Abstract
Objectives
To investigate how a transition from free text to structured reporting affects reporting language with regard to standardization and distinguishability.
Methods
A total of 747,393 radiology reports dictated between January 2011 and June 2020 were retrospectively analyzed. The body and cardiothoracic imaging divisions introduced a reporting concept using standardized language and structured reporting templates in January 2016.
Reports were segmented by a natural language processing algorithm and converted into a 20-dimension document vector. For analysis, dimensionality was reduced to a 2D visualization with t-distributed stochastic neighbor embedding and matched with metadata. Linguistic standardization was assessed by comparing distinct report types’ vector spreads (e.g., run-off MR angiography) between reporting standards. Changes in report type distinguishability (e.g., CT abdomen/pelvis vs. MR abdomen) were measured by comparing the distance between their centroids.
Results
Structured reports showed lower document vector spread (thus higher linguistic similarity) compared with free-text reports overall (21.9 [free-text] vs. 15.9 [structured]; − 27.4%; p < 0.001) and for most report types, e.g., run-off MR angiography (15.2 vs. 1.8; − 88.2%; p < 0.001) or double-rule-out CT (26.8 vs. 10.0; − 62.7%; p < 0.001). No changes were observed for reports continued to be written in free text, e.g., CT head reports (33.2 vs. 33.1; − 0.3%; p = 1).
Distances between the report types’ centroids increased with structured reporting (thus better linguistic distinguishability) overall (27.3 vs. 54.4; + 99.3 ± 98.4%) and for specific report types, e.g., CT abdomen/pelvis vs. MR abdomen (13.7 vs. 37.2; + 171.5%).
Conclusion
Structured reporting and the use of factual language yield more homogenous and standardized radiology reports on a linguistic level, tailored to specific reporting scenarios and imaging studies.
Clinical relevance
Information transmission to referring physicians, as well as automated report assessment and content extraction in big data analyses, may benefit from standardized reporting, due to consistent report organization and terminology used for pathologies and normal findings.
Key Points
• Natural language processing and t-distributed stochastic neighbor embedding can transform radiology reports into numeric vectors, allowing the quantification of their linguistic standardization.
• Structured reporting substantially increases reports’ linguistic standardization (mean: − 27.4% in vector spread) and distinguishability (mean: + 99.3 ± 98.4% increase in vector distance) compared with free-text reports.
• Higher standardization and homogeneity outline potential benefits of structured reporting for information transmission and big data analyses.
Similar content being viewed by others
Introduction
Many radiology departments have switched their reporting standard from free-text reporting to structured reporting templates in the last decades [1]. The use of such templates is increasingly advocated by many radiology societies [2, 3] and has been shown to be preferred by referring physicians given higher report completeness, clarity, and comprehensibility for the reader [4, 5]. This feedback from the radiologists’ target audience depicts one of the defined goals of structured reporting, which is to optimize information transmission with regard to the “Seven C’s of effective communication.” These are completeness, conciseness, consideration, concreteness, clarity, comparison, and correctness [6]. To reach this objective, reporting templates aim to convey information on pathology or absence thereof in a structured format to facilitate readability and information retrievability [7]. However, template organization, e.g., by means of organ-based subheadings, only represents the first step toward report standardization. To fully standardize radiology reports, the additional use of a specific lexicon or language, such as RadLex, is necessary [7, 8]. The implementation of reporting templates incorporating both factors may ultimately render radiology report content equally well standardized and machine readable like laboratory values or heart rate and blood pressure measurements are already today.
Given current trends toward big data analyses and the implementation of clinical data warehouses to facilitate data mining in clinical and in research settings, the aim to standardize radiology reports is of particular interest [7]. While there have been various approaches to assess and extract data from structured and non-structured radiology reports using natural language processing algorithms in specific scenarios, e.g., presence of pulmonary embolism or incidental pulmonary nodules [9, 10], only few investigations attempted to assess the effects of a transition from free-text reporting to structured reporting on a linguistic level [11].
The aim of our study was to investigate how the broad implementation of structured reporting templates and a reporting concept emphasizing factual standardized reporting language and discouraging ambiguous terminology and hedging in two radiology subspecialty sections in a university hospital setting affects radiology reporting language. We hypothesized that the combined use of structured templates and the advocated reporting concept would lead to higher linguistic standardization of distinct report types, better linguistic distinguishability between different types of reports, and higher reporting consistency compared to free-text reporting.
Materials and methods
Data sample
All radiology reports dictated between January 2011 and June 2020 in the body, cardiothoracic, musculoskeletal imaging, and neuroradiology divisions of our tertiary care radiology department were retrospectively included without preselection. Plain report text was used for analysis. Metadata of the reported imaging study, i.e., modality, examination type (e.g., CT abdomen/pelvis), imaging protocol, and date of the examination was available for each report.
Reporting style
In January 2016, our department’s body and cardiothoracic imaging sections switched reporting routine from traditional free-text reports to structured reporting templates. Structured reporting in our case represents organized or itemized templates with headings and subheadings. Additionally, a reporting concept emphasizing factual standardized reporting language conveying certainty was implemented. For instance, the use of ambiguous language or expressions containing hedging statements, such as “prominent” or “accentuated,” was discouraged as it was shown to diminish certainty [12, 13]. Reporting templates were drafted by senior staff radiologists based on suggestions by the RSNA reporting initiative [3]. Drafts were jointly reviewed with referring physicians, and content was in some instances amended to account for clinicians’ preferences and needs specific to our institution. The templates’ findings section organization is either organ based with prepopulated normal findings (e.g., CT abdomen/pelvis), or feature based with a point-and-click approach when tailored to specific scenarios (e.g., rectal cancer staging MRI or run-off MR angiography). Examples are provided in the online supplement (figures S1 and S2).
In contrast to the body and cardiothoracic imaging sections, our musculoskeletal imaging division continued to report imaging studies in a non-structured free-text format. Finally, our neuroradiology section introduced structured reporting templates for some examinations (e.g., stroke CT) in 2019, but the majority of reports remains to be in a non-structured format. Data from these two subspecialty sections thus almost entirely consisted of free-text reports, while data from body and cardiothoracic imaging included both structured (2016–2020) and non-structured (2011–2015) radiology reports.
Data processing
Plain report text of all available radiology reports was extracted from our institutional radiology information system (RIS).
In a first step, documents were divided into reports containing a separate “findings” and “impression” section (ultrasound, CT, and MRI studies) and reports consisting of a single combined “findings and impression” section (radiographs) using regular expressions. For reports containing distinct “findings” and “impression” sections, content was separated to allow for individual assessment of both report sections. This step was necessary, since the structured or itemized format of the newly introduced reporting templates is limited to the findings section. The impression section remains to be dictated in prose style, irrespective of the subspecialty section or template used. Without separation of report content into these two sections, assessment would have been biased, even though a distinct summary style and a format using bullet points to list primary and secondary/incidental findings prioritized by importance is advocated in our department. For reports with a combined “findings and impression” section, this step was not necessary, as the newly introduced structured reporting templates for these reports (e.g., chest radiographs) also consisted of a single section only. All report content outside these two sections, i.e., patient history and procedure information, was discarded.
In a second step, report content was converted into a 20-dimension number vector using the doc2vec approach [14]. This unsupervised neural network-based technique learns continuous distributed representations for documents, taking into account the text’s semantics and word order to obtain a numeric representation of a document, or, in our case, the distinct sections of a radiology report. Its concept is based on the word2vec model, which was introduced in 2013 and is used to vectorize words within a document [15]. There, the vector distance of two distinct words in vector space represents their similarity in meaning based on context. For example, the words “strong” and “powerful” would be close together in vector space, while the vector distance between the words “strong” and “weak” would be relatively far. Instead of averaging vectors for each word in a document, the doc2vec approach incorporates an additional document vector, intending to represent the document’s concept. This is known to outperform simple-averaging of word vectors [14]. Text data was tokenized using the Natural Language Toolkit library and each document was tagged with a unique identifier. Models were initialized with a vector size of 20, an initial learning rate of 0.025, and a minimum word frequency of 1. Training was performed over 50 epochs, with the learning rate linearly decreasing at each epoch by 0.0002. Model vocabulary was constructed using the tagged data. Document and word vectors were iteratively updated through training. Upon completion, the trained models were used to infer vector representations for each document in the dataset.
In a third step, the 20-dimension document vector had to be reduced to two dimensions to allow for data plotting, visualization, and statistical analysis. We used t-distributed stochastic neighbor embedding (t-SNE) to aggregate all dimensions into two [16]. In contrast to principal component analysis, t-SNE is a non-linear dimensionality reduction technique which preserves the local structure (neighborhood) of data and is substantially less affected by outliers.
Visualization and statistical analysis
Two-dimensional data was visualized using commercially available software (Tableau 2022.1, Tableau Inc.). To facilitate visualization, data was prepared in 2-year sets (e.g., 2014 vs. 2019) with projections of 10,000 documents per year and subspecialty section. These were joined with RIS metadata (i.e., year, imaging modality and imaging protocol). Document vectors were visualized as scatter plots with RIS attributes used for color coding.
To assess the effects of structured reporting on reporting language standardization for distinct types of imaging studies, the document vector spread around their centroid was calculated separately for free-text reports and structured reports (Fig. 1a). Standard deviations were then compared between the two reporting standards using an F-test. Distinguishability of radiology reports between distinct imaging protocols was assessed by comparing the distance between the document vectors’ centroids before and after the introduction of structured reporting templates (Fig. 1b). Reporting consistency following the introduction of structured reporting templates was assessed through comparison of centroid location and vector spread between distinct years following the change in reporting standard (e.g., 2018 vs. 2019). p < 0.05 was considered to represent a statistically significant difference.
Schematic drawings how report standardization (A) and distinguishability (B) were assessed. Linguistic standardization (A) is represented by the spread (= standard deviation) of distinct radiology report types (expressed by color coding) around their centroid (= mean) in vector space. Less spread equals higher document similarity (thus higher standardization of a distinct report type). Distinguishability (B) between distinct types of radiology reports (expressed by color coding) is represented by the distance between their centroids in vector space. A higher distance between two centroids equals lower document type similarity (thus better distinguishability of the two report types)
Results
Data sample
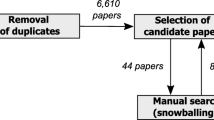
A total of 767,256 radiology reports dictated between January 2011 and June 2020 were retrieved from the RIS. In 19,863 instances, report segmentation through regular expressions failed because report content did not adhere to the expected report sections (“findings,” “impression,” or “findings and impression”). These reports were excluded from further analysis, resulting in a final study sample of 747,393 reports. Data comprised of 133,931 (17.9%) structured reports and 613,462 (82.1%) non-structured reports. A flowchart of the study sample is visualized in Fig. 2; data distribution is provided in Table 1.
Linguistic similarity of distinct radiology report types
With structured reporting, document spread around the centroids decreased overall and for most distinct radiology report types in the body and cardiothoracic imaging divisions. This means that document vectors of a specific report type (e.g., all kidney stone CT reports) were closer together in vector space and document variation among this specific report type decreased (Figs. 1a and 3).
Distribution of radiology reports in vector space before (A) and after (B) the introduction of structured reporting in body imaging. Distinguishability and clustering of distinct radiology report increased with structured templates compared with overlapping data points for free-text reporting. Neuroradiology report distribution remained unchanged between 2014 (C) and 2018 (D), given continued free-text format reporting
When comparing the newly structured reports from 2019 to free-text reports from 2014 in the body and cardiothoracic imaging sections, an overall decrease in vector spread of − 27.4% (21.9 [2014] vs. 15.9 [2019]; p < 0.001) was observed. This was true for most distinct report types from body imaging, including both highly structured templates using a point-and-click approach, e.g., run-off MR angiography (15.2 vs. 1.8; − 88.2%; p < 0.001), as well as reports with organ-based subheadings and prepopulated normal findings, e.g., polytrauma CT (23.2 vs. 10.5; − 54.7%; p < 0.001) or kidney stone CT reports (18.1 vs. 11.3; − 37.6%; p < 0.001). Body imaging reports are visualized in Fig. 3a, b. Similar decreases were observed for structured reports in the cardiothoracic imaging division, e.g., for double-rule-out CT (26.8 vs. 10.0; − 62.7%; p < 0.001), cardiac MRI (17.8 vs. 13.4; − 24.7%; p < 0.001), and supine chest radiographs (28.7 vs. 21.1; − 26.5%; p < 0.001). In both imaging divisions, decreases in vector spread were higher for level II structured reports compared with level I structured reports (− 53.4% vs. 25.4%; p < 0.001; Fig. 4).
Comparison of changes in vector spread between 2014 and 2019 for different levels of reporting. Level I structured reports represent templates with a structured layout; level II represents templates with a structured content [7]. SR = structured report
For reports from the musculoskeletal and neuroradiology sections, who continued to report imaging studies in a non-structured free-text format, no decreases in document spread were observed between 2014 and 2019 (musculoskeletal imaging) or 2014 and 2018 (neuroradiology; the year was amended to 2018 to avoid bias since some structured reporting templates were introduced in July 2019 as noted in “Materials and methods”), e.g., CT head (33.2 vs. 33.1; − 0.3%; p = 1) or CT facial bones (30.6 vs. 30.5; − 0.3%; p = 0.96). In some instances, document spread around the centroid even increased (thus, similarity further decreased), e.g., for whole spine MRI reports (37.8 vs. 43.4; + 14.8% p < 0.001). Neuroradiology reports are visualized in Fig. 3c, d. Detailed data for all report types including p values is provided in Tables 2 and 3.
Distinguishability between different radiology report types
With structured reporting templates, vector distances between the report types’ centroids increased in the body and the cardiothoracic imaging divisions (mean: 27.3 [2014] vs. 54.4 [2019]; + 99.3 ± 98.4%). This means that different report types (e.g., CT abdomen/pelvis report vs. liver ultrasound report) can be distinguished visually and statistically, as they are distributed among the coordinate system and document vectors of different report types do not overlap (Figs. 1b and 3a, b). When using the centroid of CT abdomen/pelvis reports as a reference point for body imaging reports, mean vector distance to the other report types’ centroids increased by 141.2 ± 111.5% with structured reporting, e.g., CT abdomen/pelvis vs. CT polytrauma (8.8 [2014] vs. 42.3 [2019]; + 380.7%), CT abdomen/pelvis vs. MR abdomen (13.7 vs. 37.2; + 171.5%), and CT abdomen/pelvis vs. abdominal ultrasound (37.7 vs. 77.7; + 106.1%).
Similar results were observed for reports from cardiothoracic imaging. With chest CT reports serving as reference point, mean vector distance to other report types increased by 67.6 ± 74.5%, e.g., CT chest vs. cardiac MRI (28.8 vs. 63.9; + 121.9%) and CT chest vs. MRI chest (10.1 vs. 29.4; + 191.1%). This was also true when comparing upright and supine chest radiograph reports (13.3 vs. 29.3; + 120.3%). Increases in vector distance between distinct report types are visualized in Fig. 3a, b for body imaging and in Fig. 5 for chest radiographs.
For free-text reports from the musculoskeletal and neuroradiology sections, overall vector distance remained unchanged (28.7 vs. 28.8; + 0.3 ± 27.2%). For distinct report types, the changes were variable without a clear trend. Vector distances remained unchanged in some instances, e.g., CT head vs. CT facial bones (9.8 vs. 9.8; + 0%); decreased in some instances, e.g., CT head vs. CT neck (35.7 vs. 28.7; − 19.6%); or mildly increased in some instances, e.g., CT head vs. MRI head (18.2 vs. 21.1; + 15.9%). Detailed data for all report types is provided in Tables 2 and 3.
Reporting consistency with structured reporting templates
Comparison of distinct years with sole use of structured reporting templates (e.g., 2018 vs. 2019) showed that document vectors spread remained lower than with free-text reporting or decreased even further (16.7 [2018] vs. 15.5 [2019]; p = 0.06). In body imaging, this was true, e.g., for CT chest-abdomen-pelvis (27.0 [2018] vs. 27.0 [2019]; − 0.1%; p = 0.95) and abdominal ultrasound reports (15.3 vs. 14.8; − 3.1%; p = 0.38). The continuously lower vector spread over several years thus represents a consistently higher similarity between individual documents of the same report type. With the continuous use of structured reporting templates, vector spread decreased even further over the years in some instances, e.g., CT polytrauma (16.2 vs. 13.2; − 18.6%; p < 0.001), run-off MR angiography (11.5 vs. 2.5; − 78.2%; p < 0.001), and lymph node staging ultrasound (27.1 vs. 23.8; − 52.8%; p < 0.001). Data for report types including p values is summarized in Table 4.
The location of report types’ centroids within the coordinate system remained almost similar between distinct years of structured reporting. When comparing 2018 and 2019, the mean overall difference in the centroids’ vector locations was 4.5 ± 4.4. Lowest changes in centroid location were observed for pelvic MRI (0.9), upper GI series (0.7), and urogenital ultrasound reports (0.3). The distinguishability between distinct report types thus remained high over several years of structured reporting, as the report type locations remained almost unchanged. Comparison of report distribution in vector space between 2018 and 2019 is visualized in Fig. 6. Evolution of report distribution in vector space over the course of 6 years is depicted in the online supplement (figure S3).
Distribution of radiology reports in vector space in 2018 (A) and 2019 (B) following the introduction of structured reporting templates. Centroid location in vector space and spread around the distinct report types’ centroids remain similar with structured reporting, indicating high reporting consistency
Discussion
The aim of our study was to investigate whether the transition from traditional free-text reporting to structured reporting templates and the implementation of a reporting concept emphasizing factual standardized terminology in our tertiary care radiology department have affected reporting language. We observed significantly higher linguistic similarity, thus standardization, for most radiology report types following the introduction of structured templates, expressed by a mean decrease in document spread of − 27.4% (21.9 [2014] vs. 15.9 [2019]; p < 0.001). Similarly, the linguistic distinguishability of different report types, expressed by the distance between the distinct report types’ centroids in vector space, increased with structured reporting by 99.3 ± 98.4% on average (body imaging: + 141.2 ± 111.5% and cardiothoracic imaging: + 67.6 ± 74.5%). Finally, reporting consistency between distinct years of structured reporting was high, as document spread remained lower or decreased even further compared to free-text reporting (16.7 [2018] vs. 15.5 [2019]; p = 0.06), and centroid locations of the distinct report types within the coordinate system remained almost unchanged.
Several studies demonstrated higher report completeness and consistency when structured reporting templates are used [17,18,19]. The existing literature on this topic, however, mostly comprises of qualitative assessments of single reporting templates, e.g., comparing the number of features relevant for surgical planning mentioned in structured and non-structured reports [19,20,21], and not providing a macroscopic view on how a change in reporting standard affects radiology reporting language in general. Our results from a natural language processing analysis of 747,393 radiology reports show an increase in linguistic standardization and distinguishability of distinct types of radiology reports when dedicated reporting templates and factual language are used consistently in clinical routine. These increases translate into both a more homogenous and distinct language, e.g., to describe normal findings [22], as well as a consistent format used for specific imaging examinations when reported in a predefined manner using structured templates.
Our data included structured reports of different levels, i.e., reports with standardized layouts and prepopulated normal findings, where content editing by the reporting radiologist however remains to be possible, as well as reports with standardized content, where reporting can only be performed by choosing predefined items from drop-down menus or a point-and-click approach. The latter of these two levels is considered to be the most advantageous in terms of report standardization, given the predefined way of interaction with each item within the reporting template [7, 23]. Voices in the radiology community, however, repeatedly expressed concerns with regard to highly structured reporting templates in recent years, as they might negatively impact productivity, disrupt radiologists’ search patterns, or lead to constrained thinking during the reporting process when not being able to phrase how findings are related to each other [8, 24, 25]. While we did not assess report content accuracy in this study, our results are consistent with the assumption, that higher levels of structure within the reporting templates also lead to higher report standardization. This is well depicted by the observation, that reporting templates using an itemized point-and-click approach had the highest decrease in vector spread of all report types in our study, e.g., an 88.2% decrease for run-off MR angiography reports (15.2 [free-text reporting] vs. 1.8 [structured reporting]; p < 0.001).
Higher report standardization, distinguishability, and consistency may translate into lower variance between reports of different reporting radiologists or even different institutions. This is of importance, both in clinical and research settings. With regard to clinical routine, lower report variance can improve readability and comprehensibility for the recipients of radiology reports [4, 5, 26]. Furthermore, effective communication is needed to meaningfully influence behavior of radiology report recipients [27]. Several studies already investigated referring physicians’ preferences, and found a majority of them to favor structured reports for clinical decision-making due to higher levels of completeness and comprehensibility [28,29,30]. Also, the use of heterogenous terminology may lead to miscommunication, e.g., with regard to reporting doubt or certainty, as some expressions are perceived differently by radiologists and clinicians [30,31,32]. The use of standardized language therefore may help to avoid misunderstandings, reduce the necessity of addition clarification, and improve patient care.
In addition to potential benefits in clinical routine, standardized reports may also ease workflows in research scenarios. With current trends toward the establishment of data warehouses for single- or multicentric big data analyses, it is crucial to structure or standardize the content of radiology reports. Even though several studies provided evidence that natural language processing algorithms are also able to identify relevant information on the presence of specific pathologies in free-text reports [9, 10, 33], the consistent use of structured reporting templates and a standardized terminology may render this, often time-consuming, step in data preparation redundant.
Our study has limitations. The doc2vec model is only one of several existing methods used for natural language processing and incorporates vectors for both words and document structure. Therefore, reporting templates with prepopulated normal findings may be intrinsically closer together in vector space, given that a portion of this prepopulated terminology remain constant among most reports. This, however, could also be considered an advantage of structured reporting templates, since with new therapeutic approaches, especially in complex pathologic conditions involving multiple organ systems, radiologists are demanded to specifically mention pertinent negative findings in their reports by referring physicians. While a higher level of report standardization is thought to improve readability, comprehensibility, and accuracy, we did not assess radiology reports by qualitative means. We can therefore only assume that presenting the information gathered by a specific imaging study by means of a structured report using factual language improves information transmission to the referring physician.
In conclusion, we demonstrated that the combined use of structured reporting templates and factual language decreases report variance and increases report homogeneity on a linguistic level, likely tailored to specific reporting scenarios. Information transmission to referring physicians in clinical routine, as well as automated report assessment and content extraction in big data analyses, may benefit from the implementation of these concepts, due to consistent report organization and terminology used for both pathologies and normal findings.
Abbreviations
- CT:
-
Computed tomography
- ESR:
-
European Society of Radiology
- MRI:
-
Magnetic resonance imaging
- RIS:
-
Radiology information system
- RSNA:
-
Radiological Society of North America
- t-SNE:
-
T-distributed stochastic neighbor embedding
- US:
-
Ultrasound
References
Herts BR, Gandhi NS, Schneider E et al (2019) How we do it: creating consistent structure and content in abdominal radiology report templates. AJR Am J Roentgenol 212:490–496. https://doi.org/10.2214/AJR.18.20368
European Society of Radiology (ESR) (2018) ESR paper on structured reporting in radiology. Insights Imaging 9:1–7. https://doi.org/10.1007/s13244-017-0588-8
Morgan TA, Helibrun ME, Kahn CE (2014) Reporting initiative of the Radiological Society of North America: progress and new directions. Radiology 273:642–645. https://doi.org/10.1148/radiol.14141227
Naik SS, Hanbidge A, Wilson SR (2001) Radiology reports: examining radiologist and clinician preferences regarding style and content. Am J Roentgenol 176:591–598. https://doi.org/10.2214/ajr.176.3.1760591
Heye T, Gysin V, Boll DT, Merkle EM (2018) JOURNAL CLUB: structured reporting: the voice of the customer in an ongoing debate about the future of radiology reporting. AJR Am J Roentgenol 211:964–970. https://doi.org/10.2214/AJR.18.19714
Sureka B, Garg P, Khera PS (2018) Seven C’s of effective communication. AJR Am J Roentgenol 210:W243. https://doi.org/10.2214/AJR.17.19269
Nobel JM, Kok EM, Robben SGF (2020) Redefining the structure of structured reporting in radiology. Insights Imaging 11:1–5. https://doi.org/10.1186/S13244-019-0831-6
Ganeshan D, Duong P-AT, Probyn L et al (2018) Structured reporting in radiology. Acad Radiol 25:66–73. https://doi.org/10.1016/j.acra.2017.08.005
Pham AD, Névéol A, Lavergne T et al (2014) Natural language processing of radiology reports for the detection of thromboembolic diseases and clinically relevant incidental findings. BMC Bioinformatics 15(1):266. https://doi.org/10.1186/1471-2105-15-266
Kang SK, Garry K, Chung R et al (2019) Natural language processing for identification of incidental pulmonary nodules in radiology reports. J Am Coll Radiol 16:1587–1594. https://doi.org/10.1016/J.JACR.2019.04.026
Ross SL, Ascher SM, Somwaru AS, Filice R (2017) Quantifying language before and after instituting structured CT reports. J Am Coll Radiol. https://doi.org/10.1016/j.jacr.2017.04.032
Marks AJ, Mishra A, Ormsby JW (2021) Hedging in radiology: a discussion on the ethical and financial implications on the US Health Care System. J Am Coll Radiol 18:1056. https://doi.org/10.1016/j.jacr.2021.02.030
Hoang JK (2017) Do not hedge when there is certainty. J Am Coll Radiol 14:5
Le Q, Mikolov T (2014) Distributed representations of sentences and documents. In: 31st International Conference on Machine Learning, ICML 2014. pp 2931–2939. http://proceedings.mlr.press/v32/le14.pdf
Mikolov T, Chen K, Corrado G, Dean J (2013) Efficient estimation of word representations in vector space. In: 1st International Conference on Learning Representations, ICLR 2013 - Workshop Track Proceedings. https://doi.org/10.48550/arXiv.1301.3781
sklearn.manifold.TSNE — scikit-learn 1.0.2 documentation. https://scikit-learn.org/stable/modules/generated/sklearn.manifold.TSNE.html. Accessed 1 Sep 2022
Mönch S, Andrisan T, Bernkopf K et al (2021) Structured reporting of brain MRI following mechanical thrombectomy in acute ischemic stroke patients. BMC Med Imaging 21(1):91. https://doi.org/10.1186/s12880-021-00621-4
Spiro JE, Ceelen F, Kneidinger N et al (2021) Structured reporting of computed tomography examinations in post-lung transplantation patients. J Comput Assist Tomogr 45:959–963. https://doi.org/10.1097/RCT.0000000000001209
Brook OR, Brook A, Vollmer CM et al (2015) Structured reporting of multiphasic CT for pancreatic cancer: potential effect on staging and surgical planning. Radiology 274:464–472. https://doi.org/10.1148/radiol.14140206
Nörenberg D, Sommer WH, Thasler W et al (2017) Structured reporting of rectal magnetic resonance imaging in suspected primary rectal cancer: potential benefits for surgical planning and interdisciplinary communication. Invest Radiol 52:232–239. https://doi.org/10.1097/RLI.0000000000000336
Malik RF, Hasanain A, Lafaro KJ et al (2022) Structured CT reporting of pancreatic ductal adenocarcinoma: impact on completeness of information and interdisciplinary communication for surgical planning. Abdom Radiol 47:704–714. https://doi.org/10.1007/s00261-021-03353-9
Alper DP, Shinagare AB, Hashemi SR et al (2020) Effect of a report template-enabled quality improvement initiative on use of preferred phrases for communicating normal findings in structured abdominal CT and MRI reports. AJR Am J Roentgenol 214:835–842. https://doi.org/10.2214/AJR.19.21735
Shea LAG, Towbin AJ (2019) The state of structured reporting: the nuance of standardized language. Pediatr Radiol 49:500–508. https://doi.org/10.1007/S00247-019-04345-0
Powell DK, Silberzweig JE (2015) State of structured reporting in radiology, a survey. Acad Radiol 22:226–233. https://doi.org/10.1016/j.acra.2014.08.014
Gunderman RB, McNeive LR (2014) Is structured reporting the answer? Radiology 273:7–9. https://doi.org/10.1148/radiol.14132795
Dickerson E, Davenport MS, Syed F et al (2017) Effect of template reporting of brain MRIs for multiple sclerosis on report thoroughness and neurologist-rated quality: results of a prospective quality improvement project. J Am Coll Radiol 14:371-379.e1. https://doi.org/10.1016/J.JACR.2016.09.037
Davenport MS, Weinstein S (2022) What is it we do here? AJR Am J Roentgenol 218:184–185. https://doi.org/10.2214/AJR.21.26565
Schwartz LH, Panicek DM, Berk AR et al (2011) Improving communication of diagnostic radiology findings through structured reporting. Radiology 260:174–181. https://doi.org/10.1148/radiol.11101913
Heye T, Gysin V, Boll DT, Merkle EM (2018) Structured reporting: the voice of the customer in an ongoing debate about the future of radiology reporting. Am J Roentgenol 211:964–970. https://doi.org/10.2214/AJR.18.19714
Jorg T, Halfmann MC, Arnhold G et al (2023) Implementation of structured reporting in clinical routine: a review of 7 years of institutional experience. Insights Imaging 14:1–10. https://doi.org/10.1186/S13244-023-01408-7
Khorasani R, Bates DW, Teeger S et al (2003) Is terminology used effectively to convey diagnostic certainty in radiology reports? Acad Radiol 10:685–688. https://doi.org/10.1016/S1076-6332(03)80089-2
Lee B, Whitehead MT (2017) Radiology reports: what YOU think you’re saying and what THEY think you’re saying. Curr Probl Diagn Radiol 46(3):186–195. https://doi.org/10.1067/j.cpradiol.2016.11.005
Nobel JM, Puts S, Weiss J et al (2021) T-staging pulmonary oncology from radiological reports using natural language processing: translating into a multi-language setting. Insights Imaging 12. https://doi.org/10.1186/S13244-021-01018-1
Funding
Open access funding provided by University of Basel The authors state that this work has not received any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Jan Vosshenrich.
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was not required for this study because no patient identifiers were used in any part of our retrospective study.
Ethical approval
Institutional Review Board approval was not required because no patient identifiers were used in any part of our retrospective study.
Study subjects or cohorts overlap
Study subjects or cohorts have not been previously reported.
Methodology
• retrospective
• experimental
• performed at one institution
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Vosshenrich, J., Nesic, I., Boll, D.T. et al. Investigating the impact of structured reporting on the linguistic standardization of radiology reports through natural language processing over a 10-year period. Eur Radiol 33, 7496–7506 (2023). https://doi.org/10.1007/s00330-023-10050-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-023-10050-2