Abstract
Objectives
To develop deep learning–assisted diagnosis models based on CT images to facilitate radiologists in differentiating benign and malignant parotid tumors.
Methods
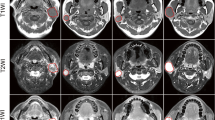
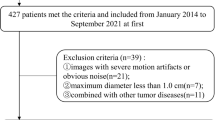
Data from 573 patients with histopathologically confirmed parotid tumors from center 1 (training set: n = 269; internal-testing set: n = 116) and center 2 (external-testing set: n = 188) were retrospectively collected. Six deep learning models (MobileNet V3, ShuffleNet V2, Inception V3, DenseNet 121, ResNet 50, and VGG 19) based on arterial-phase CT images, and a baseline support vector machine (SVM) model integrating clinical-radiological features with handcrafted radiomics signatures were constructed. The performance of senior and junior radiologists with and without optimal model assistance was compared. The net reclassification index (NRI) and integrated discrimination improvement (IDI) were calculated to evaluate the clinical benefit of using the optimal model.
Results
MobileNet V3 had the best predictive performance, with sensitivity increases of 0.111 and 0.207 (p < 0.05) in the internal- and external-testing sets, respectively, relative to the SVM model. Clinical benefit and overall efficiency of junior radiologist were significantly improved with model assistance; for the internal- and external-testing sets, respectively, the AUCs improved by 0.128 and 0.102 (p < 0.05), the sensitivity improved by 0.194 and 0.120 (p < 0.05), the NRIs were 0.257 and 0.205 (p < 0.001), and the IDIs were 0.316 and 0.252 (p < 0.001).
Conclusions
The developed deep learning models can assist radiologists in achieving higher diagnostic performance and hopefully provide more valuable information for clinical decision-making in patients with parotid tumors.
Key Points
• The developed deep learning models outperformed the traditional SVM model in predicting benign and malignant parotid tumors.
• Junior radiologist can obtain greater clinical benefits with assistance from the optimal deep learning model.
• The clinical decision-making process can be accelerated in patients with parotid tumors using the established deep learning model.






Similar content being viewed by others
Abbreviations
- APT:
-
Amide proton transfer
- ASL:
-
Arterial spin labelling
- AUC:
-
Area under the curve
- BPTs:
-
Benign parotid tumors
- CI:
-
Confidence interval
- CNNs:
-
Convolutional neural networks
- CT:
-
Computed tomography
- FNA:
-
Fine-needle aspiration
- Grad-CAM:
-
Gradient-weighted class activation mapping
- HU:
-
Hounsfield unit
- ICC:
-
Intraclass correlation coefficient
- IDI:
-
Integrated discrimination improvement
- IQR:
-
Interquartile range
- IST:
-
Infiltration of surrounding tissues
- IVIM:
-
Intravoxel incoherent motion
- LASSO:
-
Least absolute shrinkage and selection operator
- LM:
-
Lymphatic metastasis
- ML:
-
Machine learning
- MPTs:
-
Malignant parotid tumors
- MRI:
-
Magnetic resonance imaging
- NPV:
-
Negative predictive value
- NRI:
-
Net reclassification index
- PPV:
-
Positive predictive value
- ROC:
-
Receiver operating characteristic
- ROI:
-
Region of interest
- SGD:
-
Stochastic gradient descent
- SMOTE:
-
Synthetic minority oversampling technique
- SVM:
-
Support vector machine
- USCBs:
-
Ultrasound-guided core biopsies
References
Bussu F, Parrilla C, Rizzo D, Almadori G, Paludetti G, Galli J (2011) Clinical approach and treatment of benign and malignant parotid masses, personal experience. Acta Otorhinolaryngol Ital 31:135–43
Moore MG, Yueh B, Lin DT et al (2021) Controversies in the workup and surgical management of parotid neoplasms. Otolaryngol Head Neck Surg 164:27–36
Alzumaili B, Xu B, Saliba M et al (2022) Clinicopathologic characteristics and prognostic factors of primary and recurrent pleomorphic adenoma: a single institution retrospective study of 705 cases. Am J Surg Pathol 46:854–862
Liu CC, Jethwa AR, Khariwala SS, Johnson J, Shin JJ (2016) Sensitivity, specificity, and posttest probability of parotid fine-needle aspiration: a systematic review and meta-analysis. Otolaryngol Head Neck Surg 154:9–23
Witt BL, Schmidt RL (2014) Ultrasound-guided core needle biopsy of salivary gland lesions: a systematic review and meta-analysis. Laryngoscope 124:695–700
Zbaren P, Triantafyllou A, Devaney KO et al (2018) Preoperative diagnostic of parotid gland neoplasms: fine-needle aspiration cytology or core needle biopsy? Eur Arch Otorhinolaryngol 275:2609–2613
Kong X, Li H, Han Z (2019) The diagnostic role of ultrasonography, computed tomography, magnetic resonance imaging, positron emission tomography/computed tomography, and real-time elastography in the differentiation of benign and malignant salivary gland tumors: a meta-analysis. Oral Surg Oral Med Oral Pathol Oral Radiol 128(431–443):e431
Kato H, Kanematsu M, Watanabe H et al (2015) Perfusion imaging of parotid gland tumours: usefulness of arterial spin labeling for differentiating Warthin’s tumours. Eur Radiol 25:3247–3254
Law BKH, King AD, Ai QY et al (2018) Head and neck tumors: amide proton transfer MRI. Radiology 288:782–790
Ma G, Xu XQ, Zhu LN et al (2021) Intravoxel incoherent motion magnetic resonance imaging for assessing parotid gland tumors: correlation and comparison with arterial spin labeling imaging. Korean J Radiol 22:243–252
Gao R, Zhao S, Aishanjiang K et al (2021) Deep learning for differential diagnosis of malignant hepatic tumors based on multi-phase contrast-enhanced CT and clinical data. J Hematol Oncol 14:154
Rodriguez-Ruiz A, Krupinski E, Mordang JJ et al (2019) Detection of breast cancer with mammography: effect of an artificial intelligence support system. Radiology 290:305–314
Zheng Y, Zhou D, Liu H, Wen M (2022) CT-based radiomics analysis of different machine learning models for differentiating benign and malignant parotid tumors. Eur Radiol 32:6953–6964
Zheng YM, Li J, Liu S et al (2021) MRI-Based radiomics nomogram for differentiation of benign and malignant lesions of the parotid gland. Eur Radiol 31:4042–4052
Chang YJ, Huang TY, Liu YJ, Chung HW, Juan CJ (2021) Classification of parotid gland tumors by using multimodal MRI and deep learning. NMR Biomed 34:e4408
Gunduz E, Alçin OF, Kizilay A, Yildirim IO (2022) Deep learning model developed by multiparametric MRI in differential diagnosis of parotid gland tumors. Eur Arch Otorhinolaryngol 279:5389–5399
Zhang H, Lai H, Wang Y et al (2021) Research on the classification of benign and malignant parotid tumors based on transfer learning and a convolutional neural network. IEEE Access 9:40360–40371
Yuan J, Fan Y, Lv X et al (2020) Research on the practical classification and privacy protection of CT images of parotid tumors based on ResNet50 model. Journal of Physics: Conference Series 1576
Zheng X, Yao Z, Huang Y et al (2020) Deep learning radiomics can predict axillary lymph node status in early-stage breast cancer. Nat Commun 11:1236
Wang K, Lu X, Zhou H et al (2019) Deep learning radiomics of shear wave elastography significantly improved diagnostic performance for assessing liver fibrosis in chronic hepatitis B: a prospective multicentre study. Gut 68:729–741
Lecun Y, Bengio Y, Hinton G (2015) Deep learning. Nature 521:436–444
Yu Q, Wang A, Gu J et al (2022) Multiphasic CT-based radiomics analysis for the differentiation of benign and malignant parotid tumors. Front Oncol 12:913898
He Z, Mao Y, Lu S et al (2022) Machine learning-based radiomics for histological classification of parotid tumors using morphological MRI: a comparative study. Eur Radiol 32:8099–8110
Selvaraju RR, Cogswell M, Das A, Vedantam R, Parikh D, Batra D (2020) Grad-CAM: visual explanations from deep networks via gradient-based localization. International Journal of Computer Vision 128:336–359
Zuo H (2021) The clinical characteristics and CT findings of parotid and submandibular gland tumours. J Oncol 2021:8874100
Tartaglione T, Botto A, Sciandra M et al (2015) Differential diagnosis of parotid gland tumours: which magnetic resonance findings should be taken in account? Acta Otorhinolaryngol Ital 35:314–320
Aasen MH, Hutz MJ, Yuhan BT, Britt CJ (2022) Deep lobe parotid tumors: a systematic review and meta-analysis. Otolaryngol Head Neck Surg 166:60–67
Coudert H, Mirafzal S, Dissard A, Boyer L, Montoriol PF (2021) Multiparametric magnetic resonance imaging of parotid tumors: a systematic review. Diagn Interv Imaging 102:121–130
Li X, Zhang S, Zhang Q et al (2019) Diagnosis of thyroid cancer using deep convolutional neural network models applied to sonographic images: a retrospective, multicohort, diagnostic study. Lancet Oncol 20:193–201
Al Ajmi E, Forghani B, Reinhold C, Bayat M, Forghani R (2018) Spectral multi-energy CT texture analysis with machine learning for tissue classification: an investigation using classification of benign parotid tumours as a testing paradigm. Eur Radiol 28:2604–2611
Lee SB, Cho YJ, Hong Y et al (2022) Deep learning-based image conversion improves the reproducibility of computed tomography radiomics features: a phantom study. Invest Radiol 57:308–317
Meyer M, Ronald J, Vernuccio F et al (2019) Reproducibility of CT radiomic features within the same patient: influence of radiation dose and CT reconstruction settings. Radiology 293:583–591
Jimenez-Del-Toro O, Aberle C, Bach M et al (2021) The discriminative power and stability of radiomics features with computed tomography variations: task-based analysis in an anthropomorphic 3d-printed CT phantom. Invest Radiol 56:820–825
Zhu Y, Meng Z, Fan X et al (2022) Deep learning radiomics of dual-modality ultrasound images for hierarchical diagnosis of unexplained cervical lymphadenopathy. BMC Med 20:269
Fujima N, Andreu-Arasa VC, Onoue K et al (2021) Utility of deep learning for the diagnosis of otosclerosis on temporal bone CT. Eur Radiol 31:5206–5211
Howard A, Sandler M, Chen B et al (2019) Searching for MobileNetV3. In: 2019 IEEE/CVF International Conference on Computer Vision (ICCV) 1314-1324
Acknowledgements
This study received support from the Foundation of Science and Technology Bureau of Yuzhong District, Chongqing, China (Grant No. 20190111) and the Natural Science Foundation of Chongqing, China (Grant No. cstc2021jcyj-msxmX0020). We thank the American Journal Experts (AJE) for their assistance with language editing, and we appreciate the OnekeyAI platform and its developers, as well as all of the individuals who participated in these studies and each of the researchers and technicians who made this work possible.
Funding
This study received support from the Foundation of Science and Technology Bureau of Yuzhong District, Chongqing, China (Grant No. 20190111), and the Natural Science Foundation of Chongqing, China (Grant No. cstc2021jcyj-msxmX0020).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Guarantor
The scientific guarantor of this publication is Juan Peng.
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
One of the authors (Juan Peng) has significant statistical expertise and is identified as the statistical guarantor for the statistical analysis used in this study.
Informed consent
Written informed consent was waived by the institutional review board.
Ethical approval
Institutional review board approval was obtained.
Study subjects or cohorts overlap
Some study subjects or cohorts have been previously reported in Front Oncol. 2022;12:913898. https://doi.org/10.3389/fonc.2022.913898.
Methodology
• retrospective
• diagnostic or prognostic study
• multicenter study
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yu, Q., Ning, Y., Wang, A. et al. Deep learning–assisted diagnosis of benign and malignant parotid tumors based on contrast-enhanced CT: a multicenter study. Eur Radiol 33, 6054–6065 (2023). https://doi.org/10.1007/s00330-023-09568-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-023-09568-2