Abstract
Objective
Although artificial intelligence (AI) has demonstrated promise in enhancing breast cancer diagnosis, the implementation of AI algorithms in clinical practice encounters various barriers. This scoping review aims to identify these barriers and facilitators to highlight key considerations for developing and implementing AI solutions in breast cancer imaging.
Method
A literature search was conducted from 2012 to 2022 in six databases (PubMed, Web of Science, CINHAL, Embase, IEEE, and ArXiv). The articles were included if some barriers and/or facilitators in the conception or implementation of AI in breast clinical imaging were described. We excluded research only focusing on performance, or with data not acquired in a clinical radiology setup and not involving real patients.
Results
A total of 107 articles were included. We identified six major barriers related to data (B1), black box and trust (B2), algorithms and conception (B3), evaluation and validation (B4), legal, ethical, and economic issues (B5), and education (B6), and five major facilitators covering data (F1), clinical impact (F2), algorithms and conception (F3), evaluation and validation (F4), and education (F5).
Conclusion
This scoping review highlighted the need to carefully design, deploy, and evaluate AI solutions in clinical practice, involving all stakeholders to yield improvement in healthcare.
Clinical relevance statement
The identification of barriers and facilitators with suggested solutions can guide and inform future research, and stakeholders to improve the design and implementation of AI for breast cancer detection in clinical practice.
Key Points
• Six major identified barriers were related to data; black-box and trust; algorithms and conception; evaluation and validation; legal, ethical, and economic issues; and education.
• Five major identified facilitators were related to data, clinical impact, algorithms and conception, evaluation and validation, and education.
• Coordinated implication of all stakeholders is required to improve breast cancer diagnosis with AI.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Although AI has demonstrated promise in enhancing breast cancer diagnosis, the implementation of AI algorithms in clinical practice encounters various barriers. This scoping review aims to identify these barriers and facilitators to highlight key considerations for developing and implementing AI solutions in breast cancer imaging. The first modality that incorporated AI techniques through traditional computer-aided detection (CAD) was mammography (MG) [1]. CAD was initially developed to assist radiologists in the detection of breast cancers they would have potentially missed without the help of CAD. However, a large study including more than 495,000 digital screening mammograms compared the performance of screening mammography with and without CAD by 271 radiologists, and it was demonstrated that screening performance was not improved with traditional CAD systems [2], and therefore there was no clinical benefit for patients. Over the last decade, advances in AI have encouraged the clinical study and implementation of AI-based CAD because it offers superior detection performance while not being reliant on hand-crafted imaging features [3]. Many studies demonstrated the good performance of AI in the detection of breast cancer using MG, ultrasound (US), or magnetic resonance imaging (MRI) — with similar performance to radiologists [4,5,6,7,8]. Furthermore, when AI is used by radiologists, there is less variability in radiologists’ interpretations, regardless of their experience, leading to a more reproducible and standardized diagnosis [4, 7]. Finally, AI is capable of processing and analyzing images faster than radiologists. This advantage is particularly pronounced when considering MRI, a multi-parametric modality, that comprises a lot of sequences, which considerably reduces reading time. In the case of screening programs with MG resulting in a large number of examinations, AI can be used for mammogram triage by automatically detecting normal exams, allowing radiologists to focus on other more complex exams [9]. The great need for data quality and quantity constitutes a disadvantage because if there is not enough data or using insufficient quality, AI models can be biased. The quantity of available data differs among modalities; digital breast tomosynthesis (DBT) and MG are typically favored because of their large accessibility [10]. Another disadvantage concerns the external validation of a model; most models are trained and developed from a single dataset and therefore cannot be applied easily to different populations or clinical settings [11]. AI can offer both advantages and disadvantages to breast imaging, and more precisely the barriers and facilitators of the implementation of such systems in clinical breast imaging settings have not been clearly stated. While previous scoping reviews have partially addressed barriers to implementing AI in breast cancer imaging [12, 13], they have not provided a comprehensive overview of these barriers. This study aims to fill this gap by identifying and categorizing the key barriers and facilitators to developing and implementing AI solutions for cancer detection in clinical breast imaging practice.
Method
Literature research was conducted in six databases (PubMed, Web of Science, CINHAL, Embase, IEEE, ArXiv) to get exhaustive results. The search was limited to 10 years (2012–2022) to target the recent advancement of AI in clinical breast imaging. Published articles of any design were eligible. We excluded conference abstracts, as they do not contain sufficient data for this review. Search strategy details were designed by M.P. and can be found in Supplement S1.
The selection of studies was done in two stages as depicted in the PRISMA [14] flow (Fig. 1), with the RAYYAN tool [15]. For the first stage, two reviewers (J.S., B.L.) independently screened the title and abstract of each article. Then in the second stage, the selected studies, as well as additional works found through screening the reference lists, were independently reviewed based on the inclusion criteria. When there were disagreements between the two reviewers, divergences were discussed and solved. There was no need for a third reviewer. Papers were included when there was mention of barriers and/or facilitators of AI for cancer detection in breast imaging. The following criteria led to the exclusion of papers:
-
Focus only on performance,
-
Use of synthetic datasets or data acquired with phantoms,
-
Not conventional clinical imaging of the breast (e.g., thermal imaging, microwave breast imaging),
-
Focus on histopathology images,
-
Conference abstract.
Papers that could not be found or were not available were also excluded. The final included studies were charted in a table containing structured information and characteristics of the studies (e.g., author, year of publication, geographical information, paper type, modality) (Supplement Table S4).
Results
Characteristics of the included publications
Of the 1476 screened publications, 107 were included (Fig. 1). Most papers originated from the USA (n = 37) and China (n = 17) (Fig. 2), and a large proportion (89.7%) were published after 2018 (Fig. 3). As depicted in Fig. 4, most articles focused on a single modality including MG (n = 39), US (n = 16), breast MRI (n = 6), and DBT (n = 2). In the “other” category, the studies were classified involving two or three modalities (n = 7) such as CT and US (n = 1), MG and DBT (n = 4), MRI and US (n = 1), and CT and MRI and US (n = 1). The “all” category referred to the inclusion of breast imaging as a whole, mentioning all the modalities in general (n = 37). Figure 5 shows that most of the articles were review articles (57%), and original research papers (34%). Scoping (n = 2) and systematic reviews (n = 2) (4%), as well as some opinion articles (n = 6, 5%), were included. Very few articles made their data (n = 6) or code (n = 8) publicly available or available under request to the authors. Details are provided in Supplement Table S4.
Main identified barriers and facilitators of AI in breast clinical imaging
Barriers and facilitators were identified through the first screening stage, and then clarified and enriched iteratively through complete text analysis of the included studies. Detailed tables can be found in Supplement Tables S2 and S3. Table 1 reports the main identified barriers and facilitators derived from included papers with relative frequency. We identified six major barriers involving data (B1), black box and trust (B2), algorithms and conception (B3), evaluation and validation (B4), legal, ethical, and economic issues (B5), and education (B6). We determined five major facilitators involving data (F1), clinical impact (F2), algorithms and conception (F3), evaluation and validation (F4), and education (F5). Figure 6 highlights that major barriers were reported twice as much as major facilitators. Sub-barriers and sub-facilitators were also derived as described in the following.
B1 Data
Data size and variety (B1.1)
The majority of publications (n = 60) reported the problem of small datasets for training and validation, as the size of the datasets was relatively small [16] to properly train AI algorithms. Different mentioned causes were limited data availability due to privacy concerns or technical constraints (e.g., collection of paired imaging data) [17, 18], insufficient data diversity (variety of population and imaging protocols, pathology nuances, etc.) often leading to overfitting, or data balancing issues (under/over-represented categories in the dataset, commonly observed in the medical field and that can affect prediction accuracy) [11, 16, 17, 19,20,21,22].
Data quality and data processing (B1.2)
Linked to data quantity, model performance depends on data quality affected by noisy or missing/incomplete data. This barrier was often mentioned (n = 48) as it requires appropriate data labelling supported by reliable annotation methods, which can be a very demanding process (need for trained staff to label or verify the data). This process was qualified as expensive, time-consuming, and subjective if not adequately performed [18, 19, 23,24,25,26,27,28].
Data sharing (B1.3)
The ability to share and pool data across actors (institutions, research teams, etc.) was reported as limited (n = 15). These limitations concern patient confidentiality, regulations, institutional policies, or different interests of stakeholders [10, 23, 29, 30].
B2 Black box and trust
Model transparency (B2.1)
The barrier of model transparency was often mentioned (n = 51). There is a need to develop transparent models able to explain what is predicted, how it has been done, and the degree of prediction confidence. Thus, it is important to have an interpretable AI system (the rationale followed by the system) to detect possible biases generated by the algorithms [11, 31, 32]. In the literature, the terms “transparency”, “explainability”, and “interpretability” are often used interchangeably, and there are no generally accepted definitions; therefore, all three terms were regrouped.
Clinician trust (B2.2)
Related to the interpretability problem, the adoption of an AI system depends on the level of confidence that the radiologists have in the AI system and its findings, and also on the understanding they have about the tool (n = 19) [24, 33, 34]. Avoiding dependence on AI systems to preserve users’ ability to think critically and make good patient decisions is also linked to radiologists’ trust [35, 36].
Patient trust (B2.3)
Patient confidence (n = 11) in the AI systems was also reported as important in the same way as for radiologists, and is also linked to communication between human and machine when the diagnosis is disclosed [3, 37].
B3 Algorithm and conception
Model architecture (B3.1)
A large variety of AI algorithmic models exists, along with multiple ways for parameterizing, training, validating, and testing these models. This contributes to the difficulty of choosing and tuning the right architecture for a given purpose, as well as devising objective ways to compare results between models (n = 16) [20, 26, 38].
Technical constraints (B3.2)
Model architectures may impose some constraints (n = 17) on the input data (data dimensionality, resolution, layout, etc.) leading to data transformation (e.g., data dimensionality reduction) [10]. Similarly, hardware constraints (storage, memory, computing capabilities, etc.) may limit the choice of usable models or further contribute to data transformation [26, 38,39,40,41]. Finally, difficulties related to the integration of AI tools in clinical practice (e.g., compatibility with PACS and RIS systems, characteristics of the imaging modalities) are part of these technical constraints [33, 42, 43].
Multi-variable data (B3.3)
The development of efficient algorithms is more challenging due to the complex nature of multi-variable data essential for clinical reasoning. This data includes multi-modality imaging, multi-parametric protocols, clinical knowledge, and previous or contralateral examinations (n = 28) [29, 44].
Involvement of stakeholders (B3.4)
There is a need for a closer collaboration (n = 29) between all stakeholders (clinicians, data scientists, researchers, industry, policymakers, patients, etc.) in the design and development of AI systems [1, 19, 33, 45], sharing of development tools and procedures, as well as in the definition of common definitions and metrics for evaluation and model comparison [18, 27, 28].
B4 Evaluation and validation
Meaningful clinical validation (B4.1)
Assessments of clinical utility, performance, and adoption are of paramount importance and were thus often mentioned in the studies (n = 44). Prospective studies are required to evaluate performance and the effect on clinicians in clinical settings, distinguishing engineering metrics from clinical ones [11], as well as the type of clinical scenarios (e.g., screening vs. follow-ups). Large trials should be conducted, possibly over long periods, and the use of independent test datasets was promoted [1, 3, 19, 28].
Data variability (B4.2)
In real-world clinical practice, there is inherent data variability depending on e.g. manufacturers, equipment age and characteristics, imaging protocols, and population traits that must be taken into account to assess the generalization of the deployed AI systems (n = 54) [10, 19, 27].
Quality assurance (QA) (B4.3)
Continuous monitoring of AI algorithms was recommended (n = 17) for continuous improvements or to prevent performance degradation over time due to changes, requiring to put in place QA procedures with adequate resources [40, 43, 46].
B5 Legal, ethical, and economic issues
Liability (B5.1)
Many open questions are raised concerning the final responsibility in the decisions made for patient care (n = 22) (e.g., Can final decisions be made by the AI systems? Who will be responsible for errors? Will AI negatively influence radiologists?), and thus these questions need to be addressed [11, 42].
Law and policies (B5.2)
This barrier (n = 24) highlighted concerns about the importance of patient-privacy policies, market approval or clearance of AI solutions, intellectual properties (e.g., who owns the data?), and regulatory guidelines [11, 19, 33].
Fair AI (B5.3)
There are many ways to unintentionally introduce biases in AI systems (e.g., in data collection or development stages) and it is crucial to embrace fair AI practices promoting equity in diagnosis and treatment across diverse populations without excluding minorities (n = 22) [21, 28, 30].
Cybersecurity (B5.4)
Few studies reported concerns about cybersecurity (n = 10). Healthcare data being very sensitive, the importance of addressing security risks, preventing imaging data sabotage/manipulation (e.g., adversarial attacks by inserting or removing pathologies), and ensuring data protection and privacy were reported [3, 19].
Economic issues (B5.5)
Economic barriers were mentioned in some papers (n = 11), due to different interests among stakeholders (e.g., company vs. researchers), reimbursement policies (e.g., CAD is reimbursed in the USA but not in EU for most cases, with the potential exception of screening) [47], increased health costs due to unnecessary actions (non-relevant findings leading to overdiagnosis or overtreatment) [48], costs of collecting and processing data, especially from expensive/less common modalities such as MRI, and the costs of running and maintaining AI systems [23, 33, 45].
B6 Education
User education (B6.1)
Few papers (n = 5) reported that users (radiologists, patients, health professionals, etc.) must have sufficient knowledge about AI data (collection, annotation, etc.) and AI tools (terminologies and concepts, methods, and applications, etc.) to critically evaluate them, and be aware of their strengths and limitations [9, 11, 33, 35].
F1 Data
Datasets initiatives (F1.1)
There exist initiatives from multiple public and private sector institutions to create large, diversified, annotated datasets, to be made available to public databases, challenges, etc. (n = 15) [19, 23, 32, 39, 49].
Algorithmic approaches to address data barriers (F1.2)
Some solutions were mentioned or utilized to try to address the issues of lack of or non-shareable data (n = 27) [28], such as federated learning (data remains locally but algorithm parameters travel [10, 19]), swarm learning [10], transfer learning [16, 26], data augmentation [49], data normalization [10], and generative models [39].
F2 Clinical impact
Diagnostic performance (F2.1)
A model/AI system’s performance is evaluated using a test set. In the different studies, the metrics usually used are area under the ROC curve (AUC), or sensitivity and specificity, with or without comparison to the radiologist or in combination with the radiologist. Generally, good diagnostic performance was reported in surveyed reviews and original research works (n = 53) [5, 8, 50, 51].
Clinical workflow (F2.2)
A lot of papers (n = 58) reported that AI systems positively impacted clinical workflow by improving efficiency in clinical practice, such as triaging, using AI as proof reader, reading time reduction, improved communication with patients, reduction of radiologist fatigue, cost reduction, or more reproducible readings [9, 11, 12, 52, 53].
F3 Algorithms and conception
Multi-variable data (F3.1)
Some papers (n = 24) argued that multi-variable data (e.g., multi-modality imaging, multi-parametric protocols, or inclusion of clinical non-imaging information) could lead to better results for AI tools because each source of data provides valuable information and machine learning (ML) offers approaches to embrace multi-dimensional data [10, 13, 37, 54].
Numerous algorithms (F3.2)
It was also reported that the large number of algorithms developed provides greater flexibility for AI integration (n = 11). The use of ensemble models combining the predictions of several algorithms has also been reported as a way to increase performance [21, 32, 55, 56].
F4 Evaluation and validation
Increased accessibility of AI (F4.1)
There is an increasing number of (certified) AI products that are made available in clinical practice, facilitating the setup of clinical trials and prospective studies (n = 3) [19, 34, 37].
Benchmarking of AI approaches (F4.2)
There were mentioned (n = 6) international scientific challenges that contribute to strengthening the benchmarking of AI approaches by providing open and reproducible evaluation (training and testing data, evaluation metrics, and tools) that strongly encourages or imposes the sharing of computer code from participants [47, 57].
F5 Education
AI for education (F5.1)
Few papers (n = 5) highlighted that some systems or models can be used for the education of clinicians, such as generative models producing images for the training of radiologists [39, 50] or systems giving feedback to radiographers for image quality or acquisition parameters [48].
Discussion
This scoping review provides a comprehensive summary of the barriers and facilitators encountered during the creation and deployment of AI in clinical settings. Solutions can then be found and measures can be taken for better implementation of AI systems in practice — bringing tangible benefits to both patients and clinicians.
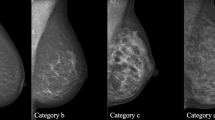
Conception
The importance of data size (B1.1) and data quality (B1.2) was predominant in the included studies, being directly related to the effectiveness of machine learning and the issue of data sharing (e.g., less than 17% of original papers’ data is publicly available or under request as shown in Supplement Table S4). As a result of screening programs and higher availability, it was highlighted that digital MG and DBT studies usually have large datasets (many thousands of patients, from 9919 to 32,714 women in studies with MG [58] and DBT [51]) often acquired in several centers, in comparison to studies involving US and MRI [1, 10]. MRI studies especially lacked data (from 93 [59] to 1715 patients [25] in included studies, with varying types of MR protocols). While US imaging may benefit from larger accessibility, an important discrepancy was observed among studies where the number of patients ranged from 92 to 5151 [54, 60,61,62,63,64,65,66,67]. Variety in the data was also reported as a critical issue since clinical data is often imbalanced due to disease prevalence, data availability, or population characteristics, which remains an unsolved issue still under research in the ML field [16]. In practice, data curation is a difficult and tedious task, especially depending on the type of collected data or modality of imaging. Collection without interfering with the clinical practice workflow, anonymization process, ethics commission requirements, and compliant and robust databases are among the many hurdles faced during this process. Despite being expensive and time-consuming, data curation with clinical expert validation remains an absolute necessity [68].
To address these challenges, some solutions can be considered, like large datasets initiatives (F1.1) (e.g., result of competitions opened to the research community [57, 69]), more adapted algorithmic approaches (F1.2), or the promotion of data sharing and collaboration between clinical settings by supporting regulations on patient confidentiality in favor to research (such as the generalized patient consent). These actions can contribute to having larger but also more representative and diversified datasets.
To support data annotation, one suggestion would be to rely more on automated systems compliant with regulations and ease the work of clinical annotators. For instance, pathological findings reported in radiological reports could be associated with their exact localization in the images via user-friendly reporting tools, simplifying the data annotation and expediting its processing. In the context of creating a data challenge on US breast lesions, Lassau et al [57] observed the added value of relying on professional tools to anonymize and gather annotated data from eleven clinical centers in a centralized and an automatic way, in accordance with regulations such as GDPR. Involving and training healthcare professionals with experience in medical imaging, such as radiographers in the collection and annotation of imaging data, can be another solution to address the time-consuming data preparation and processing usually performed by radiologists.
The large variety of identified model architectures involving multiple parameters can be a double-edged sword at the conception stage. On the one hand, this allows more flexibility in the design and contributes to reinforcing some models (F3.2). On the other hand, this can also result in empirical model selection and parameter setting (B3.1) in the presence of ubiquitous technical and data constraints (B3.2 and B3.3). This contributes to the difficulty to choose the right model for the clinical target problem — fostering the need to gather all stakeholders (B3.4) to define common guidelines for the design and comparison of AI models [70]. Fortunately, the availability of code will continue to increase (~ 30% is publicly available or under request, Supplement Table S4) — supporting the reproducibility and transparency of published works.
Clinical implementation
Despite several studies highlighting the potential of AI systems in terms of diagnostic performance (F2.1) and clinical workflow improvement (F2.2), only a few are properly implemented and used in clinical practice. In two recent systematic reviews on the use of AI in breast cancer screening programs, no prospective study for test accuracy was found [71]. This is a crucial point (B4.1) as a prospective study design is crucial to assess real clinical impact. Multi-center studies are also very important to assess the generalizability of developed AI systems, with different devices, acquisition protocols, and populations [3]. If data can be shared across institutions, validation on other data and imaging devices can be facilitated, and continuous update and quality control on AI systems would be possible.
Among the included studies, model transparency (B2.1) was an often-reported barrier. The black-box nature of modern AI algorithms is a major barrier to clinical implementation due to limited explanations for decisions, and the possible presence of bias — eroding the trust of clinicians and patients. Many methods to explain decisions of AI models are being investigated by the ML community, but these should be validated in clinical practice with end-users [72, 73]. Moving forward, it is imperative that future research focuses on the systematic development of more transparent AI algorithms using or creating explainability methods. Furthermore, these methods need to be evaluated to prevent potential biases.
These ethical aspects are closely related to legal concerns that are rising with the development of AI. At present, there are no international laws or consensus on the guidelines for the regulation of AI in medicine. However, many international supportive actions (e.g., WHO [74] and OCDE [75]) and national initiatives are being developed (e.g., USA FDA’s Software as Medical Device Action Plan [11] or EU’s “right to explanation” for patients [76]). Nevertheless, we strongly believe that achieving an international consensus for AI regulation is imperative, as opposed to relying solely on regional or national initiatives.
Specificities of breast imaging modalities
Identified barriers and facilitators were globally encountered in each modality of clinical breast imaging (MG, DBT, US, or MRI); nevertheless, nuances related to the specificities of each modality were also identified. Compared to other modalities, US is more strongly operator-dependent due to the operator’s level of expertise, image quality appreciation, variability of acquisition (e.g., probe positioning, tissue compression, use of other imaging techniques like Doppler or elastography), and device parameters. This variability hinders the training and application of models [77,78,79]. In addition, careful attention is required when using common augmentation techniques as they may alter typical patterns of breast lesions (e.g., the presence of posterior acoustic shadow) [79]. Finally, embedded AI systems are often desired for real-time US investigation, introducing significant technical constraints given their low computing capabilities [54].
Even if AI methods developed for MG can be applied to DBT with transfer learning [80], DBT still presents some particularities related to the acquisition at multiple angles allowing the assessment of different depths of the breast [80]. This process is not standardized among clinical sites (number of images and angular range), enforcing the need for multi-center and multivendor studies [81].
Breast MRI generates a large amount of data, mainly due to the multi-parametric nature of this modality (multiple types of sequences), involving high dimensional data, e.g., DCE-MRI (dynamic contrast-enhanced MRI), 4D ultrafast sequences (series of 3D images over time with a high temporal resolution allowing visualization of contrast media uptake within 1 min), and diffusion sequences. The resulting series of 3D and 4D data are difficult to handle due to technical constraints (memory and computing resources), and the absence of off-the-shelf ML architectures to efficiently support and process the data (especially for 4D data). This often results in data transformation (such as dimensionality reduction) with the risk of losing information [10].
Methodological choices with limitations and perspectives
Despite AI performance indicators being predominantly present in the surveyed literature, we purposely chose to not focus on performance metrics in the context of a scoping review. However, the dimension of performance was considered in the facilitators when a positive clinical impact was reported, since a well-performing AI solution will more likely be implemented or accepted in clinical practice.
In addition to works that explicitly mentioned barriers and/or facilitators of AI in breast imaging diagnosis, we decided to also include some papers that indirectly refer to barriers or facilitators based on the study design or author comments. Similarly, we included some publications not exclusively focusing on breast cancer as they were relevant in the context of breast cancer imaging and because they enriched the analysis of identified barriers and facilitators. The decision to include reviews, opinion articles, and original research also contributed to a more exhaustive scoping of the literature.
Most of the included papers originated from the USA, China, South Korea, India, and European countries (Fig. 2); thus, the results of this scoping review cannot reflect all the specificities of countries across the globe. For instance, depending on the difficulties of access or socio-economic constraints of some countries, some barriers may become more important [82] but facilitators may also appear, such as a greater demand for AI to counter a shortage of qualified professionals. This could pave the way for future work focusing on geographic, cultural, and socio-economic issues and potential discrepancies that could be related to AI introduction in breast cancer care.
Authors’ opinion
There is still work to be done before AI systems are implemented sustainably in clinical practice. Regarding research, we believe it is important to promote transparency and reproducibility. Furthermore, it is important to acknowledge that AI models are susceptible to biases, particularly in cases where data are imbalanced or certain segments of the population are under-represented. To address this concern, it is recommended in the literature that research systematically includes demographic data (such as age, sex, ethnicity) and provides a comprehensive description of the measures taken to ensure data quality [68, 83]. This approach allows for the evaluation of biases within the models.
In practice, it appears urgent to establish methods for data collection and processing through the development of automated tools and active involvement of all health professionals engaged in breast imaging including radiographers, radiologists, and medical physicists. For instance, radiographers could assume a more significant role [19] in tasks such as data collection, data processing, protocol optimization, evaluation, clinical integration, and quality control for AI development and maintenance [84,85,86]. Another critical aspect to emphasize is that trust, from health professionals, patients, and also society in general, can impact the integration and adoption of AI in clinical settings. To address this barrier, it is crucial to focus on transparent AI algorithms with robust explainability methods and user-friendly AI interface systems during the conception stage. Additionally, more attention should be paid to the education of health professionals and patients about AI. This scoping review revealed a persistent lack of education among healthcare professionals, with insufficient integration of AI into their curricula despite recommendations [11, 87]. The acceptance of AI by patients is also a determining factor, with studies indicating that patient utilization of AI is more acceptable when under the continuous supervision of a physician [88]. This is understandable since physicians consider the patient’s complete medical history, while AI systems often focus solely on the imaging modality for which they are designed. Patients also harbor concerns regarding AI, such as preserving choice and autonomy, ensuring AI safety, and managing costs [89]. It is essential to address these concerns by implementing practices such as obtaining informed consent, establishing robust data privacy security measures, and ensuring that AI services are covered by health insurance. In conclusion, we strongly recommend the inclusion of AI training in professional education programs, accompanied by continuous training to keep up with the rapidly evolving techniques. Moreover, patients should be actively involved by receiving adequate information and being given the opportunity to participate in decisions regarding their care management and treatment. All stakeholders, including patients and healthcare professionals, should be actively engaged in the development of AI in healthcare.
Conclusion
By identifying barriers and facilitators along with suggested solutions, this scoping review can provide valuable guidance to inform future research endeavors and support stakeholders in enhancing the design and implementation of AI for breast cancer detection in clinical practice. It highlighted the need to carefully conceive, deploy, and evaluate AI solutions in practice. Fortunately, most identified barriers had corresponding facilitators — showing that solutions are being explored to mitigate the current issues faced by clinical AI. There is little doubt that AI can improve breast cancer imaging, but a lot of coordinated effort among stakeholders will be required. In particular, health professionals involved in the production and consumption of medical images should be trained in AI principles and closely interact with AI systems.
Abbreviations
- AI:
-
Artificial intelligence
- AUC:
-
Area under the curve
- CAD:
-
Computer-aided diagnosis/detection
- CINHAL:
-
Cumulative Index to Nursing and Allied Health Literature
- CT:
-
Computed tomography
- DBT:
-
Digital breast tomosynthesis
- DCE:
-
Dynamic contrast-enhanced
- FDA:
-
Food and Drug Administration
- GDPR:
-
General Data Protection Regulation
- IEEE:
-
Institute of Electrical and Electronics Engineers
- MG:
-
Digital mammography
- ML:
-
Machine learning
- MRI:
-
Magnetic resonance imaging
- PACS:
-
Picture Archiving and Communication System
- PRISMA:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- QA:
-
Quality assurance
- RIS:
-
Radiology information systems
- US:
-
Ultrasound
References
Bitencourt A, Naranjo I, Lo Gullo R, Saccarelli C, Pinker K (2021) AI-enhanced breast imaging: where are we and where are we heading? Eur J Radiol. https://doi.org/10.1016/j.ejrad.2021.109882
Lehman CD, Wellman RD, Buist DSM, Kerlikowske K, Tosteson ANA, Miglioretti DL (2015) Diagnostic accuracy of digital screening mammography with and without computer-aided detection. JAMA Intern Med. https://doi.org/10.1001/jamainternmed.2015.5231
Ou WC, Polat D, Dogan BE (2021) Deep learning in breast radiology: current progress and future directions. Eur Radiol. https://doi.org/10.1007/s00330-020-07640-9
Pacilè S, Lopez J, Chone P, Bertinotti T, Grouin JM, Fillard P (2020) Improving breast cancer detection accuracy of mammography with the concurrent use of an artificial intelligence tool. Radiol Artif Intell 2:e190208. https://doi.org/10.1148/ryai.2020190208
Rodríguez-Ruiz A, Krupinski E, Mordang J-J et al (2019) Detection of breast cancer with mammography: effect of an artificial intelligence support system. Radiology. https://doi.org/10.1148/radiol.2018181371
O’Connell AM, Bartolotta TV, Orlando A, Jung S, Baek J, Parker KJ (2022) Diagnostic performance of an artificial intelligence system in breast ultrasound. J Ultrasound Med. https://doi.org/10.1002/jum.15684
Adachi M, Fujioka T, Mori M et al (2020) Detection and diagnosis of breast cancer using artificial intelligence based assessment of maximum intensity projection dynamic contrast-enhanced magnetic resonance images. Diagnostics. https://doi.org/10.3390/diagnostics10050330
Rodriguez-Ruiz A, Lång K, Gubern-Merida A et al (2019) Stand-alone artificial intelligence for breast cancer detection in mammography: comparison with 101 radiologists. J Natl Cancer Inst. https://doi.org/10.1093/jnci/djy222
Tagliafico AS, Piana M, Schenone D, Lai R, Massone AM, Houssami N (2019) Overview of radiomics in breast cancer diagnosis and prognostication. Breast 49:74–80. https://doi.org/10.1016/j.breast.2019.10.018
Balkenende L, Teuwen J, Mann RM (2022) Application of deep learning in breast cancer imaging. Semin Nucl Med. https://doi.org/10.1053/j.semnuclmed.2022.02.003
Vobugari N, Raja V, Sethi U, Gandhi K, Raja K, Surani SR (2022) Advancements in oncology with artificial intelligence—a review article. Cancers. https://doi.org/10.3390/cancers14051349
Masud R, Al-Rei M, Lokker C (2019) Computer-aided detection for breast cancer screening in clinical settings: scoping review. JMIR Med Inform. https://doi.org/10.2196/12660
Houssami N, Kirkpatrick-Jones G, Noguchi N, Lee CI (2019) Artificial intelligence (AI) for the early detection of breast cancer: a scoping review to assess AI’s potential in breast screening practice. Expert Rev Med Devices. https://doi.org/10.1080/17434440.2019.1610387
Tricco AC, Lillie E, Zarin W et al (2018) PRISMA Extension for Scoping Reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. https://doi.org/10.7326/M18-0850
Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A (2016) Rayyan—a web and mobile app for systematic reviews. Syst Rev. https://doi.org/10.1186/s13643-016-0384-4
Zhang Z, Sejdić E (2019) Radiological images and machine learning: trends, perspectives, and prospects. Comput Biol Med. https://doi.org/10.1016/j.compbiomed.2019.02.017
Trivizakis E, Papadakis GZ, Souglakos I et al (2020) Artificial intelligence radiogenomics for advancing precision and effectiveness in oncologic care (Review). Int J Oncol. https://doi.org/10.3892/ijo.2020.5063
Pang T, Wong J, Ng W, Chan C (2020) Deep learning radiomics in breast cancer with different modalities: overview and future. Expert Syst Appl. https://doi.org/10.1016/j.eswa.2020.113501
Wichmann JL, Willemink MJ, De Cecco CN (2020) Artificial intelligence and machine learning in radiology: current state and considerations for routine clinical implementation. Invest Radiol. https://doi.org/10.1097/RLI.0000000000000673
Deshmukh PB, Kashyap KL (2021) Research challenges in breast cancer classification through medical imaging modalities using machine learning. In: 2021 International Conference on Industrial Electronics Research and Applications (ICIERA). IEEE, New Delhi, India, pp 1–5. https://doi.org/10.1109/ICIERA53202.2021.9726746
Cuocolo R, Caruso M, Perillo T, Ugga L, Petretta M (2020) Machine learning in oncology: a clinical appraisal. Cancer Lett. https://doi.org/10.1016/j.canlet.2020.03.032
Chaudhary V, Chaudhari S (2021) Application of machine learning in breast cancer diagnosis: a review. In: 2021 IEEE Bombay Section Signature Conference (IBSSC). pp 1–6. https://doi.org/10.1109/IBSSC53889.2021.9673373
Gardezi SJS, Elazab A, Lei B, Wang T (2019) Breast cancer detection and diagnosis using mammographic data: systematic review. J Med Internet Res. https://doi.org/10.2196/14464
Bahl M (2020) Artificial intelligence: a primer for breast imaging radiologists. J Breast Imaging. https://doi.org/10.1093/jbi/wbaa033
Meyer-Bäse A, Morra L, Meyer-Bäse U, Pinker K (2020) Current status and future perspectives of artificial intelligence in magnetic resonance breast imaging. Contrast Media Mol Imaging. https://doi.org/10.1155/2020/6805710
Wang Z, Luo Y, Xin J et al (2020) Computer-aided diagnosis based on extreme learning machine: a review. IEEE Access. https://doi.org/10.1109/ACCESS.2020.3012093
Bai J, Posner R, Wang T, Yang C, Nabavi S (2021) Applying deep learning in digital breast tomosynthesis for automatic breast cancer detection: a review. Med Image Anal. https://doi.org/10.1016/j.media.2021.102049
Bi WL, Hosny A, Schabath MB et al (2019) Artificial intelligence in cancer imaging: clinical challenges and applications. CA Cancer J Clin. https://doi.org/10.3322/caac.21552
Panayides A, Amini A, Filipovic N et al (2020) AI in medical imaging informatics: current challenges and future directions. IEEE J Biomed Health Inform. https://doi.org/10.1109/JBHI.2020.2991043
Halim A, Andrew A, Yasin M et al (2021) Existing and emerging breast cancer detection technologies and its challenges: a review. Appl Sci. https://doi.org/10.3390/app112210753
Zhang X, Zhang Y, Zhang G et al (2022) Deep learning with radiomics for disease diagnosis and treatment: challenges and potential. Front Oncol. https://doi.org/10.3389/fonc.2022.773840
Sahiner B, Pezeshk A, Hadjiiski L et al (2019) Deep learning in medical imaging and radiation therapy. Med Phys. https://doi.org/10.1002/mp.13264
Tadavarthi Y, Vey B, Krupinski E et al (2020) The state of radiology AI: considerations for purchase decisions and current market offerings. Radiol Artif Intell 2(6):e200004. https://doi.org/10.1148/ryai.2020200004
Komatsu M, Sakai A, Dozen A et al (2021) Towards clinical application of artificial intelligence in ultrasound imaging. Biomedicines. https://doi.org/10.3390/biomedicines9070720
Le EPV, Wang Y, Huang Y, Hickman S, Gilbert FJ (2019) Artificial intelligence in breast imaging. Clin Radiol. https://doi.org/10.1016/j.crad.2019.02.006
Johansson G, Olsson C, Smith F, Edegran M, Björk-Eriksson T (2021) AI-aided detection of malignant lesions in mammography screening - evaluation of a program in clinical practice. BJR Open 3:20200063
Grimm L (2021) Radiomics: a primer for breast radiologists. J Breast Imaging. https://doi.org/10.1093/jbi/wbab014
Batchu S, Liu F, Amireh A, Waller J, Umair M (2021) A review of applications of machine learning in mammography and future challenges. Oncology. https://doi.org/10.1159/000515698
Harvey H, Karpati E, Khara G et al (2019) The role of deep learning in breast screening. Curr Breast Cancer Rep. https://doi.org/10.1007/s12609-019-0301-7
Li H, Ye J, Liu H et al (2021) Application of deep learning in the detection of breast lesions with four different breast densities. Cancer Med. https://doi.org/10.1002/cam4.4042
Maqsood S, Damasevicius R, Maskeliunas R (2022) TTCNN: a breast cancer detection and classification towards computer-aided diagnosis using digital mammography in early stages. Appl Sci. https://doi.org/10.3390/app12073273
European Society of Radiology (2019) What the radiologist should know about artificial intelligence - an ESR white paper. Insights Imaging 10(1):44. https://doi.org/10.1186/s13244-019-0738-2
Choy G, Khalilzadeh O, Michalski M et al (2018) Current applications and future impact of machine learning in radiology. Radiology. https://doi.org/10.1148/radiol.2018171820
Fujioka T, Mori M, Kubota K et al (2020) The utility of deep learning in breast ultrasonic imaging: a review. Diagnostics 10:1055
Lamb LR, Lehman CD, Gastounioti A, Conant EF, Bahl M (2022) Artificial intelligence (AI) for screening mammography, from the AJR special series on AI applications. AJR Am J Roentgenol. https://doi.org/10.2214/AJR.21.27071
Lee CI, Houssami N, Elmore JG, Buist DSM (2020) Pathways to breast cancer screening artificial intelligence algorithm validation. Breast. https://doi.org/10.1016/j.breast.2019.09.005
Bennani-Baiti B, Baltzer PAT (2020) Künstliche Intelligenz in der Mammadiagnostik. Radiologe. https://doi.org/10.1007/s00117-019-00615-y
Thomassin-Naggara I, Balleyguier C, Ceugnart L et al (2019) Artificial intelligence and breast screening: French Radiology Community position paper. Diagn Interv Imaging. https://doi.org/10.1016/j.diii.2019.08.005
Gao Y, Geras KJ, Lewin AA, Moy L (2019) New frontiers: an update on computer-aided diagnosis for breast imaging in the age of artificial intelligence. AJR Am J Roentgenol. https://doi.org/10.2214/AJR.18.20392
Huang S, Yang J, Fong S, Zhao Q (2020) Artificial intelligence in cancer diagnosis and prognosis: opportunities and challenges. Cancer Lett. https://doi.org/10.1016/j.canlet.2019.12.007
Shoshan Y, Bakalo R, Gilboa-Solomon F et al (2022) Artificial intelligence for reducing workload in breast cancer screening with digital breast tomosynthesis. Radiology. https://doi.org/10.1148/radiol.211105
Lei Y-M, Yin M, Yu M-H et al (2021) Artificial intelligence in medical imaging of the breast. Front Oncol. https://doi.org/10.3389/fonc.2021.600557
Song L, Hsu W, Xu J, van der Schaar M (2016) Using contextual learning to improve diagnostic accuracy: application in breast cancer screening. IEEE J Biomed Health Inform. https://doi.org/10.1109/JBHI.2015.2414934
Dai J, Lei S, Dong L et al (2021) More reliable AI solution: breast ultrasound diagnosis using multi-AI combination. arXiv preprint arXiv:210102639 [cs]
Ayer T, Chen Q, Burnside ES (2013) Artificial neural networks in mammography interpretation and diagnostic decision making. Comput Math Methods Med. https://doi.org/10.1155/2013/832509
Satake H, Ishigaki S, Ito R, Naganawa S (2022) Radiomics in breast MRI: current progress toward clinical application in the era of artificial intelligence. Radiol Med (Torino). https://doi.org/10.1007/s11547-021-01423-y
Lassau N, Bousaid I, Chouzenoux E et al (2021) Three artificial intelligence data challenges based on CT and ultrasound. Diagn Interv Imaging. https://doi.org/10.1016/j.diii.2021.06.005
Chang Y-W, An JK, Choi N et al (2022) Artificial intelligence for breast cancer screening in mammography (AI-STREAM): a prospective multicenter study design in Korea using AI-based CADe/x. J Breast Cancer. https://doi.org/10.4048/jbc.2022.25.e4
Daimiel Naranjo I, Gibbs P, Reiner JS et al (2022) Breast lesion classification with multiparametric breast MRI using radiomics and machine learning: a comparison with radiologists’ performance. Cancers. https://doi.org/10.3390/cancers14071743
Qian X, Pei J, Zheng H et al (2021) Prospective assessment of breast cancer risk from multimodal multiview ultrasound images via clinically applicable deep learning. Nat Biomed Eng. https://doi.org/10.1038/s41551-021-00711-2
Han S, Kang HK, Jeong JY et al (2017) A deep learning framework for supporting the classification of breast lesions in ultrasound images. Phys Med Biol. https://doi.org/10.1088/1361-6560/aa82ec
Ciritsis A, Rossi C, Eberhard M, Marcon M, Becker AS, Boss A (2019) Automatic classification of ultrasound breast lesions using a deep convolutional neural network mimicking human decision-making. Eur Radiol. https://doi.org/10.1007/s00330-019-06118-7
Du R, Chen Y, Li T, Shi L, Fei Z, Li Y (2022) Discrimination of breast cancer based on ultrasound images and convolutional neural network. J Oncol 2022:7733583
Heller SL, Wegener M, Babb JS, Gao Y (2021) Can an artificial intelligence decision aid decrease false-positive breast biopsies? Ultrasound Q. https://doi.org/10.1097/RUQ.0000000000000550
Kim Y, Kang BJ, Lee JM, Kim SH (2019) Comparison of the diagnostic performance of breast ultrasound and CAD using BI-RADS descriptors and quantitative variables. Iran J Radiol. https://doi.org/10.5812/iranjradiol.67729
Lyu SY, Zhang Y, Zhang MW et al (2022) Diagnostic value of artificial intelligence automatic detection systems for breast BI-RADS 4 nodules. World J Clin Cases. https://doi.org/10.12998/wjcc.v10.i2.518
Yu T-F, He W, Gan C-G et al (2021) Deep learning applied to two-dimensional color Doppler flow imaging ultrasound images significantly improves diagnostic performance in the classification of breast masses: a multicenter study. Chin Med J. https://doi.org/10.1097/CM9.0000000000001329
Mincu D, Roy S (2022) Developing robust benchmarks for driving forward AI innovation in healthcare. Nat Mach Intell. https://doi.org/10.1038/s42256-022-00559-4
Schaffter T, Buist DSM, Lee CI et al (2020) Evaluation of combined artificial intelligence and radiologist assessment to interpret screening mammograms. JAMA Netw Open. https://doi.org/10.1001/jamanetworkopen.2020.0265
Ibrahim H, Liu X, Denniston AK (2021) Reporting guidelines for artificial intelligence in healthcare research. Clin Experiment Ophthalmol. https://doi.org/10.1111/ceo.13943
Freeman K, Geppert J, Stinton C et al (2021) Use of artificial intelligence for image analysis in breast cancer screening programmes: systematic review of test accuracy. BMJ (Clin Res Ed). https://doi.org/10.1136/bmj.n1872
Singh BK, Jain P, Banchhor SK, Verma K (2019) Performance evaluation of breast lesion detection systems with expert delineations: a comparative investigation on mammographic images. Multimed Tools Appl. https://doi.org/10.1007/s11042-019-7570-z
Gulum MA, Trombley CM, Kantardzic M (2021) A review of explainable deep learning cancer detection models in medical imaging. Appl Sci. https://doi.org/10.3390/app11104573
World Health Organization (2021) Ethics and governance of artificial intelligence for health: WHO guidance. World Health Organization, Geneva
Vincent-Lancrin S, van der Vlies R (2020) Trustworthy artificial intelligence (AI) in education: Promises and challenges. OECD Education Working Papers Series, OECD, n° 218. https://doi.org/10.1787/a6c90fa9-en
Goodman B, Flaxman S (2017) European Union regulations on algorithmic decision-making and a “right to explanation.” AI Magazine. https://doi.org/10.1609/aimag.v38i3.2741
Zhang D, Jiang F, Yin R et al (2021) A review of the role of the S-Detect computer-aided diagnostic ultrasound system in the evaluation of benign and malignant breast and thyroid masses. Med Sci Monit 27:e931957. https://doi.org/10.12659/MSM.931957
Shen Y-T, Chen L, Yue W-W, Xu H-X (2021) Artificial intelligence in ultrasound. Eur J Radiol. https://doi.org/10.1016/j.ejrad.2021.109717
Kim J, Kim HJ, Kim C, Kim WH (2021) Artificial intelligence in breast ultrasonography. Ultrasonography. https://doi.org/10.14366/usg.20117
Sechopoulos I, Teuwen J, Mann R (2021) Artificial intelligence for breast cancer detection in mammography and digital breast tomosynthesis: state of the art. Semin Cancer Biol. https://doi.org/10.1016/j.semcancer.2020.06.002
Geras KJ, Mann RM, Moy L (2019) Artificial intelligence for mammography and digital breast tomosynthesis: current concepts and future perspectives. Radiology. https://doi.org/10.1148/radiol.2019182627
Juhn YJ, Ryu E, Wi C-I et al (2022) Assessing socioeconomic bias in machine learning algorithms in health care: a case study of the HOUSES index. J Am Med Inform Assoc. https://doi.org/10.1093/jamia/ocac052
Garin SP, Parekh VS, Sulam J, Yi PH (2023) Medical imaging data science competitions should report dataset demographics and evaluate for bias. Nat Med. https://doi.org/10.1038/s41591-023-02264-0
Malamateniou C, McEntee M (2022) Integration of AI in radiography practice: ten priorities for implementation. Radmagazine 48:19–20. Available from: https://www.radmagazine.com/scientificarticle/integration-of-ai-in-radiography-practice-ten-priorities-for-implementation/
Malamateniou C, Knapp KM, Pergola M, Woznitza N, Hardy M (2021) Artificial intelligence in radiography: where are we now and what does the future hold? Radiography. https://doi.org/10.1016/j.radi.2021.07.015
Hardy M, Harvey H (2020) Artificial intelligence in diagnostic imaging: impact on the radiography profession. Br J Radiol. https://doi.org/10.1259/bjr.20190840
Rainey C, O’Regan T, Matthew J et al (2021) Beauty is in the AI of the beholder: are we ready for the clinical integration of artificial intelligence in radiography? An exploratory analysis of perceived AI knowledge, skills, confidence, and education perspectives of UK radiographers. Front Digit Health. https://doi.org/10.3389/fdgth.2021.739327
Fritsch SJ, Blankenheim A, Wahl A et al (2022) Attitudes and perception of artificial intelligence in healthcare: a cross-sectional survey among patients. Digit Health. https://doi.org/10.1177/20552076221116772
Richardson JP, Smith C, Curtis S et al (2021) Patient apprehensions about the use of artificial intelligence in healthcare. NPJ Dig Med 4(1):140. https://doi.org/10.1038/s41746-021-00509-1
Funding
Open access funding provided by University of Applied Sciences and Arts Western Switzerland (HES-SO) This publication is part of the SUBREAM project funded by the Swiss Cancer Research (KFS-5460–08-2021-R).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Prof. Jérôme Schmid.
Conflict of interest
The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was not required for this study because this paper is a scoping review.
Ethical approval
Institutional review board approval was not required because this is a review paper.
Study subjects or cohorts overlap
Not applicable.
Methodology
• Scoping review
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lokaj, B., Pugliese, MT., Kinkel, K. et al. Barriers and facilitators of artificial intelligence conception and implementation for breast imaging diagnosis in clinical practice: a scoping review. Eur Radiol 34, 2096–2109 (2024). https://doi.org/10.1007/s00330-023-10181-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-023-10181-6