Abstract
Objective
To compare sacroiliac joint (SIJ) lesions on MRI in women with versus without axial spondyloarthritis (ax-SpA) and establish an algorithm to determine whether such lesions are due to ax-SpA.
Methods
This retrospective comparative study assessed bone marrow edema (BME), sclerosis, erosions, osteophytes, and ankylosis at the SIJ in two groups of women, one with and another without ax-SpA. Sensitivity and specificity were calculated for combinations/characteristics of lesions, using rheumatologists’ assessment with assessment of spondyloarthritis international society (ASAS) criteria as the gold standard for diagnosis of ax-SpA.
Results
Compared to women without ax-SpA, women with ax-SpA had more BME (61% vs 17%, p < 0.001), sclerosis (40% vs 22%, p < 0.001), erosions (35% vs 5%, p < 0.001), and ankylosis (2% vs 0%, p = 0.007), but less osteophytes (5% vs 33%, p < 0.001). The ASAS MRI criteria yielded 59% sensitivity and 88% specificity, while a new algorithm achieved 56% sensitivity and 95% specificity using the following criteria: no osteophytes at the SIJ and either (i) BME at the SIJ with at least one dimension ≥ 8 mm or (ii) at least one erosion at the SIJ.
Conclusions
We recommend the following pragmatic algorithm for MRI diagnosis of ax-SpA in women: no osteophytes at the SIJ and either (i) BME at the SIJ with at least one dimension ≥ 8 mm or (ii) at least one erosion at the SIJ. The false positive rate when using the new algorithm (3.3%) is less than half than when using the ASAS MRI criteria (7.7%); thus, its application in clinical practice could reduce overdiagnosis and prevent overtreatment of ax-SpA.
Clinical relevance statement
The developed algorithm has a false-positive rate that is less than half than when using the ASAS MRI criteria (3.3% vs 7.7%), thus its application in clinical practice could reduce overdiagnosis and prevent overtreatment of axial spondyloarthritis.
Key Points
• Compared to women without axial spondyloarthritis (ax-SpA), women with ax-SpA had a significantly higher prevalence of bone marrow edema (BME), sclerosis, erosions, and ankylosis, but a significantly lower prevalence of osteophytes.
• A new algorithm for positive ax-SpA based on sacroiliac joint MRI was developed: no osteophytes at the sacroiliac joint (SIJ) and either (i) BME at the SIJ with at least one dimension ≥ 8 mm or (ii) at least one erosion at the SIJ.
• We recommend this new algorithm for diagnosis of ax-SpA in women, as it has a significantly better specificity than the assessment of spondyloarthritis international society (ASAS) MRI criteria and less than half the false positive rate; thus, its application in clinical practice could reduce overdiagnosis and prevent overtreatment of ax-SpA.




Similar content being viewed by others
Abbreviations
- ASAS:
-
Assessment of spondyloarthritis international society
- AUC:
-
Area under the curve
- ax-SpA:
-
Axial spondyloarthritis
- BME:
-
Bone marrow edema
- ICC:
-
Intraclass correlation coefficient
- MRI:
-
Magnetic resonance imaging
- NPV:
-
Negative predictive value
- PACS:
-
Picture archiving communication system
- PPV:
-
Positive predictive value
- SIJ:
-
Sacroiliac joint
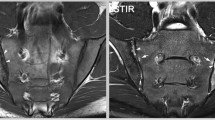
- STIR:
-
Short Tau Inversion Recovery
References
Rudwaleit M, van der Heijde D, Landewé R et al (2011) The Assessment of SpondyloArthritis International Society classification criteria for peripheral spondyloarthritis and for spondyloarthritis in general. Ann Rheum Dis 70:25–31
Oostveen J, Prevo R, den Boer J, van de Laar M (1999) Early detection of sacroiliitis on magnetic resonance imaging and subsequent development of sacroiliitis on plain radiography. A prospective, longitudinal study. J Rheumatol 26:1953–1958
Mease PJ, McLean RR, Dube B et al (2021) Comparison of men and women with axial spondyloarthritis in the US-based Corrona Psoriatic Arthritis/Spondyloarthritis Registry. J Rheumatol 48:1528–1536
Wright GC, Kaine J, Deodhar A (2020) Understanding differences between men and women with axial spondyloarthritis. Semin Arthritis Rheum 50:687–694
Plier M, Nzeusseu Toukap A, Michoux N et al (2021) Diagnostic performance of sacroiliac joint MRI and added value of spine MRI to detect active spondyloarthritis. Diagn Interv Imaging 102:171–180
Campos-Correia D, Sudoł-Szopińska I, Diana Afonso P (2019) Are we overcalling sacroiliitis on MRI? Differential diagnosis that every rheumatologist should know - Part I. Acta Reumatol Port 44:29–41
Østergaard M (2020) MRI of the sacroiliac joints: what is and what is not sacroiliitis? Curr Opin Rheumatol 32:357–364
De Rycke L, Maas M, Tak PP, Baeten D (2010) ‘MRI-tis’ in the early diagnosis of axial SpA: issues and limitations. Nat Rev Rheumatol 6:666–669
Jans L, Coeman L, Van Praet L et al (2014) How sensitive and specific are MRI features of sacroiliitis for diagnosis of spondyloarthritis in patients with inflammatory back pain? JBR-BTR 97:202–205
Agten CA, Zubler V, Zanetti M et al (2018) Postpartum bone marrow edema at the sacroiliac joints may mimic sacroiliitis of axial spondyloarthritis on MRI. AJR Am J Roentgenol 211:1306–1312
Hoballah A, Lukas C, Leplat C et al (2020) MRI of sacroiliac joints for the diagnosis of axial SpA: prevalence of inflammatory and structural lesions in nulliparous, early postpartum and late postpartum women. Ann Rheum Dis 79:1063–1069
de Winter J, de Hooge M, van de Sande M et al (2018) Magnetic resonance imaging of the sacroiliac joints indicating sacroiliitis according to the Assessment of SpondyloArthritis international Society definition in healthy individuals, runners, and women with postpartum back pain. Arthritis Rheumatol 70:1042–1048
Pialat JB, Di Marco L, Feydy A et al (2016) Sacroiliac joints imaging in axial spondyloarthritis. Diagn Interv Imaging 97:697–708
Sieper J, Rudwaleit M, Baraliakos X et al (2009) The Assessment of SpondyloArthritis international Society (ASAS) handbook: a guide to assess spondyloarthritis. Ann Rheum Dis 68(Suppl 2):ii1-44
de Vet HC, Mokkink LB, Terwee CB, Hoekstra OS, Knol DL (2013) Clinicians are right not to like Cohen’s kappa. BMJ 346:f2125
Benchoufi M, Matzner-Lober E, Molinari N, Jannot AS, Soyer P (2020) Interobserver agreement issues in radiology. Diagn Interv Imaging 101:639–641
Cicchetti DV, Showalter D, Rosenheck R (1997) A new method for assessing interexaminer agreement when multiple ratings are made on a single subject: applications to the assessment of neuropsychiatric symtomatology. Psychiatry Res 72:51–63
Poddubnyy D (2020) Classification vs diagnostic criteria: the challenge of diagnosing axial spondyloarthritis. Rheumatology (Oxford) 59:iv6–iv17
El Rafei M, Badr S, Lefebvre G et al (2018) Sacroiliac joints: anatomical variations on MR images. Eur Radiol 28:5328–5337
Varkas G, de Hooge M, Renson T et al (2018) Effect of mechanical stress on magnetic resonance imaging of the sacroiliac joints: assessment of military recruits by magnetic resonance imaging study. Rheumatology (Oxford) 57:508–513
Weber U, Jurik AG, Zejden A et al (2018) Frequency and anatomic distribution of magnetic resonance imaging features in the sacroiliac joints of young athletes: exploring “background noise” toward a data-driven definition of sacroiliitis in early spondyloarthritis. Arthritis Rheumatol 70:736–745
Link TM, Li X (2011) Bone marrow changes in osteoarthritis. Semin Musculoskelet Radiol 15:238–246
Maksymowych WP, Lambert RG, Østergaard M et al (2019) MRI lesions in the sacroiliac joints of patients with spondyloarthritis: an update of definitions and validation by the ASAS MRI working group. Ann Rheum Dis 78:1550–1558
Deppe D, Hermann KG, Proft F et al (2021) CT-like images of the sacroiliac joint generated from MRI using susceptibility-weighted imaging (SWI) in patients with axial spondyloarthritis. RMD Open 7:e001656
Li Y, Xiong Y, Hou B et al (2022) Comparison of zero echo time MRI with T1-weighted fast spin echo for the recognition of sacroiliac joint structural lesions using CT as the reference standard. Eur Radiol 32:3963–3973
Acknowledgements
The authors are grateful to Celine Engrand for her assistance with data collection.
Funding
This study has received funding by Montpellier University Hospital, for statistical analysis and manuscript writing.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Catherine Cyteval.
Conflict of interest
The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Statistics and biometry
One of the authors has significant statistical expertise.
Informed consent
Written informed consent was obtained from all subjects (patients) in this study.
Ethical approval
Institutional Review Board approval was obtained.
Study subjects or cohorts overlap
Some study subjects or cohorts have been previously reported in Hoballah et al, 2020 (http://dx.doi.org/10.1136/ annrheumdis-2020-217208).
Methodology
• Retrospective
• Case–control study
• Multicentre study
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Pastor, M., Lukas, C., Ramos-Pascual, S. et al. Sacroiliac joint MRI for diagnosis of ax-SpA: algorithm to improve the specificity of the current ASAS MRI criteria. Eur Radiol 33, 8645–8655 (2023). https://doi.org/10.1007/s00330-023-09969-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-023-09969-3