Abstract
Objectives
To assess coronary artery calcification (CAC) on non-contrast non-ECG-gated CT thorax (NC-NECG-CTT) and to evaluate its correlation with short-term risk of cardiovascular disease (CVD) events and death.
Methods
Single-institution retrospective study including all patients 40–70 years old who underwent NC-NECG-CTT over a period of 6 months. Individuals with known CVD were excluded. The presence of CAC was assessed and quantified by the Agatston score (CACS). CAC severity was defined as mild (< 100), moderate (100–400), or severe (> 400). CVD events (including CVD death, myocardial infarction, revascularisation procedures, ischaemic stroke, acute peripheral atherosclerotic ischaemia), and all-cause mortality over a median of 3.5 years were recorded. Cox proportional-hazards regression modelling was performed including CACS, age, gender and CVD risk factors (smoking, hypertension, diabetes mellitus, dyslipidaemia, and family history of CVD).
Results
Of the total 717 eligible cases, 325 (45%) had CAC. In patients without CAC, there was only one CVD event, compared to 26 CVD events including 5 deaths in patients with CAC. The presence and severity of CAC correlated with CVD events (p < 0.001). A CACS > 100 was significantly associated with both CVD events, hazard ratio (HR) 5.74, 95% confidence interval: 2.19–15.02; p < 0.001, and all-cause mortality, HR 1.7, 95% CI: 1.08–2.66; p = 0.02. Ever-smokers with CAC had a significantly higher risk for all-cause mortality compared to never-smokers (p = 0.03), but smoking status was not an independent predictor for CVD events in any subgroup category of CAC severity.
Conclusions
The presence and severity of CAC assessed on NC-NECG-CTT correlates with short-term cardiovascular events and death.
Key Points
• Patients aged 40–70 years old without known CVD but with CAC on NC-NECG-CTT have a higher risk of CVD events compared to those without CAC.
• CAC (Agatston) score above 100 confers a 5.7-fold increase in the risk of short-term CVD events in these patients.
• The presence and severity of CAC on NC-NECG-CTT may have prognostic and therapeutic implications.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cardiovascular disease (CVD) is the most common cause of death worldwide, with one-third of events occurring in people younger than 70 years [1]. Coronary artery disease (CAD)–related deaths are increasing and are predicted to account for 23.6 million deaths globally by 2030 [2]. Coronary artery calcification (CAC) is a marker of coronary atherosclerosis, strongly associated with major CVD events in asymptomatic individuals [3]. CAC reflects the cumulative lifetime effect of genetic and environmental factors, leading to coronary atherosclerosis [3, 4]. Recent American and European guidelines advise a class II recommendation for CAC testing by computerised tomography (CT) among individuals in whom a risk score–based treatment decision is unclear [5, 6]. The 2021 guidelines also state a class I recommendation that all patients with chronic obstructive pulmonary disease are investigated for atherosclerotic CVD (ASCVD) and ASCVD risk factors [6].
Although CAC scoring (CACS) is the best-established imaging test for CVD risk stratification, there are concerns regarding the availability and cost-effectiveness of systematic screening with ECG-gated CAC scanning [6]. However, every thoracic CT (CTT) can be used to assess CAC and can facilitate opportunistic screening with the advantage of no additional cost. The Society of Cardiovascular Computed Tomography (SCCT)/Society of Thoracic Radiology guidelines provide a class I indication for evaluation and reporting of CAC on all non-contrast chest CT examinations [7]. Non-gated CT scans allow for either semiquantitative or quantitative CACS, with a high correlation to gated CT studies [3]. An important barrier to the adoption of CAC reporting and quantification on non-gated chest CT studies remains the lack of validation with patient outcomes and the negligible impact that reporting incidental CAC has on clinical management decisions [8, 9]. While CAC based on gated cardiac CT is part of CAD work-up usually solicited by cardiology, clinicians referring for CTT may not recognise the importance of this finding. Extensive data is available from lung cancer screening (LCS) studies [10,11,12,13], which only include patients with a history of smoking. Very few studies have assessed the prognostic implication of CAC identified on routine, clinically indicated thoracic CT in unselected populations [14,15,16], with limitations regarding the availability of clinical data related to risk factors, detailed CVD-events or cause of death.
We hypothesised that the CAC burden on non-contrast non-ECG gated CTT (NC-NECG-CTT) in a middle-aged clinical population is associated with short-term adverse outcomes beyond traditional cardiovascular risk factors. The purpose of our study was to detect and quantify CAC on NC-NECG-CTT and collate associated short-term all-cause mortality and CVD events, including CVD-specific death. Additionally, we compared the risk of CVD events and death in smokers compared to never-smokers in patients with CAC.
Materials and methods
Study design and population
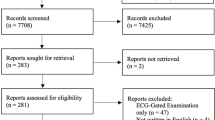
This single-centre retrospective observational study included all consecutive patients aged 40–70 years who underwent NC-NECG-CTT between April and September 2018. Patients with known CVD were excluded. For each patient, only the first scan during the study period was analysed. Figure 1 displays a detailed flowchart of the study population.
Flowchart of the study cohort and overview of events. *Excluded for history of CVD: 2 $MI—myocardial infarction, 4 coronary artery bypass graft (CABG), 29 percutaneous coronary intervention (PCI), 2 cardiac valve interventions, 2 known ischaemic heart disease, 2 ischaemic stroke; aInterstitial lung disease, pulmonary haemorrhage, chronic obstructive pulmonary disease, asthma, cystic lung disease, bronchiectasis, cause for persistent cough, recurrent infection, shortness of breath; bSuspected lung cancer, completion staging from extrathoracic malignancy; cIncluding tuberculosis, atypical/fungal, allergic bronchopulmonary aspergillosis, assessment of response to antibiotics, prior to organ transplant; dLung volume reduction surgery, endobronchial valves, recurrent pneumothorax, foreign body and non-major trauma; e5 PCI and 3 CABG; fTAVI—transcatheter aortic valve implantation
Ethical committee approval and written informed consent were waived because this was a retrospective service evaluation study registered with the institutional Quality and Safety Information System (ID 3329 with registration number PRN9329), with board approval to publish obtained in March 2022.
Imaging methods
The NC-NECG-CTT scans were performed on one of five thin-section CT scanners (four Siemens Definition AS and a Somatom Definition Flash Dual Source, Siemens Healthineers) using volumetric acquisition from lung apices to the diaphragm with breath-hold at the end of deep inspiration. The scan parameters for the protocol used included 0.6 mm collimation, 1.3 pitch, 0.5 s/rotation, 300–409 mm field of view and 512 × 512 matrix, 120 [120–130] kV and mA adjusted according to patient habitus. All examinations were reconstructed as contiguous slices with a thickness of 1 mm, by means of iterative reconstruction (SAFIRE strength level 3).
Data analysis
From our hospital electronic records and linked primary care practitioner (GP) electronic records, we documented patient demographics including age, gender and ethnicity. The notes were manually searched for the presence of CAD risk factors that included smoking status (defined as never-smoker or ever-smoker, the latter including current or former smoker), established diagnosis of hypertension, diabetes mellitus, dyslipidaemia and positive family history of coronary artery disease (CAD). The use of lipid-lowering therapy as well as the commencement of such treatment relative to the date of the NC-NECG-CTT exam was recorded.
CAC was defined as calcification along the course of the coronary arteries and was quantified using the Agatston method [17]. The presence and quantification of CAC were automatically assessed on the mediastinal window reconstruction using the calcium score package of Syngo.via software 7.3 (Siemens Healthineers) and manually corrected by a cardiothoracic radiologist, holder of the European Board of Cardiovascular Radiology Diploma, with 7 years of reporting experience, blinded to patient data. The cohort was divided into patients with and without CAC. In patients with CAC, calcium score was used to define three severity levels: < 100 mild, 100–400 moderate and > 400 severe, as previously described [4, 18].
Follow-up commenced at the time of the CT scan and continued until death, loss to follow-up, or last check of the hospital/GP records in December 2021. We analysed two separate endpoints of adverse outcomes: (1) Major events were defined as fatal and non-fatal CVD including CAD events (MI, CABG or PCI), ischaemic stroke, acute peripheral atherosclerotic ischaemia, and all-cause mortality; (2) Minor events were defined as presentation to the emergency department or referral to cardiology for chest pain, and/or dedicated cardiac imaging (anatomical or functional) for suspected CAD, without a record of a major event.
Statistical analysis was performed using R statistical software version 4.0.5 (R Foundation). The baseline characteristics of patients are presented as absolute numbers and percentages for categorical variables, and median and interquartile range (IQR) for continuous variables. Chi-square and Wilcoxon rank-sum tests were used for comparing categorical or continuous variables, respectively, between the two main groups (with and without CAC) and for the subgroups of ever- and never-smoker with CAC. CACS was tested as an ordinal categorical variable, and binary using cut-offs 0 and 100. Cox proportional hazards models with hazard ratios (HRs) and 95% confidence intervals (CIs) were fitted to test CACS as a predictor of major adverse outcomes. HRs were calculated to assess the prognostic value of smoking status stratified by CACS severity, where patients with missing smoking status were excluded. Incidence of CAD, CVD, all-cause mortality and all major events were evaluated as separate outcomes. Multivariate models were adjusted for age-related risk (M: ≥ 45 y, F: ≥ 55 y) and a number of other known CVD risk factors. Univariate relative risk (RR) of CAC was calculated for a composite end-point of minor events and CVD events. All tests were 2-sided, with a significance level of 0.05.
Results
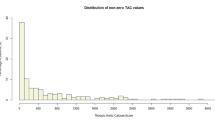
In the final study cohort of 717 cases (Fig. 1), 325 (45%) patients had CAC above 0: 161 mild, 92 moderate, and 72 severe. Detailed baseline characteristics of the main groups and smoking subgroups with CAC are presented in Table 1 and 2, respectively. CACS in ever-smokers was > 50% higher compared to never-smokers, p = 0.04. We observed that 60% of those with CACS = 0 and 63% of those with CACS > 0 had 1–2 CAD risk factors at baseline (p = 0.39).
Outcomes
Major events
Follow-up extended for a median [IQR] of 41.6 [39.8–43.2] months. In patients with CAC, there were 26 CVD events including 5 CVD-related deaths; a case example is presented in Fig. 2. Details on the type of events are presented in Fig. 1. In patients without CAC, there was only one CVD event. The detailed cause of death for the 48 and respectively 49 events recorded in each group respectively are presented in Supplementary Material Table 1.
a High-resolution non-contrast non-ECG gated CT thorax (mediastinal window) of a 55-year-old male patient showing coronary artery calcification in the proximal left anterior descending (LAD) and right coronary arteries (RCA). b The same study demonstrating the calcified plaque within LAD (yellow) and RCA (red) as highlighted on the CT CaScoring on Syngo.via software together with the automatically generated table with per-vessel and total Agatston score. c In this case, the coronary artery calcification had moderate severity and placed the patient close to the 90th percentile for matched age and gender as demonstrated by the automatically generated CT CaScoring percentile chart (Raggi, Circulation 2001). d Coronary angiography shows angiographically significant stenosis in the proximal LAD and a large obtuse marginal branch. e Chest radiograph showing LAD stent placed following myocardial infarction, three months after the reference CT
Table 3 provides the univariate and multivariate HRs for all major events, CVD events and all-cause mortality for the presence of CAC and for each CAC severity subgroup. The presence and each severity level of CAC were independent predictors of CVD events. There was a stepwise increase in CVD events by CAC severity compared with CACS = 0. This was valid both for the multivariate model including the number of CVD risk factors as variable and for the model including each CVD risk factor as separate variables (Supplementary Material Table 2). The unadjusted Kaplan–Meier event-free curves for each CAC severity category and event type are displayed in Fig. 3 and show that the presence and severity of CAC significantly impact event-free progression. Multivariate analysis with CAC as ordinal severity categories showed CAC was an independent predictor for all events (HR 1.29, 95% CI: 1.08–1.54; p = 0.006), CAD (HR 2.77, 95% CI: 1.67–4.62; p < 0.001) and CVD (HR 2.54, 95% CI: 1.68–3.85; p < 0.001), but not for all-cause mortality (HR 1.17, 95% CI: 0.96–1.43; p = 0.11).
In patients with CAC, univariate analysis revealed a significant increase in all major events (p = 0.03) and all-cause mortality (p = 0.04) in ever-smokers compared to never-smokers, but not for CAD or CVD events. No significant difference was found between ever- and never-smokers in any subgroup category of CAC severity either by univariate or multivariate analysis. Detailed results are presented in Table 4.
Minor events
In patients with CAC and no major events, there were 21 minor events: 13 in mild CAC, 6 in moderate CAC, 2 in severe CAC, while in patients without CAC, there were 10 minor events. We found that patients with CAC had 4.93 (95% CI: 2.59–9.38; p < 0.001) times the higher cumulative risk of CVD and minor events, compared to those without CAC, with the highest RR in severe CAC 6.43 (95% CI: 3.00–13.8; p < 0.001). Detailed results are presented in Table 5.
Discussion
Coronary artery calcification is a frequent incidental finding in middle-aged adults undergoing clinically-indicated CTT. Our study shows that (1) the presence and severity of CAC assessed on NC-NECG-CTT correlates with short-term CVD events and death; (2) ever-smokers have significantly higher CAC compared to never-smokers with significantly higher risk for all-cause mortality, but the similar risk for CVD events within each CAC severity category, and (3) the presence of CAC is significantly associated with a presentation to emergency or cardiology departments with anginal symptoms and further cardiac imaging. To our knowledge, this is the first study analysing clinically-indicated CTTs to explore the correlation of CACS with adverse cardiovascular events beyond traditional cardiovascular risk factors and beyond all-cause mortality. In this setup, it is the first study investigating the prognostic value of CACS cut-off 100 for CVD events and death.
We based our analysis on the well-established CAC quantification using the Agatston score. Excellent correlation has been demonstrated between CAC identified on NECG-CTT and Agatston’s scores obtained from gated-CT scans with a pooled correlation coefficient of 0.94 (95% CI, 0.89–0.97) and very low false negative rate (8.8%) [10]. Very good agreement has been reported between the Agatston score and visual assessment or ordinal scores [11, 19,20,21].
CACS has been extensively studied in the context of LCS [11,12,13, 21,22,23], and the severity of CAC on LCS CTs correlates with subsequent major adverse cardiac events, including CVD mortality [11,12,13]. Although we observed a lower number of incident events due to differences in cohort characteristics and size, our results are comparable with previously reported data from LCS showing increasing HRs with increasing CACS [7]. In 1442 patients in the National Lung Screening Trial, compared to Agatston scores of 0, scores of 1–100, 101–1000, and > 1000 had HR for CAD death of 1.27 (95% CI: 0.69–2.53), 3.57 (95% CI: 2.14–7.48), and 6.63 (95% CI: 3.57–14.97), respectively [11]. Our results from clinically-indicated CTT showed that the presence of CAC predicts CVD, with incremental risk in proportion to CAC severity when adjusting for cardiovascular risk factors. We found a significant association of CACS > 100 with all major events, all-cause mortality, CAD and CVD events in both unadjusted and multivariate-adjusted analyses. The adjusted HR for CVD events among those with CACS > 100 was 5.74 (95% CI: 2.19–15.02; p < 0.001). In a similar setup using CAC assessed by ordinal score, the risk of any CVD event (fatal and non-fatal) was increased by a factor of 2.2 (95% CI: 1.6–3.0) in mild, 2.5 (95% CI: 1.8–3.4) in moderate and 3.7 (95% CI: 2.7–5.2) in severe CAC compared with no CAC [14]. This study did not adjust for cardiovascular risk factors. In a study assessing the prognostic value of CAC for a composite end-point of all-cause mortality or non-fatal MI, an HR of 2.6 (95% CI: 1.0–6.4; p = 0.04) for CACS 1–500 and 5.3 (95% CI: 1.9–14.2; p < 0.001) for CACS > 500, compared to no CAC, was found adjusting for age, sex, and diabetes [15].
The presence of CAC and higher CAC score among smokers is associated with higher CVD, CAD, and all-cause mortality, particularly in CACS > 400 where CVD mortality is 3.5-fold and CAD is 8.8-fold higher compared to CACS = 0 [24]. However, we found no significant statistical difference in incident events in ever-smokers and never-smokers within each CAC severity subgroup suggesting CAC as a stronger predictor of adverse events and supporting the use of CAC scoring for CAD risk stratification in smokers.
The addition of CAC to the assessment of traditional risk factors should aid patient reclassification into more accurate risk groups, resulting in incremental clinical benefit through a change in patient behaviour and clinical management [3]. In a meta-analysis of 11,256 participants followed over 1.6–6 years, Gupta et al demonstrated significantly higher use of aspirin, lipid-lowering medication, antihypertensive medication, exercise, and dietary change in individuals with CACS > 0 compared to those with CACS = 0 [25]. In 950 individuals who met inclusion criteria for the use of statins in a preventive interventional clinical trial, the 5-year Number Needed to Treat (NNT) to prevent one CVD event varied from 124 for individuals with CACS = 0, to just 19 for those with CACS > 100 [26]. Similarly, the 10-year NNT to reduce ASCVD events by aggressive blood pressure regulation in patients with an intermediate risk of CAD and prehypertension or mild hypertension correlates to baseline CAC status, from 99 for CACS = 0 to only 24 for CACS > 100 [27]. The SCCT recommends prophylactic daily aspirin in those with CACS > 100, with studies showing a net benefit of aspirin therapy, regardless of risk factors in these cases [28, 29]. There remains a lack of clarity in therapeutic recommendations for Agatston CACS between 0 and 100; however, it may be prudent to initiate statin therapy in presence of any CAC [30].
In our cohort, 60% of patients with and without CAC had 1–2 CAD risk factors at baseline, which reflects the real-world challenge of identifying patients who would most benefit from lipid-lowering therapy based on CAD risk factor estimates alone. Furthermore, less than a quarter of patients with CAC (including only 27% of ever-smokers) were taking statins at baseline indicating the potential benefit to a large majority of patients who would receive guideline-recommended therapy as a result of incidental identification of CAC on NC-NECG-CTT.
The SCCT recommends CAC testing within the context of shared decision-making for asymptomatic individuals aged 40–75 years without clinical ASCVD when the 10-year ASCVD calculated risk is < 20% [3, 7]. Individuals with CAC confirmed on CT scans performed for another indication may not need another CT for a CAC score [31]. Furthermore, the severity of CAC on NECG-CTT may guide the decision on future cardiac imaging either with coronary CT angiography or alternative tests. A recent study showed that CACS > 400 was the most prominent predictor of obstructive CAD and higher benefit from alternative tests [32]. Finally, NC-NECG-CCT could allow for the assessment of CAC progression in patients requiring multiple scans over several years. It has been shown that a repeat CAC scan after 5 years would be of additional value, except for those already classified as high risk due to a CACS > 400 [33].
Reporting CAC on NECG-CTT caters to a larger population than through gated CT alone, prompting further investigation, leading to earlier identification and modification of risk factors, earlier intervention and improved outcomes for patients; ultimately these could represent financial savings for national health systems in the longer term [34]. However, routine reporting of CAC will increase the demand on clinicians, requiring the implementation of a dedicated care pathway for high-risk patients. Additional training would be required to initiate CAC reporting, and adoption of standardised templates and protocols would help promote reporting and referral to appropriate services [30, 35]. No additional equipment or funding would be necessary to undertake CACS, although it would require additional reporting time for radiologists. Artificial intelligence may prove useful both for the implementation of routine reporting and for retrospective analysis of large datasets.
Our study has several limitations. Due to the retrospective nature, the data gathered, especially regarding family history, was limited by the quality of available records. Nevertheless, the study cohort represents a random sample of the routine clinical population and avoids cardiac-specific referral bias which is a recognised limitation in most ECG-gated CAC CT studies. CAC on NC-NECG-CTT is generally under-reported [9, 36]. We recognise its reporting might have led to risk factor modification and therapeutic intervention in a limited number of cases. During the SARS-CoV-2 pandemic, many elective procedures were postponed, thereby underestimating the number of events under normal circumstances. Additionally, the CAC severity subgroup analysis was underpowered. Our study was limited to a single centre, in a predominantly Caucasian population of middle-aged adults, therefore extrapolation to other demographic groups may be difficult. However, previous studies have shown that the incremental risk-predictive value of CAC can be extended to both young and elderly individuals [31, 37]. Lastly, we did not analyse the anatomical distribution of CAC after considering the potential impact of such detailed reporting in clinical practice, both in terms of time and adoption, particularly by non-cardiothoracic radiologists. The number of coronary arteries with CAC and the presence of CAC in the proximal dominant coronary artery are significantly associated with major CAD events after adjusting for risk factors and severity of the Agatston score [38].
In conclusion, we have confirmed that CAC on routine clinically-indicated CT thorax can be used to identify those at greater risk of future CVD events. Our findings support the current guidelines recommending reporting of CAC on all thoracic CTs, to facilitate adequate risk modification and preventive treatment.
Abbreviations
- ASCVD:
-
Atherosclerotic cardiovascular disease
- CABG:
-
Coronary artery bypass graft
- CAC:
-
Coronary artery calcification
- CACS:
-
Coronary artery calcification scoring
- CAD:
-
Coronary artery disease
- CI:
-
Confidence interval
- CVD:
-
Cardiovascular disease
- GP:
-
Primary care practitioner
- HR:
-
Hazard ratio
- IQR:
-
Interquartile range
- LCS:
-
Lung cancer screening
- MI:
-
Myocardial infarction
- NC-NECG-CTT:
-
Non-contrast non-ECG gated CT thorax
- NNT:
-
Number needed to treat
- PCI:
-
Percutaneous coronary intervention
- RR:
-
Relative risk
- SCCT:
-
The Society of Cardiovascular Computed Tomography
References
World Health Organization (2021) Cardiovascular diseases (CVDs). https://www.who.int/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds). Accessed 27 Nov 2021
Chi JM, Makaryus JN, Rahmani N et al (2021) Coronary CT calcium score in patients with prior nongated CT, is it necessary? Curr Probl Diagn Radiol 50:54–58. https://doi.org/10.1067/j.cpradiol.2019.07.011
Greenland P, Blaha MJ, Budoff MJ et al (2018) Coronary calcium score and cardiovascular risk. J Am Coll Cardiol 72:434–447
Grandhi GR, Mirbolouk M, Dardari ZA et al (2020) Interplay of coronary artery calcium and risk factors for predicting CVD/CHD mortality: the CAC consortium. JACC Cardiovasc Imaging 13:1175–1186. https://doi.org/10.1016/j.jcmg.2019.08.024
Grundy SM, Stone NJ, Bailey AL et al (2019) 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol. J Am Coll Cardiol 73:e285–e350. https://doi.org/10.1016/j.jacc.2018.11.003
Visseren FLJ, Mach F, Smulders YM et al (2021) 2021 ESC GUIDELINES on cardiovascular disease prevention in clinical practice. Eur Heart J 42:3227–3337. https://doi.org/10.1093/eurheartj/ehab484
Hecht HS, Cronin P, Blaha MJ et al (2017) 2016 SCCT/STR guidelines for coronary artery calcium scoring of noncontrast noncardiac chest CT scans: a report of the Society of Cardiovascular Computed Tomography and Society of Thoracic Radiology. J Cardiovasc Comput Tomogr 11:74–84. https://doi.org/10.1016/j.jcct.2016.11.003
Dzaye O, Dudum R, Mirbolouk M et al (2020) Validation of the coronary artery calcium data and reporting system (CAC-DRS): dual importance of CAC score and CAC distribution from the Coronary Artery Calcium (CAC) consortium. J Cardiovasc Comput Tomogr 14:12–17. https://doi.org/10.1016/j.jcct.2019.03.011
Uretsky S, Chokshi N, Kobrinski T et al (2015) The interplay of physician awareness and reporting of incidentally found coronary artery calcium on the clinical management of patients who underwent noncontrast chest computed tomography. Am J Cardiol 115:1513–1517. https://doi.org/10.1016/j.amjcard.2015.02.051
Xie X, Zhao Y, de Bock GH et al (2013) Validation and prognosis of coronary artery calcium scoring in nontriggered thoracic computed tomography. Circ Cardiovasc Imaging 6:514–521. https://doi.org/10.1161/CIRCIMAGING.113.000092
Chiles C, Duan F, Gladish GW et al (2015) Association of coronary artery calcification and mortality in the national lung screening trial: a comparison of three scoring methods. Radiology 276:82–90. https://doi.org/10.1148/radiol.15142062
Shemesh J, Henschke CI, Shaham D et al (2010) Ordinal scoring of coronary artery calcifications on low-dose CT scans of the chest is predictive of death from cardiovascular disease. Radiology 257:541–548. https://doi.org/10.1148/radiol.10100383
Jacobs PC, Gondrie MJA, van der Graaf Y et al (2012) Coronary artery calcium can predict all-cause mortality and cardiovascular events on low-dose CT screening for lung cancer. AJR Am J Roentgenol 198:505–511. https://doi.org/10.2214/AJR.10.5577
Jacobs PC, Gondrie MJ, Mali WP et al (2011) Unrequested information from routine diagnostic chest CT predicts future cardiovascular events. Eur Radiol 21:1577–1585. https://doi.org/10.1007/s00330-011-2112-8
Shao L, Yan AT, Lebovic G et al (2017) Prognostic value of visually detected coronary artery calcification on unenhanced non-gated thoracic computed tomography for prediction of non-fatal myocardial infarction and all-cause mortality. J Cardiovasc Comput Tomogr 11:196–202. https://doi.org/10.1016/j.jcct.2017.03.004
Rodriguez-Granillo GA, Reynoso E, Capunay C et al (2017) Impact on mortality of coronary and non-coronary cardiovascular findings in non-gated thoracic CT by malignancy status. Eur J Radiol 93:169–177. https://doi.org/10.1016/j.ejrad.2017.05.030
Agatston AS, Janowitz WR, Hildner FJ et al (1990) Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol 15:827–832. https://doi.org/10.1016/0735-1097(90)90282-T
Greenland P, Bonow RO, Brundage BH et al (2007) ACCF/AHA 2007 clinical expert consensus document on coronary artery calcium scoring by computed tomography in global cardiovascular risk assessment and in evaluation of patients with chest pain. J Am Coll Cardiol 49:378–402. https://doi.org/10.1016/j.jacc.2006.10.001
Azour L, Kadoch MA, Ward TJ et al (2017) Estimation of cardiovascular risk on routine chest CT: ordinal coronary artery calcium scoring as an accurate predictor of Agatston score ranges. J Cardiovasc Comput Tomogr 11:8–15. https://doi.org/10.1016/j.jcct.2016.10.001
Blair KJ, Allison MA, Morgan C et al (2014) Comparison of ordinal versus Agatston coronary calcification scoring for cardiovascular disease mortality in community-living individuals. Int J Cardiovasc Imaging 30:813–818. https://doi.org/10.1007/s10554-014-0392-1
Huang Y-L, Wu F-Z, Wang Y-C et al (2013) Reliable categorisation of visual scoring of coronary artery calcification on low-dose CT for lung cancer screening: validation with the standard Agatston score. Eur Radiol 23:1226–1233. https://doi.org/10.1007/s00330-012-2726-5
Suh YJ, Lee JW, Shin SY et al (2020) Coronary artery calcium severity grading on non-ECG-gated low-dose chest computed tomography: a multiple-observer study in a nationwide lung cancer screening registry. Eur Radiol 30:3684–3691. https://doi.org/10.1007/s00330-020-06707-x
Zhu Y, Yip R, Shemesh J et al (2020) Combined aortic valve and coronary artery calcifications in lung cancer screening as predictors of death from cardiovascular disease. Eur Radiol 30:6847–6857. https://doi.org/10.1007/s00330-020-07049-4
Mirbolouk M, Kianoush S, Dardari Z et al (2020) The association of coronary artery calcium score and mortality risk among smokers: the coronary artery calcium consortium. Atherosclerosis 294:33–40. https://doi.org/10.1016/j.atherosclerosis.2019.12.014
Gupta A, Lau E, Varshney R et al (2017) The identification of calcified coronary plaque is associated with initiation and continuation of pharmacological and lifestyle preventive therapies. JACC Cardiovasc Imaging 10:833–842. https://doi.org/10.1016/j.jcmg.2017.01.030
Blaha MJ, Budoff MJ, DeFilippis AP et al (2011) Associations between C-reactive protein, coronary artery calcium, and cardiovascular events: implications for the JUPITER population from MESA, a population-based cohort study. Lancet 378:684–692. https://doi.org/10.1016/S0140-6736(11)60784-8
McEvoy JW, Martin SS, Dardari ZA et al (2017) Coronary artery calcium to guide a personalized risk-based approach to initiation and intensification of antihypertensive therapy. Circulation 135:153–165. https://doi.org/10.1161/CIRCULATIONAHA.116.025471
Miedema MD, Duprez DA, Misialek JR et al (2014) Use of coronary artery calcium testing to guide aspirin utilization for primary prevention: estimates from the multi-ethnic study of atherosclerosis. Circ Cardiovasc Qual Outcomes 7:453–460. https://doi.org/10.1161/CIRCOUTCOMES.113.000690
Hecht H, Blaha MJ, Berman DS et al (2017) Clinical indications for coronary artery calcium scoring in asymptomatic patients: expert consensus statement from the Society of Cardiovascular Computed Tomography. J Cardiovasc Comput Tomogr 11:157–168. https://doi.org/10.1016/j.jcct.2017.02.010
Hecht HS, Blaha MJ, Kazerooni EA et al (2018) CAC-DRS: coronary artery calcium data and reporting system. An expert consensus document of the Society of Cardiovascular Computed Tomography (SCCT). J Cardiovasc Comput Tomogr 12:185–191. https://doi.org/10.1016/j.jcct.2018.03.008
Carr JJ, Jacobs DR, Terry JG et al (2017) Association of coronary artery calcium in adults aged 32 to 46 years with incident coronary heart disease and death. JAMA Cardiol 2:391–399. https://doi.org/10.1001/jamacardio.2016.5493
Simon J, Száraz L, Szilveszter B et al (2020) Calcium scoring: a personalized probability assessment predicts the need for additional or alternative testing to coronary CT angiography. Eur Radiol 30:5499–5506. https://doi.org/10.1007/s00330-020-06921-7
Lehmann N, Erbel R, Mahabadi AA et al (2018) Value of progression of coronary artery calcification for risk prediction of coronary and cardiovascular events. Circulation 137:665–679. https://doi.org/10.1161/CIRCULATIONAHA.116.027034
Public Health England (2019) Health matters: preventing cardiovascular disease. https://www.gov.uk/government/publications/health-matters-preventing-cardiovascular-disease/health-matters-preventing-cardiovascular-disease. Accessed 1 Mar 2022
Williams MC, Abbas A, Tirr E et al (2021) Reporting incidental coronary, aortic valve and cardiac calcification on non-gated thoracic computed tomography, a consensus statement from the BSCI/BSCCT and BSTI. Br J Radiol 94:20200894. https://doi.org/10.1259/bjr.20200894
Williams KA, Kim JT, Holohan KM (2013) Frequency of unrecognized, unreported, or underreported coronary artery and cardiovascular calcification on noncardiac chest CT. J Cardiovasc Comput Tomogr 7:167–172. https://doi.org/10.1016/j.jcct.2013.05.003
Yano Y, O’Donnell CJ, Kuller L et al (2017) Association of coronary artery calcium score vs age with cardiovascular risk in older adults: an analysis of pooled population-based studies. JAMA Cardiol 2:986–994. https://doi.org/10.1001/jamacardio.2017.2498
Ferencik M, Pencina KM, Liu T et al (2017) Coronary artery calcium distribution is an independent predictor of incident major coronary heart disease events. Circ Cardiovasc Imaging 10:e006592. https://doi.org/10.1161/CIRCIMAGING.117.006592
Funding
The authors state that this work has not received any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Dr Unni Krishnan.
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was not required for this study because this was a retrospective service evaluation study.
Ethical approval
Institutional Review Board approval was not required because the project was registered with the institutional Quality and Safety Information System as service evaluation project ID 3329 with registration number PRN9329 with consent to publish obtained in March 2022.
Study subjects or cohorts overlap
Some study subjects have been previously reported in EPOS: ECR 2020 / C-14385 and ESCR 2019 / P-0023.
Methodology
• retrospective
• diagnostic or prognostic study / observational
• performed at one institution
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wetscherek, M.T.A., McNaughton, E., Majcher, V. et al. Incidental coronary artery calcification on non-gated CT thorax correlates with risk of cardiovascular events and death. Eur Radiol 33, 4723–4733 (2023). https://doi.org/10.1007/s00330-023-09428-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-023-09428-z