Abstract
Objectives
The purpose of this study was to leverage a magnetic resonance imaging (MRI) approach to characterize foot perfusion distribution in patients with diabetes, with or without foot ulcers, and determine the ability of the regional perfusion measurements to identify ulcer-healing status.
Methods
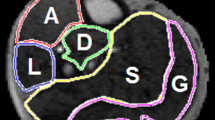
Three groups of participants (n = 15 / group) were recruited: controls (without diabetes), type II diabetes, and type II diabetes with foot ulcers. All participants underwent MRI evaluating foot perfusion in three muscle layers (from plantar to dorsal) at rest and during a standardized toe-flexion exercise. The exercise perfusion and perfusion reserve values were analyzed around and away from ulcers. Participants with foot ulcers were followed up 3 months after the MRI exams to determine the foot healing status.
Results
Foot plantar muscle perfusion reserves were progressively lower from controls to diabetes, and to diabetes with foot ulcers (e.g., 2.58 ± 0.67, 1.48 ± 0.71, 1.12 ± 0.35, p < 0.001). In controls, the plantar layer had significantly higher perfusion reserve than the dorsal layer, whereas in either diabetes group, there was no significant difference in perfusion reserve among muscle layers. Using the ratio of total exercise perfusion around ulcers to that away from ulcers, the sensitivity and specificity to differentiate healing from non-healed ulcers were 100% and 86%, respectively.
Conclusions
Our study reveals significantly different foot perfusion distribution among controls, diabetes, and diabetes with foot ulcers. The prognostic value of MRI regional perfusion assessments has the potential to monitor interventions to improve ulcer healing outcomes.
Key Points
• Contrast-free MRI permits quantitative assessment of regional foot muscle perfusion at rest and during isometric exercise.
• Patients with diabetes and foot ulcers, without clinical evidence of peripheral arterial disease, had significantly impaired foot muscle perfusion and perfusion reserve.
• Regional foot perfusion distribution may be used to predict the short-term healing status of foot ulcers in diabetes.


Similar content being viewed by others
Data Availability
The datasets generated and analyzed during the current study are available from the corresponding author upon reasonable request.
Abbreviations
- ABI:
-
Ankle-brachial index
- AUC:
-
Area under the ROC Curve
- DFU:
-
Diabetic foot ulcer
- DM:
-
Diabetes mellitus
- MRI:
-
Magnetic resonance imaging
- PAD:
-
Peripheral arterial disease
- ROC:
-
Receiver operating characteristic
- SMBF:
-
Skeletal muscle blood flow
- TBI:
-
Toe-brachial index
- TcPO2 :
-
Transcutaneous oximetry
References
Boulton AJ, Vileikyte L, Ragnarson-Tennvall G, Apelqvist J (2005) The global burden of diabetic foot disease. Lancet 366:1719–1724
Apelqvist J, Bakker K, van Houtum WH, Nabuurs-Franssen MH, Schaper NC (2000) International consensus and practical guidelines on the management and the prevention of the diabetic foot. International Working Group on the Diabetic Foot. Diabetes Metab Res Rev 16 (Suppl 1):S84–92
Pecoraro RE, Reiber GE, Burgess EM (1990) Pathways to diabetic limb amputation. Basis for prevention. Diabetes Care 13:513–521
American Diabetes Association (1999) Consensus Development Conference on Diabetic Foot Wound Care: 7–8 April 1999, Boston, Massachusetts. Diabetes Care 22:1354–1360
Edmonds ME, Foster AV (2006) Diabetic foot ulcers. BMJ 332(7538):407–410
Gershater MA, Löndahl M, Nyberg P et al (2009) Complexity of factors related to outcome of neuropathic and neuroischaemic/ischaemic diabetic foot ulcers: a cohort study. Diabetologia 52:398–407
Grunfeld C (1992) Diabetic foot ulcers: etiology, treatment and prevention. Adv Intern Med 37:103–132
Edmonds ME, Foster AVM (2005) Managing the diabetic foot, 2nd ed. Wiley-Blackwell, Hoboken, NJ
Casey SL, Lanting SM, Chuter VH (2020) The ankle brachial index in people with and without diabetes: intra-tester reliability. J Foot Ankle Res 13:21
Wang Z, Hasan R, Firwana B et al (2016) A systematic review and meta-analysis of tests to predict wound healing in diabetic foot. J Vasc Surg 63:29S-36S
Brownrigg JR, Hinchliffe RJ, Apelqvist J et al (2016) International Working Group on the Diabetic Foot. Performance of prognostic markers in the prediction of wound healing or amputation among patients with foot ulcers in diabetes: a systematic review. Diabetes Metab Res Rev 32 Suppl 1:128–135
Jung DY, Kim MH, Koh EK, Kwon OY, Cynn HS, Lee WH (2011) A comparison in the muscle activity of the abductor hallucis and the medial longitudinal arch angle during toe curl and short foot exercises. Phys Ther Sport 12:30–35
Kurihara T, Yamauchi J, Otsuka M, Tottori N, Hashimoto T, Isaka T (2014) Maximum toe flexor muscle strength and quantitative analysis of human plantar intrinsic and extrinsic muscles by a magnetic resonance imaging technique. J Foot Ankle Res 7:26
Błażkiewicz M, Sundar L, Healy A, Ramachandran A, Chockalingam N, Naemi R (2015) Assessment of lower leg muscle force distribution during isometric ankle dorsi and plantar flexion in patients with diabetes: a preliminary study. J Diabetes Complications 29:282–287
Chatzistergos PE, Naemi R, Sundar L, Ramachandran A, Chockalingam N (2014) The relationship between the mechanical properties of heel-pad and common clinical measures associated with foot ulcers in patients with diabetes. J Diabetes Complications 28:488–493
Park SC1, Choi CY, Ha YI, Yang HE (2012) Utility of toe-brachial index for diagnosis of peripheral artery disease. Arch Plast Surg 39:227–231
Edalati M, Hastings MK, Muccigrosso D et al (2019) Intravenous contrast-free standardized exercise perfusion imaging in diabetic feet with ulcers. J Magn Reson Imaging 50(2):474–480
Zhang H, Shea SM, Park V et al (2005) Accurate myocardial T1 measurements: toward quantification of myocardial blood flow with arterial spin labeling. Magn Reson Med 53:1135–1142
Zheng J, An H, Coggan AR et al (2014) Non-contrast skeletal muscle oximetry. Magn Reson Med 71:318–325
Zheng J, Hastings MK, Muccigross D et al (2015) Non-contrast MRI perfusion angiosome in diabetic feet. Eur Radiol 25:99–105
Belle V, Kahler E, Waller C et al (1998) In vivo quantitative mapping of cardiac perfusion in rats using a noninvasive MR spin-labeling method. J Magn Reson Imaging 8:1240–1245
Waller C, Kahler E, Hiller KH et al (2000) Myocardial perfusion and intracapillary blood volume in rats at rest and with coronary dilation: MR imaging in vivo with use of spin-labeling technique. Radiology 215:189–197
Look DC, Locker DR (1970) Time saving in measurement of NMR and EPR relaxation times. Rev Sci Instrum 41:250–251
Dipietro L, Caspersen CJ, Ostfeld AM et al (1993) A survey for assessing physical activity among older adults. Med Sci Sports Exerc 25:628–642
Manevska N, Gjorceva DP, Ahmeti I, Todorovska L, Stojanoski S, Kocovska MZ (2016) Tissue-muscle perfusion scintigraphy of the lower limbs in a patient with type 2 diabetes mellitus and peripheral arterial disease. Mol Imaging Radionucl Ther 25:42–46
Sacre JW, Jellis CL, Haluska BA et al (2015) Association of exercise intolerance in type 2 diabetes with skeletal muscle blood flow reserve. JACC Cardiovasc Imaging 8:913–921
Ma J, Lai Z, Shao J et al (2021) Infrapopliteal endovascular intervention and the angiosome concept: intraoperative real-time assessment of foot regions’ blood volume guides and improves direct revascularization. Eur Radiol 31:2144–2152
Kagadis GC, Tsantis S, Gatos I, Spiliopoulos S, Katsanos K, Karnabatidis D (2020) 2D perfusion DSA with an open-source, semi-automated, color-coded software for the quantification of foot perfusion following infrapopliteal angioplasty: a feasibility study. Eur Radiol Exp 4:47
Veit-Haibach P, Huellner MW, Banyai M et al (2021) CT perfusion in peripheral arterial disease-hemodynamic differences before and after revascularisation. Eur Radiol 31:5507–5513
Fronek A, Coel M, Berstein EF (1976) Quantitative ultrasonographic studies of lower extremity flow velocities in health and disease. Circulation 53:957–960
Zhou J, van Zijl PC (1999) Effect of transit times on quantification of cerebral blood flow by the FAIR T(1)-difference approach. Magn Reson Med 42:890–894
Zheng J, Sorensen C, Li R et al (2021) Deteriorated regional calf microcirculation measured by contrast-free MRI in patients with diabetes mellitus and relation with physical activity. Diab Vasc Dis Res 18(4):14791641211029002
Zheng J, Li R, Zayed MA, Yan Y, An H, Hastings MK (2021) Pilot study of contrast free MRI reveals significantly impaired calf skeletal muscle perfusion in diabetes with incompressible peripheral arteries. Vasc Med 26:367–373
Acknowledgements
The authors would like to thank Christopher Sorensen, Darrah Snozek, Katherine Love, and Dakkota Thies for recruiting the study participants.
Funding
This study was supported in part by National Institutes of Health (NIH) research grants R21 AR065672 and R01DK105322.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantors of this publication are Professor Jie Zheng and Professor Mary K. Hastings.
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
Professor Yan Yan has significant statistical expertise and provided all statistical analysis results.
Informed consent
Written informed consent was obtained from all subjects (patients) in this study.
Ethical approval
Institutional Review Board approval was obtained.
Methodology
• prospective
• Observational
• Performed at one institution
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zheng, J., Li, R., Dickey, E.E. et al. Regional skeletal muscle perfusion distribution in diabetic feet may differentiate short-term healed foot ulcers from non-healed ulcers. Eur Radiol 33, 3303–3311 (2023). https://doi.org/10.1007/s00330-023-09405-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-023-09405-6