Abstract
Objectives
To analyze the diagnostic performance and prognostic value of CT-defined visceral pleural invasion (CT-VPI) in early-stage lung adenocarcinomas.
Methods
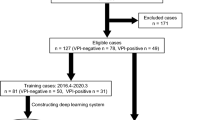
Among patients with clinical stage I lung adenocarcinomas, half of patients were randomly selected for a diagnostic study, in which five thoracic radiologists determined the presence of CT-VPI. Probabilities for CT-VPI were obtained using deep learning (DL). Areas under the receiver operating characteristic curve (AUCs) and binary diagnostic measures were calculated and compared. Inter-rater agreement was assessed. For all patients, the prognostic value of CT-VPI by two radiologists and DL (using high-sensitivity and high-specificity cutoffs) was investigated using Cox regression.
Results
In 681 patients (median age, 65 years [interquartile range, 58–71]; 382 women), pathologic VPI was positive in 130 patients. For the diagnostic study (n = 339), the pooled AUC of five radiologists was similar to that of DL (0.78 vs. 0.79; p = 0.76). The binary diagnostic performance of radiologists was variable (sensitivity, 45.3–71.9%; specificity, 71.6–88.7%). Inter-rater agreement was moderate (weighted Fleiss κ, 0.51; 95%CI: 0.43–0.55). For overall survival (n = 680), CT-VPI by radiologists (adjusted hazard ratio [HR], 1.27 and 0.99; 95%CI: 0.84–1.92 and 0.63–1.56; p = 0.26 and 0.97) or DL (HR, 1.44 and 1.06; 95%CI: 0.86–2.42 and 0.67–1.68; p = 0.17 and 0.80) was not prognostic. CT-VPI by an attending radiologist was prognostic only in radiologically solid tumors (HR, 1.82; 95%CI: 1.07–3.07; p = 0.03).
Conclusion
The diagnostic performance and prognostic value of CT-VPI are limited in clinical stage I lung adenocarcinomas. This feature may be applied for radiologically solid tumors, but substantial reader variability should be overcome.
Clinical relevance statement
Although the diagnostic performance and prognostic value of CT-VPI are limited in clinical stage I lung adenocarcinomas, this parameter may be applied for radiologically solid tumors with appropriate caution regarding inter-reader variability.
Key Points
• Use of CT-defined visceral pleural invasion in clinical staging should be cautious, because prognostic value of CT-defined visceral pleural invasion remains unexplored.
• Diagnostic performance and prognostic value of CT-defined visceral pleural invasion varied among radiologists and deep learning.
• Role of CT-defined visceral pleural invasion in clinical staging may be limited to radiologically solid tumors.






Similar content being viewed by others
Abbreviations
- AUC:
-
Area under the receiver operating characteristic curve
- DL:
-
Deep learning
- HR:
-
Hazard ratio
- IQR:
-
Interquartile range
- NPV:
-
Negative predictive value
- NSCLC:
-
Non-small cell lung cancer
- OS:
-
Overall survival
- PPV:
-
Positive predictive value
- pVPI:
-
Pathologic VPI
- VPI:
-
Visceral pleural invasion
References
Rami-Porta R, Bolejack V, Crowley J et al (2015) The IASLC lung cancer staging project: proposals for the revisions of the T descriptors in the forthcoming eighth edition of the TNM classification for lung cancer. J Thorac Oncol 10(7):990–1003
Eberhardt WE, Mitchell A, Crowley J et al (2015) The IASLC lung cancer staging project: proposals for the revision of the M descriptors in the forthcoming eighth edition of the TNM classification of lung cancer. J Thorac Oncol. 10(11):1515–1522
Qi M, Bian D, Zhang J, Zhu X, Zhou C, Zhang L (2021) The modification of T description according to visceral pleural invasion and tumor size from 3.1cm to 4.0cm in non-small cell lung cancer: a retrospective analysis based on the SEER database. Lung Cancer 158:47–54
Kim H, Goo JM, Kim YT, Park CM (2019) CT-defined visceral pleural invasion in T1 lung adenocarcinoma: lack of relationship to disease-free survival. Radiology 292(3):741–749
Choi H, Kim H, Hong W et al (2021) Prediction of visceral pleural invasion in lung cancer on CT: deep learning model achieves a radiologist-level performance with adaptive sensitivity and specificity to clinical needs. Eur Radiol 31(5):2866–2876
Ahn SY, Park CM, Jeon YK et al (2017) Predictive CT features of visceral pleural invasion by T1-sized peripheral pulmonary adenocarcinomas manifesting as subsolid nodules. AJR Am J Roentgenol 209(3):561–566
Hsu JS, Han IT, Tsai TH et al (2016) Pleural tags on CT scans to predict visceral pleural invasion of non-small cell lung cancer that does not abut the pleura. Radiology 279(2):590–596
Zhang Y, Kwon W, Lee HY et al (2021) Imaging assessment of visceral pleural surface invasion by lung cancer: comparison of CT and contrast-enhanced radial T1-weighted gradient echo 3-Tesla MRI. Korean J Radiol 22(5):829–839
Onoda H, Higashi M, Murakami T et al (2021) Correlation between pleural tags on CT and visceral pleural invasion of peripheral lung cancer that does not appear touching the pleural surface. Eur Radiol 31(12):9022–9029
Goldstraw P, Chansky K, Crowley J et al (2016) The IASLC lung cancer staging project: proposals for revision of the TNM stage groupings in the forthcoming (eighth) edition of the TNM classification for lung cancer. J Thorac Oncol 11(1):39–51
Lee KH, Lee JH, Park S et al (2023) Computed tomography-based prognostication in lung adenocarcinomas through histopathological feature learning: a retrospective multicenter study. Ann Am Thorac Soc 20(7):1020–1028
Hong S, Won YJ, Lee JJ et al (2018) Cancer statistics in Korea: incidence, mortality, survival, and prevalence in 2018. Cancer Res Treat 53(2):301–315
Travis WD, Brambilla E, Rami-Porta R et al (2008) Visceral pleural invasion: pathologic criteria and use of elastic stains: pathologic criteria and use of elastic stains: proposal for the 7th edition of the TNM classification for lung cancer. J Thorac Oncol. 3(12):1384–1390
Hillis SL (2007) A comparison of denominator degrees of freedom methods for multiple observer ROC analysis. Stat Med 26(3):596–619
Mandrekar JN (2010) Receiver operating characteristic curve in diagnostic test assessment. J Thorac Oncol 5(9):1315–1316
Landis JR, Koch GG (1977) The measurement of observer agreement for categorical data. Biometrics 33(1):159–174
Nakao K, Anraku M, Karasaki T et al (2019) Impact of previous malignancy on outcome in surgically resected non-small cell lung cancer. Ann Thorac Surg 108(6):1671–1677
Takamori S, Shimokawa M, Matsubara T et al (2021) Prognostic impact of smoking period in patients with surgically resected non-small cell lung cancer. Ann Surg Oncol 28(2):685–694
Cao J, Yuan P, Wang Y et al (2018) Survival rates after lobectomy, segmentectomy, and wedge resection for non-small cell lung cancer. Ann Thorac Surg 105(5):1483–1491
Xu J, Wang S, Zhong H et al (2019) Adjuvant chemotherapy improves survival in surgically resected stage IB squamous lung cancer. Ann Thorac Surg 107(6):1683–1689
McHugh ML (2012) Interrater reliability: the kappa statistic. Biochem Med (Zagreb) 22(3):276–282
Liang RB, Li P, Li BT et al (2021) Modification of pathologic T classification for non-small cell lung cancer with visceral pleural invasion: data from 1,055 cases of cancers ≤ 3 cm. Chest 160(2):754–764
Yip R, Ma T, Flores RM, Yankelevitz D, Henschke CI (2019) International Early Lung Cancer Action Program Investigators. Survival with parenchymal and pleural invasion of non-small cell lung cancers less than 30 mm. J Thorac Oncol 14(5):890–902
Fu F, Zhang Y, Wen Z et al (2019) Distinct prognostic factors in patients with stage I non-small cell lung cancer with radiologic part-solid or solid lesions. J Thorac Oncol 14(12):2133–2142
National Lung Screening Trial Research Team, Aberle DR, Adams AM et al (2011) Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med 365(5):395–409
de Koning HJ, van der Aalst CM, de Jong PA et al (2020) Reduced lung-cancer mortality with volume CT screening in a randomized trial. N Engl J Med 382(6):503–513
Vachani A, Carroll NM, Simoff MJ et al (2022) Stage migration and lung cancer incidence after initiation of low-dose CT screening. J Thorac Oncol 17(12):1355–1364
Chu ZG, Yang ZG, Shao H et al (2011) Small peripheral lung adenocarcinoma: CT and histopathologic characteristics and prognostic implications. Cancer Imaging 11(1):237–246
Nam JG, Park S, Park CM et al (2022) Histopathologic basis for a chest CT deep learning survival prediction model in patients with lung adenocarcinoma. Radiology 305(2):441–451
Shi J, Yang Y, Zhao Y, Zhu J, Song X, Jiang G (2019) EGFR mutations are significantly associated with visceral pleural invasion development in non-small-cell lung cancer patients. Cancer Manag Res 11:1945–1957
Chinchilla-Tabora LM, Sayagues JM, Gonzalez-Morais I, Rodriguez M, Ludena MD (2022) Prognostic impact of EGFR amplification and visceral pleural invasion in early stage pulmonary squamous cell carcinomas patients after surgical resection of primary tumor. Cancers (Basel) 14(9):2174
Funding
This study was supported by the Seoul National University Hospital Research Fund (grant numbers: 04–2020-2040 and 03–2022-2170) and by the Basic Science Research Program through the National Research Foundation of Korea (NRF), funded by the Ministry of Science and ICT (grant number: NRF-2020R1C1C1003684). However, the funders had no role in the study design; in the collection, analysis, and interpretation of the data; in the writing of the report; and in the decision to submit the article for publication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Pf. Hyungjin Kim.
Conflict of interest
Activities related to the present article: none.
Activities not related to the present article: J.M.G. received research grants from Dong Kook Lifescience, LG Electronics, and Coreline Soft. Y.T.K. received consulting fees from Johnson and Johnson and payment for lectures from AstraZeneca, and holds stock option in Genome Insight. H.K. received consulting fees from RadiSen, and holds stock and stock option in Medical IP.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was waived by the Institutional Review Board of Seoul National University Hospital and Seoul National University Bundang Hospital.
Ethical approval
Institutional Review Board approval was obtained.
Study subject or cohorts overlap
The study patients were reported previously in Lee et al. (2023), https://doi.org/10.1513/AnnalsATS.202210-895OC.
Methodology
-
Retrospective
-
Diagnostic and prognostic study
-
Performed at one institution
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lim, W.H., Lee, K.H., Lee, J.H. et al. Diagnostic performance and prognostic value of CT-defined visceral pleural invasion in early-stage lung adenocarcinomas. Eur Radiol 34, 1934–1945 (2024). https://doi.org/10.1007/s00330-023-10204-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-023-10204-2