Abstract
Objective
To develop a bimodal nomogram to reduce unnecessary biopsies in breast lesions with discordant ultrasound (US) and mammography (MG) Breast Imaging Reporting and Data System (BI-RADS) assessments.
Methods
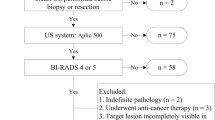
This retrospective study enrolled 706 women following opportunistic screening or diagnosis with discordant US and MG BI-RADS assessments (where one assessed a lesion as BI-RADS 4 or 5, while the other assessed the same lesion as BI-RADS 0, 2, or 3) from two medical centres between June 2019 and June 2021. Univariable and multivariable logistic regression analyses were used to develop the nomogram. DeLong’s and McNemar’s tests were used to assess the model’s performance.
Results
Age, MG features (margin, shape, and density in masses, suspicious calcifications, and architectural distortion), and US features (margin and shape in masses as well as calcifications) were independent risk factors for breast cancer. The nomogram obtained an area under the curve of 0.87 (95% confidence interval (CI), 0.83–0.91), 0.91 (95% CI, 0.87 – 0.96), and 0.92 (95% CI, 0.86–0.98) in the training, internal validation, and external testing samples, respectively, and demonstrated consistency in calibration curves. Coupling the nomogram with US reduced unnecessary biopsies from 74 to 44% and the missed malignancies rate from 13 to 2%. Similarly, coupling with MG reduced missed malignancies from 20 to 6%, and 63% of patients avoided unnecessary biopsies. Interobserver agreement between US and MG increased from – 0.708 (poor agreement) to 0.700 (substantial agreement) with the nomogram.
Conclusion
When US and MG BI-RADS assessments are discordant, incorporating the nomogram may improve the diagnostic accuracy, avoid unnecessary breast biopsies, and minimise missed diagnoses.
Clinical relevance statement
The nomogram developed in this study could be used as a computer program to assist radiologists with detecting breast cancer and ensuring more precise management and improved treatment decisions for breast lesions with discordant assessments in clinical practice.
Key Points
• Coupling the nomogram with US and mammography improves the detection of breast cancers without the risk of unnecessary biopsy or missed malignancies.
• The nomogram increases mammography and US interobserver agreement and enhances the consistency of decision-making.
• The nomogram has the potential to be a computer program to assist radiologists in identifying breast cancer and making optimal decisions.





Similar content being viewed by others
Abbreviations
- ACR:
-
American College of Radiology
- AUC:
-
Area under the curve
- BI-RADS:
-
Breast Imaging Reporting and Data System
- CEUS:
-
Contrast-enhanced US
- CI:
-
Confidence interval
- MG:
-
Mammography
- OR:
-
Odds ratio
- ROC:
-
Receiver operator characteristic curve
- SWE:
-
Shear wave elastography
- US:
-
Ultrasound
References
Lawson MB, Bissell M, Miglioretti DL et al (2022) Multilevel factors associated with time to biopsy after abnormal screening mammography results by race and ethnicity. JAMA Oncol 8:1115–1126
Ohuchi N, Suzuki A, Sobue T et al (2016) Sensitivity and specificity of mammography and adjunctive ultrasonography to screen for breast cancer in the Japan Strategic Anti-cancer Randomized Trial (J-START): a randomised controlled trial. Lancet 387:341–348
Rebolj M, Assi V, Brentnall A, Parmar D, Duffy SW (2018) Addition of ultrasound to mammography in the case of dense breast tissue: systematic review and meta-analysis. Br J Cancer 118:1559–1570
Mann RM, Athanasiou A, Baltzer PA et al (2022) Breast cancer screening in women with extremely dense breasts recommendations of the European Society of Breast Imaging (EUSOBI). Eur Radiol 32:4036–4045
Goh JHL, Tan TL, Aziz S, Rizuana IH (2022) Comparative study of digital breast tomosynthesis (DBT) with and without ultrasound versus breast magnetic resonance imaging (MRI) in detecting breast lesion. Int J Environ Res Public Health 19:759
Berg WA, Blume JD, Cormack JB et al (2008) Combined screening with ultrasound and mammography vs mammography alone in women at elevated risk of breast cancer. JAMA 299:2151–2163
Shen Y, Shamout FE, Oliver JR et al (2021) Artificial intelligence system reduces false-positive findings in the interpretation of breast ultrasound exams. Nat Commun 12(1):5645
Liu H, Zhan H, Sun D (2020) Comparison of 99mTc-MIBI scintigraphy, ultrasound, and mammography for the diagnosis of BI-RADS 4 category lesions. BMC Cancer 20(1):1–8
Barba D, Leon-Sosa A, Lugo P et al (2021) Breast cancer, screening and diagnostic tools: all you need to know. Crit Rev Oncol Hematol 157:103174
Berg WA, Zhang Z, Lehrer D et al (2012) Detection of breast cancer with addition of annual screening ultrasound or a single screening MRI to mammography in women with elevated breast cancer risk. JAMA 307(13):1394–1404
Qian X, Pei J, Zheng H et al (2021) Prospective assessment of breast cancer risk from multimodal multiview ultrasound images via clinically applicable deep learning. Nat Biomed Eng 5(6):522–532
Shao SH, Li CX, Yao MH, Li G, Li X, Wu R (2020) Incorporation of contrast-enhanced ultrasound in the differential diagnosis for breast lesions with inconsistent results on mammography and conventional ultrasound. Clin Hemorheol Microcirc 74:463–473
Pu H, Zhang XL, Xiang LH et al (2019) The efficacy of added shear wave elastography (SWE) in breast screening for women with inconsistent mammography and conventional ultrasounds (US). Clin Hemorheol Microcirc 71:83–94
Luo S, Yao G, Hong Z et al (2019) Qualitative classification of shear wave elastography for differential diagnosis between benign and metastatic axillary lymph nodes in breast cancer. Front Oncol 9:533
Kajiwara Y, Oka S, Tanaka S et al (2023) Nomogram as a novel predictive tool for lymph node metastasis in T1 colorectal cancer treated with endoscopic resection: a nationwide, multicenter study. Gastrointest Endosc. https://doi.org/10.1016/j.gie.2023.01.022
Wang XY, Cui LG, Feng J, Chen W (2021) Artificial intelligence for breast ultrasound: an adjunct tool to reduce excessive lesion biopsy. Eur J Radiol 138:109624
Raza S, Goldkamp AL, Chikarmane SA, Birdwell RL (2010) US of breast masses categorized as BI-RADS 3, 4, and 5: pictorial review of factors influencing clinical management. Radiographics 30:1199–1213
Xie Y, Zhu Y, Chai W et al (2022) Downgrade BI-RADS 4A patients using nomogram based on breast magnetic resonance imaging, ultrasound, and mammography. Front Oncol 12:807402
Cai Y, Zhu C, Chen Q, Zhao F, Guo S (2021) Application of a second opinion ultrasound in breast imaging reporting and data system 4A cases: can immediate biopsy be avoided? J Int Med Res 49:675881916
Niu S, Huang J, Li J et al (2020) Application of ultrasound artificial intelligence in the differential diagnosis between benign and malignant breast lesions of BI-RADS 4A. BMC Cancer 20:1–7
Hong AS, Rosen EL, Soo MS, Baker JA (2005) BI-RADS for sonography: positive and negative predictive values of sonographic features. AJR Am J Roentgenol 184:1260–1265
Tan PS, Ali MA, Eriksson M, Hall P, Humphreys K, Czene K (2021) Mammography features for early markers of aggressive breast cancer subtypes and tumor characteristics: a population-based cohort study. Int J Cancer 148:1351–1359
Choi WJ, Han K, Shin HJ, Lee J, Kim E, Yoon JH (2021) Calcifications with suspicious morphology at mammography: should they all be considered with the same clinical significance? Eur Radiol 31:2529–2538
Rauch GM, Hobbs BP, Kuerer HM et al (2016) Microcalcifications in 1657 Patients with pure ductal carcinoma in situ of the breast: correlation with clinical, histopathologic, biologic features, and local recurrence. Ann Surg Oncol 23:482–489
Hofvind S, Iversen BF, Eriksen L, Styr BM, Kjellevold K, Kurz KD (2011) Mammographic morphology and distribution of calcifications in ductal carcinoma in situ diagnosed in organized screening. Acta Radiol 52:481–487
Kerlikowske K, Zhu W, Tosteson AN et al (2015) Identifying Women with dense breasts at high risk for interval cancer. Ann Intern Med 162:673–681
Tagliafico AS, Calabrese M, Mariscotti G et al (2016) Adjunct screening with tomosynthesis or ultrasound in women with mammography-negative dense breasts: interim report of a prospective comparative trial. J Clin Oncol 34:1882–1888
Funding
This study has received funding by the National Natural Science Foundation of China (82271998 and 82071949), College Students’ Innovative Entrepreneurial Training Plan Program (202212121022), and Guangzhou Municipal Science and Technology Department: 2023 Key research and development plan projects (2023B03J1350).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Guarantor
The scientific guarantor of this publication is Yingjia Li.
Conflict of interest
The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Statistics and biometry
One of the authors has significant statistical expertise.
Informed consent
Written informed consent was waived by the Institutional Review Board.
Ethical approval
Institutional Review Board approval was obtained (NFEC-2020-294).
Study subjects or cohorts overlap
No study subjects or cohorts have been previously reported.
Methodology
• Retrospective
• Diagnostic study
• Multicentre study
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Xu, Z., Lin, Y., Huo, J. et al. A bimodal nomogram as an adjunct tool to reduce unnecessary breast biopsy following discordant ultrasonic and mammographic BI-RADS assessment. Eur Radiol 34, 2608–2618 (2024). https://doi.org/10.1007/s00330-023-10255-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-023-10255-5