Abstract
Objectives
Adult solitary intra-axial cerebellar tumors are uncommon. Their presurgical differentiation based on neuroimaging is crucial, since management differs substantially. Comprehensive full assessment of MR dynamic-susceptibility-contrast perfusion-weighted imaging (DSC-PWI) may reveal key differences between entities. This study aims to provide new insights on perfusion patterns of these tumors and to explore the potential of DSC-PWI in their presurgical discrimination.
Methods
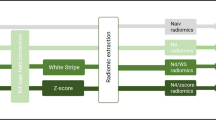
Adult patients with a solitary cerebellar tumor on presurgical MR and confirmed histological diagnosis of metastasis, medulloblastoma, hemangioblastoma, or pilocytic astrocytoma were retrospectively retrieved (2008–2023). Volumetric segmentation of tumors and normal-appearing white matter (for normalization) was semi-automatically performed on CE-T1WI and coregistered with DSC-PWI. Mean normalized values per patient tumor-mask of relative cerebral blood volume (rCBV), percentage of signal recovery (PSR), peak height (PH), and normalized time-intensity curves (nTIC) were extracted. Statistical comparisons were done. Then, the dataset was split into training (75%) and test (25%) cohorts and a classifier was created considering nTIC, rCBV, PSR, and PH in the model.
Results
Sixty-eight patients (31 metastases, 13 medulloblastomas, 13 hemangioblastomas, and 11 pilocytic astrocytomas) were included. Relevant differences between tumor types’ nTICs were demonstrated. Hemangioblastoma showed the highest rCBV and PH, pilocytic astrocytoma the highest PSR. All parameters showed significant differences on the Kruskal–Wallis tests (p < 0.001). The classifier yielded an accuracy of 98% (47/48) in the training and 85% (17/20) in the test sets.
Conclusions
Intra-axial cerebellar tumors in adults have singular and significantly different DSC-PWI signatures. The combination of perfusion metrics through data-analysis rendered excellent accuracies in discriminating these entities.
Clinical relevance statement
In this study, the authors constructed a classifier for the non-invasive imaging presurgical diagnosis of adult intra-axial cerebellar tumors. The resultant tool can be a support for decision-making in the clinical practice and enables optimal personalized patient management.
Key Points
• Adult intra-axial cerebellar tumors exhibit specific, singular, and statistically significant different MR dynamic-susceptibility-contrast perfusion-weighted imaging (DSC-PWI) signatures.
• Data-analysis, applied to MR DSC-PWI, could provide added value in the presurgical diagnosis of solitary cerebellar metastasis, medulloblastoma, hemangioblastoma, and pilocytic astrocytoma.
• A classifier based on DSC-PWI metrics yields excellent accuracy rates and could be used as a support tool for radiologic diagnosis with clinician-friendly displays.




Similar content being viewed by others
Abbreviations
- DSC-PWI:
-
Dynamic-susceptibility-contrast perfusion-weighted imaging
- nTIC:
-
Normalized time-intensity curves
- PH:
-
Peak height
- PSR:
-
Percentage of signal recovery
- rCBV:
-
Relative cerebral blood volume
References
Ostrom QT, Patil N, Cioffi G et al (2020) CBTRUS statistical report: primary brain and other central nervous system tumors diagnosed in the United States in 2013–2017. Neuro Oncol 22:iv1–iv96. https://doi.org/10.1093/neuonc/noaa200
Shih RY, Smirniotopoulos JG (2016) Posterior fossa tumors in adult patients. Neuroimaging Clin N Am 26:493–510. https://doi.org/10.1016/j.nic.2016.06.003
Wade A, Hayhurst C, Amato-Watkins A et al (2013) Cerebellar pilocytic astrocytoma in adults: a management paradigm for a rare tumour. Acta Neurochir (Wien) 155:1431–1435. https://doi.org/10.1007/s00701-013-1790-1
Sunderland GJ, Jenkinson MD, Zakaria R (2016) Surgical management of posterior fossa metastases. J Neurooncol 130:535–542. https://doi.org/10.1007/s11060-016-2254-2
Kuharic M, Jankovic D, Splavski B et al (2018) Hemangioblastomas of the posterior cranial fossa in adults: demographics, clinical, morphologic, pathologic, surgical features, and outcomes. A systematic review. World Neurosurg 110:e1049–e1062. https://doi.org/10.1016/j.wneu.2017.11.173
Franceschi E, Giannini C, Furtner J et al (2022) Adult medulloblastoma: updates on current management and future perspectives. Cancers (Basel) 14. https://doi.org/10.3390/cancers14153708
Jhaveri M, Osborn A, Salzman K (2020) Diagnostic imaging: brain, 4th ed. Elsevier, Salt Lake City, UT
Kurokawa R, Kurokawa M, Baba A et al (2022) Differentiation of pilocytic astrocytoma, medulloblastoma, and hemangioblastoma on diffusion-weighted and dynamic susceptibility contrast perfusion MRI. Medicine (Baltimore) 101:e31708. https://doi.org/10.1097/MD.0000000000031708
Neska-Matuszewska M, Zimny A, Bladowska J et al (2018) The role of diffusion and perfusion magnetic resonance imaging in differentiation of haemangioblastomas and pilocytic astrocytomas. Polish J Radiol 83:e197–e203. https://doi.org/10.5114/pjr.2018.75870
Hakyemez B, Erdogan C, Bolca N et al (2006) Evaluation of different cerebral mass lesions by perfusion-weighted MR imaging. J Magn Reson Imaging 24:817–824
She D, Yang X, Xing Z, Cao D (2016) Differentiating hemangioblastomas from brain metastases using diffusion-weighted imaging and dynamic susceptibility contrast-enhanced perfusion-weighted MR imaging. AJNR Am J Neuroradiol 37:1844–1850. https://doi.org/10.3174/ajnr.A4809
Cha S, Lupo JM, Chen MH et al (2007) Differentiation of glioblastoma multiforme and single brain metastasis by peak height and percentage of signal intensity recovery derived from dynamic susceptibility-weighted contrast-enhanced perfusion MR imaging. AJNR Am J Neuroradiol 28:1078–1084. https://doi.org/10.3174/ajnr.A0484
Pons-Escoda A, Garcia-Ruiz A, Naval-Baudin P et al (2020) Presurgical identification of primary central nervous system lymphoma with normalized time-intensity curve: a pilot study of a new method to analyze DSC-PWI. AJNR Am J Neuroradiol 41:1816–1824. https://doi.org/10.3174/ajnr.A6761
Pons-Escoda A, García-Ruíz A, Naval-Baudin P et al (2022) Diffuse large B-cell Epstein-Barr virus-positive primary CNS lymphoma in non-AIDS patients: high diagnostic accuracy of DSC perfusion metrics. AJNR Am J Neuroradiol 43:1567–1574. https://doi.org/10.3174/ajnr.A7668
Pons-Escoda A, Garcia-Ruiz A, Naval-Baudin P et al (2022) Voxel-level analysis of normalized DSC-PWI time-intensity curves: a potential generalizable approach and its proof of concept in discriminating glioblastoma and metastasis. Eur Radiol. https://doi.org/10.1007/s00330-021-08498-1
Boxerman JL, Schmainda KM, Weisskoff RM (2006) Relative cerebral blood volume maps corrected for contrast agent extravasation significantly correlate with glioma tumor grade, whereas uncorrected maps do not. AJNR Am J Neuroradiol 27:859–867
Kuhn M, Wing J, Weston S, Williams A (2022) “Caret”: classification and regression training. R package version 6.0–93
Team R R Core Team (2020) R: a language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria
Barajas RF, Politi LS, Anzalone N et al (2021) Consensus recommendations for MRI and PET imaging of primary central nervous system lymphoma: guideline statement from the International Primary CNS Lymphoma Collaborative Group (IPCG). Neuro Oncol 23:1056–1071. https://doi.org/10.1093/neuonc/noab020
Boxerman JL, Quarles CC, Hu LS et al (2020) Consensus recommendations for a dynamic susceptibility contrast MRI protocol for use in high-grade gliomas. Neuro Oncol 22:1262–1275. https://doi.org/10.1093/neuonc/noaa141
Kaufmann TJ, Smits M, Boxerman J et al (2020) Consensus recommendations for a standardized brain tumor imaging protocol for clinical trials in brain metastases. Neuro Oncol 22:757–772. https://doi.org/10.1093/neuonc/noaa030
Ho CY, Cardinal JS, Kamer AP et al (2016) Contrast leakage patterns from dynamic susceptibility contrast perfusion MRI in the grading of primary pediatric brain tumors. AJNR Am J Neuroradiol 37:544–551. https://doi.org/10.3174/ajnr.A4559
Cindil E, Sendur HN, Cerit MN et al (2021) Validation of combined use of DWI and percentage signal recovery-optimized protocol of DSC-MRI in differentiation of high-grade glioma, metastasis, and lymphoma. Neuroradiology 63:331–342. https://doi.org/10.1007/s00234-020-02522-9
Acknowledgements
Albert Pons-Escoda and Carles Majos acknowledge a grant from the Instituto de Salud Carlos III (PI20/00360). Pablo Gago-Ferrero acknowledges a Ramón y Cajal grant (RYC2019-027913-I). The authors want to acknowledge Pilar Lopez-Ubeda, PhD, from HT Medica. She participated in retrospective patient recruitment through advanced natural language processing methods. The authors thank CERCA Programme/Generalitat de Catalunya for institutional support.
Funding
No funding was received.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Albert Pons-Escoda.
Conflict of interest
Albert Pons-Escoda is a member of the European Radiology Scientific Editorial Board. He has not taken part in review or selection process for this article. The remaining authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
Several authors have significant statistical expertise; mainly Alonso Garcia-Ruiz and Ruben Gil-Solsona have expertise in statistics, data analysis, and machine learning.
Informed consent
Written informed consent was waived by the institutional review board.
Ethical approval
Institutional review board approval was obtained. This study has been approved by The Research Ethics Committee of the Hospital Universitari de Bellvitge (PR306/22).
Study subjects or cohorts overlap
None of the study subjects or cohorts has been previously reported.
Methodology
• retrospective
• diagnostic study
• performed at one institution
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Twitter: @PonsEscoda
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Pons-Escoda, A., Garcia-Ruiz, A., Garcia-Hidalgo, C. et al. MR dynamic-susceptibility-contrast perfusion metrics in the presurgical discrimination of adult solitary intra-axial cerebellar tumors. Eur Radiol 33, 9120–9129 (2023). https://doi.org/10.1007/s00330-023-09892-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-023-09892-7