Abstract
Objective
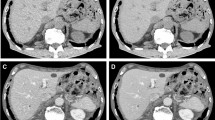
This study aimed to evaluate the image quality and lesion conspicuity of the deep learning image reconstruction (DLIR) algorithm compared with standard image reconstruction algorithms on abdominal enhanced computed tomography (CT) scanning with a wide range of body mass indexes (BMIs).
Methods
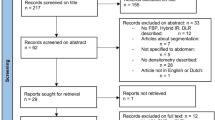
A total of 112 participants who underwent contrast-enhanced abdominal CT scans were divided into three groups according to BMIs: the 80-kVp group (BMI ≤ 23.9 kg/m2), 100-kVp group (BMI 24–28.9 kg/m2), and 120-kVp group (BMI ≥ 29 kg/m2). All images were reconstructed using filtered back projection (FBP), adaptive statistical iterative reconstruction-V of 50% level (IR), and DLIR at low, medium, and high levels (DL, DM, and DH, respectively). Subjective noise, artifact, overall image quality, and low- and high-contrast hepatic lesion conspicuity were all graded on a 5-point scale. The CT attenuation value (in HU), image noise, and contrast-to-noise ratio (CNR) were quantified and compared.
Results
DM and DH improved the qualitative and quantitative parameters compared with FBP and IR for all three BMI groups. DH had the lowest image noise and highest CNR value, while DM had the highest subjective overall image quality and low- and high-contrast lesion conspicuity scores for the three BMI groups. Based on the FBP, the improvement in image quality and lesion conspicuity of DM and DH images was greater in the 80-kVp group than in the 100-kVp and 120-kVp groups.
Conclusion
For all BMIs, DLIR improves both image quality and hepatic lesion conspicuity, of which DM would be the best choice to balance both.
Clinical relevance statement
The study suggests that utilizing DLIR, particularly at the medium level, can significantly enhance image quality and lesion visibility on abdominal CT scans across a wide range of BMIs.
Key Points
• DLIR improved the image quality and lesion conspicuity across a wide range of BMIs.
• DLIR at medium level had the highest subjective parameters and lesion conspicuity scores among all reconstruction levels.
• On the basis of the FBP, the 80-kVp group had improved image quality and lesion conspicuity more than the 100-kVp and 120-kVp groups.





Similar content being viewed by others
Abbreviations
- ASiR-V:
-
Adaptive statistical iterative reconstruction-V
- BMI:
-
Body mass index
- CNR:
-
Contrast-to-noise ratio
- CTDIvol:
-
Volume computed tomography dose index
- DLIR:
-
Deep learning image reconstruction algorithm
- DLP:
-
Dose–length product
- FBP:
-
Filtered back projection
- IR:
-
Iterative reconstruction
- ROI:
-
Region of interest
- SD:
-
Standard deviation
References
Sodickson A, Baeyens PF, Andriole KP et al (2009) Recurrent CT, cumulative radiation exposure, and associated radiation-induced cancer risks from CT of adults. Radiology 251(1):175–184
Chen LH, Jin C, Li JY et al (2018) Image quality comparison of two adaptive statistical iterative reconstruction (ASiR, ASiR-V) algorithms and filtered back projection in routine liver CT. Br J Radiol 91(1088):20170655
Mileto A, Guimaraes LS, McCollough CH, Fletcher JG, Yu L (2019) State of the art in abdominal CT: the limits of iterative reconstruction algorithms. Radiology 293(3):491–503
Noda Y, Kaga T, Kawai N et al (2021) Low-dose whole-body CT using deep learning image reconstruction: image quality and lesion detection. Br J Radiol 94(1121):20201329
Sun J, Li H, Li J et al (2021) Performance evaluation of using shorter contrast injection and 70 kVp with deep learning image reconstruction for reduced contrast medium dose and radiation dose in coronary CT angiography for children: a pilot study. Quant Imaging Med Surg 11(9):4162–4171
van Stiphout JA, Driessen J, Koetzier LR et al (2022) The effect of deep learning reconstruction on abdominal CT densitometry and image quality: a systematic review and meta-analysis. Eur Radiol 32:2921–2929
Akagi M, Nakamura Y, Higaki T et al (2019) Deep learning reconstruction improves image quality of abdominal ultra-high-resolution CT. Eur Radiol 29:6163–6171
Nakamura Y, Higaki T, Tatsugami F et al (2019) Deep learning-based CT image reconstruction: initial evaluation targeting hypovascular hepatic metastases. Radiol Artif Intell 1:e180011
Wang X, Zheng F, Xiao R et al (2021) Comparison of image quality and lesion diagnosis in abdominopelvic unenhanced CT between reduced-dose CT using deep learning post-processing and standard-dose CT using iterative reconstruction: a prospective study. Eur J Radiol 139:109735
Greffier J, Hamard A, Pereira F et al (2020) Image quality and dose reduction opportunity of deep learning image reconstruction algorithm for CT: a phantom study. Eur Radiol 30(7):3951–3959
Kawashima H, Ichikawa K, Takata T et al (2020) Performance of clinically available deep learning image reconstruction in computed tomography: a phantom study. J Med Imaging (Bellingham) 7:06350312
Park HJ, Choi SY, Lee JE et al (2022) Deep learning image reconstruction algorithm for abdominal multidetector CT at different tube voltages: assessment of image quality and radiation dose in a phantom study. Eur Radiol 32:3974–398413
Cao L, Liu X, Li J et al (2021) A study of using a deep learning image reconstruction to improve the image quality of extremely low-dose contrast-enhanced abdominal CT for patients with hepatic lesions. Br J Radiol 94(1118):20201086
Kim JH, Yoon HJ, Lee E, Kim I, Cha YK, Bak SH (2021) Validation of deep-learning image reconstruction for low-dose chest computed tomography scan: emphasis on image quality and noise. Korean J Radiol 22(1):131–138
Nishikawa M, Machida H, Shimizu Y et al (2022) Image quality and radiologists’ subjective acceptance using model-based iterative and deep learning reconstructions as adjuncts to ultrahigh-resolution CT in low-dose contrast-enhanced abdominopelvic CT: phantom and clinical pilot studies. Abdom Radiol (NY) 47(2):891–902
Nakamura Y, Narita K, Higaki T, Akagi M, Honda Y, Awai K (2021) Diagnostic value of deep learning reconstruction for radiation dose reduction at abdominal ultra-high-resolution CT. Eur Radiol 31(7):4700–4709
Zhang X, Zhang G, Xu L et al (2022) Application of deep learning reconstruction of ultra-low-dose abdominal CT in the diagnosis of renal calculi. Insights Imaging 13:163
Mileto A, Zamora DA, Alessio AM et al (2018) CT detectability of small low-contrast hypoattenuating focal lesions: iterative reconstructions versus filtered back projection. Radiology 289:443–454
Huda W, Scalzetti EM, Levin G (2000) Technique factors and image quality as functions of patient weight at abdominal CT. Radiology 217(2):430–435
Lv P, Zhou Z, Liu J et al (2019) Can virtual monochromatic images from dual-energy CT replace low-kVp images for abdominal contrast-enhanced CT in small- and medium-sized patients. Eur Radiol 29(6):2878–2889
Christner JA, Kofler JM, McCollough CH (2010) Estimating effective dose for CT using dose-length product compared with using organ doses: consequences of adopting International Commission on Radiological Protection publication 103 or dual-energy scanning. AJR Am J Roentgenol 194(4):881–889
Jensen CT, Gupta S, Saleh MM et al (2022) Reduced-dose deep learning reconstruction for abdominal CT of liver metastases. Radiology 303:90–98
Nam JG, Hong JH, Kim DS, Oh J, Goo JM (2021) Deep learning reconstruction for contrast-enhanced CT of the upper abdomen: similar image quality with lower radiation dose in direct comparison with iterative reconstruction. Eur Radiol 31(8):5533–5543
Lyu P, Neely B, Solomon J et al (2021) Effect of deep learning image reconstruction in the prediction of resectability of pancreatic cancer: diagnostic performance and reader confidence. Eur J Radiol. 141:109825
Park J, Shin J, Min IK, Bae H, Kim YE, Chung YE (2022) Image quality and lesion detectability of lower-dose abdominopelvic CT obtained using deep learning image reconstruction. Korean J Radiol 23(4):402–412
Noda Y, Iritani Y, Kawai N et al (2021) Deep learning image reconstruction for pancreatic low-dose computed tomography: comparison with hybrid iterative reconstruction. Abdom Radiol (NY) 46(9):4238–4244
Lee NK, Kim S, Hong SB et al (2019) Low-dose CT with the adaptive statistical iterative reconstruction V technique in abdominal organ injury: comparison with routine-dose CT with filtered back projection. AJR Am J Roentgenol 213:659–66628
Wang JJ, Chi XT, Wang WW, Deng K (2022) Analysis of contrast-enhanced spectral chest CT optimal monochromatic imaging combined with ASIR and ASIR-V. Eur Rev Med Pharmacol Sci 26:1930–1938
Funding
This study was supported by the Key Scientific Research Project of Higher Education in Henan Province (No. 22A320057) and the Science and Technology Project of Henan province (No.222102310505).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Guarantor
The scientific guarantor of this publication is Peijie Lyu.
Conflict of interest
One of the authors (Luotong Wang) is an employee of CT imaging research center from GE Healthcare. The other coauthors who are not employees of or consultants for the company had control of inclusion of all data and information that might present a conflict of interest.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was obtained from all participates in this study.
Ethical approval
Institutional Review Board approval was obtained.
Study subjects or cohorts overlap
No study subjects or cohorts have been previously reported.
Methodology
• retrospective
• observational
• performed at one institution
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wang, H., Yue, S., Liu, N. et al. Deep learning reconstruction vs standard reconstruction for abdominal CT: the influence of BMI. Eur Radiol 34, 1614–1623 (2024). https://doi.org/10.1007/s00330-023-10179-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-023-10179-0