60.2%). Conventional DWI however exhibited a more negative contrast-to-noise ratio (CNR) than ZOOMit (p = 0.001).
Conclusion
ZOOMit DWI improves distal extremity proton diffusion assessment and helps visualize more bones in the foot, with less image distortion and improved fat saturation at the expense of reduced CNR. This makes it a viable option for assessing lower extremity infections.
Clinical relevance statement
This study highlights the novel utilization of ZOOMit diffusion-weighted imaging (DWI) for the assessment of lower extremity lesions compared to conventional DWI.
Key Points
• Distal extremity diffusion-weighted imaging (DWI) is often limited.
• ZOOMit DWI displayed improved fat suppression with less motion artifacts and better visualization of the lower extremity bones than conventional DWI.
• ZOOMit shows decreased contrast-to-noise ratio than conventional DWI.






Similar content being viewed by others
Abbreviations
- ACR:
-
American College of Radiology
- ADC:
-
Apparent diffusion coefficient
- CNR:
-
Contrast-to-noise ratio
- DFO:
-
Diabetic foot osteomyelitis
- DWI:
-
Diffusion-weighted imaging
- ICC:
-
Intraclass observer correlation
- MoCI:
-
Motion correct imaging
- MSK:
-
Musculoskeletal
- MT:
-
Metatarsal
- OM:
-
Osteomyelitis
- RESOLVE:
-
Readout segmentation of long variable echo-trains
- SD:
-
Standard deviation
- SNR:
-
Signal-to-noise ratio
- SPAIR:
-
Spectral adiabatic inversion recovery fat saturation
- T1W:
-
T-1 weighted
- T2W:
-
T-2 weighted
References
Sia IG, Berbari EF (2006) Infection and musculoskeletal conditions: osteomyelitis. Best Pract Res Clin Rheumatol. 20(6):1065–81. https://doi.org/10.1016/j.berh.2006.08.014
Kremers HM, Nwojo ME, Ransom JE, Wood-Wentz CM, Melton LJ 3rd, Huddleston PM 3rd (2015) Trends in the epidemiology of osteomyelitis: a population-based study, 1969 to 2009. J Bone Joint Surg Am. 97(10):837–45. https://doi.org/10.2106/JBJS.N.01350
Geraghty T, LaPorta G (2019) Current health and economic burden of chronic diabetic osteomyelitis. Expert Rev Pharmacoecon Outcomes Res. 19(3):279–286. https://doi.org/10.1080/14737167.2019.1567337
Rice JB, Desai U, Cummings AK, Birnbaum HG, Skornicki M, Parsons NB (2014) Burden of diabetic foot ulcers for medicare and private insurers. Diabetes Care. 37(3):651–8. https://doi.org/10.2337/dc13-2176
Lee YJ, Sadigh S, Mankad K, Kapse N, Rajeswaran G (2016) The imaging of osteomyelitis. Quant Imaging Med Surg. 6(2):184–98. https://doi.org/10.21037/qims.2016.04.01
Luchs JS, Hines J, Katz DS, Athanasian EA (2002) MR imaging of squamous cell carcinoma complicating chronic osteomyelitis of the femur. AJR Am J Roentgenol. 178(2):512–3. https://doi.org/10.2214/ajr.178.2.1780512
Bauer T, David T, Rimareix F, Lortat-Jacob A (2007) Ulcere de Marjolin sur osteite chronique: diagnostic et resultats du traitement: 7 cas. [Marjolin’s ulcer in chronic osteomyelitis: seven cases and a review of the literature]. Rev Chir Orthop Reparatrice Appar Mot. 93(1):63–71. https://doi.org/10.1016/s0035-1040(07)90205-6
Expert Panel on Musculoskeletal I, Beaman FD, von Herrmann PF et al (2017) ACR Appropriateness Criteria((R)) suspected osteomyelitis, septic arthritis, or soft tissue infection (excluding spine and diabetic foot). J Am Coll Radiol. 14(5S):S326–S337. https://doi.org/10.1016/j.jacr.2017.02.008
Harish S, Chiavaras MM, Kotnis N, Rebello R (2011) MR imaging of skeletal soft tissue infection: utility of diffusion-weighted imaging in detecting abscess formation. Skeletal Radiol. 40(3):285–94. https://doi.org/10.1007/s00256-010-0986-1
Kim Y, Lee SK, Kim JY, Kim JH (2023) Pitfalls of diffusion-weighted imaging: clinical utility of T2 shine-through and T2 black-out for musculoskeletal diseases. Diagnostics (Basel) 13(9). https://doi.org/10.3390/diagnostics13091647
Towers JD (1997) The use of intravenous contrast in MRI of extremity infection. Semin Ultrasound CT MR. 18(4):269–75. https://doi.org/10.1016/s0887-2171(97)80017-0
Chun CW, Jung JY, Baik JS, Jee WH, Kim SK, Shin SH (2018) Detection of soft-tissue abscess: comparison of diffusion-weighted imaging to contrast-enhanced MRI. J Magn Reson Imaging. 47(1):60–68. https://doi.org/10.1002/jmri.25743
Kumar Y, Khaleel M, Boothe E, Awdeh H, Wadhwa V, Chhabra A (2017) Role of diffusion weighted imaging in musculoskeletal infections: current perspectives. Eur Radiol. 27(1):414–423. https://doi.org/10.1007/s00330-016-4372-9
Bhojwani N, Szpakowski P, Partovi S et al (2015) Diffusion-weighted imaging in musculoskeletal radiology-clinical applications and future directions. Quant Imaging Med Surg. 5(5):740–53. https://doi.org/10.3978/j.issn.2223-4292.2015.07.07
Spinnato P, Patel DB, Di Carlo M et al (2022) Imaging of musculoskeletal soft-tissue infections in clinical practice: a comprehensive updated review. Microorganisms 10(12). https://doi.org/10.3390/microorganisms10122329
Salastekar N, Su A, Rowe JS, Somasundaram A, Wong PK, Hanna TN (2023) Imaging of soft tissue infections. Radiol Clin North Am. 61(1):151–166. https://doi.org/10.1016/j.rcl.2022.08.003
Zaitsev M, Maclaren J, Herbst M (2015) Motion artifacts in MRI: a complex problem with many partial solutions. J Magn Reson Imaging. 42(4):887–901. https://doi.org/10.1002/jmri.24850
Van de Walle R, Lemahieu I, Achten E (1997) Magnetic resonance imaging and the reduction of motion artifacts: review of the principles. Technol Health Care. 5(6):419–35
Wood ML, Henkelman RM (1985) MR image artifacts from periodic motion. Med Phys. 12(2):143–51. https://doi.org/10.1118/1.595782
Liu W, Liu H, Xie S et al (2022) Comparing the clinical utility of single-shot, readout-segmented and zoomit echo-planar imaging in diffusion-weighted imaging of the kidney at 3 T. Sci Rep. 12(1):12389. https://doi.org/10.1038/s41598-022-16670-w
Guirguis M, Sharan G, Wang J, Chhabra A (2022) Diffusion-weighted MR imaging of musculoskeletal tissues: incremental role over conventional MR imaging in bone, soft tissue, and nerve lesions. BJR Open. 4(1):20210077. https://doi.org/10.1259/bjro.20210077
Kruk KA, Dietrich TJ, Wildermuth S et al (2022) Diffusion-weighted imaging distinguishes between osteomyelitis, bone marrow edema, and healthy bone on forefoot magnetic resonance imaging. J Magn Reson Imaging. 56(5):1571–1579. https://doi.org/10.1002/jmri.28091
Eren MA, Karakas E, Torun AN, Sabuncu T (2019) The clinical value of diffusion-weighted magnetic resonance imaging in diabetic foot infection. J Am Podiatr Med Assoc. 109(4):277–281. https://doi.org/10.7547/17-066
Cicchetti D (1994) Guidelines, criteria, and rules of thumb for evaluating normed and standardized assessment instrument in psychology. Psychol Assess. 6:284–290. https://doi.org/10.1037/1040-3590.6.4.284
Khoo MM, Tyler PA, Saifuddin A, Padhani AR (2011) Diffusion-weighted imaging (DWI) in musculoskeletal MRI: a critical review. Skeletal Radiol. 40(6):665–81. https://doi.org/10.1007/s00256-011-1106-6
Schaefer PW, Copen WA, Lev MH, Gonzalez RG (2006) Diffusion-weighted imaging in acute stroke. Magn Reson Imaging Clin N Am. 14(2):141–68. https://doi.org/10.1016/j.mric.2006.06.005
Baur A, Stäbler A, Brüning R et al (1998) Diffusion-weighted MR imaging of bone marrow: differentiation of benign versus pathologic compression fractures. Radiology. 207(2):349–56. https://doi.org/10.1148/radiology.207.2.9577479
Chan JH, Peh WC, Tsui EY et al (2002) Acute vertebral body compression fractures: discrimination between benign and malignant causes using apparent diffusion coefficients. Br J Radiol. 75(891):207–14. https://doi.org/10.1259/bjr.75.891.750207
Weaver JS, Omar IM, Mar WA et al (2022) Magnetic resonance imaging of musculoskeletal infections. Pol J Radiol. 87:e141–e162. https://doi.org/10.5114/pjr.2022.113825
Dallaudière B, Lecouvet F, Vande Berg B et al (2015) Diffusion-weighted MR imaging in musculoskeletal diseases: current concepts. Diagn Interv Imaging. 96(4):327–40. https://doi.org/10.1016/j.diii.2014.10.008
Chaturvedi A (2021) Pediatric skeletal diffusion-weighted magnetic resonance imaging: part 1 - technical considerations and optimization strategies. Pediatr Radiol. 51(9):1562–1574. https://doi.org/10.1007/s00247-021-04975-3
Funding
The authors state that this work has not received any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Dr. Avneesh Chhabra, MD, MBA, FACR.
Conflict of interest
The authors of this manuscript declare relationships with the following companies:
Avneesh Chhabra: Consultant: ICON Medical and TREACE Medical Concepts Inc., Book Royalties: Jaypee, Wolters, Speaker: Siemens, Medical advisor: Image Biopsy Lab Inc., Research grant: Image biopsy Lab Inc.
Avneesh Chhabra is a Deputy Editor in European Radiology. He has not taken part in the review or selection process of this article.
The other authors declare no conflict of interest for this work.
Statistics and biometry
One of the authors, Dr. Yin Xi, PhD, has significant statistical expertise.
Informed consent
Written informed consent was obtained from all participants.
Ethical approval
Institutional Review Board approval of UT Southwestern was obtained.
Study subjects or cohorts overlap
None.
Methodology
• prospective
• observational
• performed at one institution
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Xia, S., Gowda, P., Silva, F.D. et al. Comparison between ZOOMit DWI and conventional DWI in the assessment of foot and ankle infection: a prospective study. Eur Radiol 34, 3483–3492 (2024). https://doi.org/10.1007/s00330-023-10315-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-023-10315-w