Abstract
Objectives
To evaluate susceptibility values associated with iron accumulation in the deep gray matter during postnatal development and to compare magnetic susceptibility between patients with normal and delayed development.
Methods
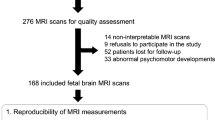
Patients with postmenstrual age (PMA) ≤ 1000 days underwent MR scans between August 2015 and April 2020 at our hospital. Quantitative susceptibility mapping (QSM) was performed, and magnetic susceptibility was measured using three-dimensional volumes of interest (VOIs) for the caudate nucleus (CN), globus pallidus (GP), putamen (PT), and ventrolateral thalamic nucleus (VL). Cross-sectional analysis was performed for 99 patients with normal development and 39 patients with delayed development. Longitudinal analysis was also performed to interpret changes over time in 13 patients with normal development. Correlations between magnetic susceptibility in VOIs and PMA or chronological age (CA) were assessed.
Results
Susceptibility values for CN, GP, PT, and VL showed positive moderate correlations with both PMA (ρ = 0.45, 0.69, 0.62, and 0.33, respectively) and CA (ρ = 0.53, 0.69, 0.66, and 0.39, respectively). The slope of the correlation between susceptibility values and age was highest in the GP among the four gray matter areas. Susceptibility values for the CN, GP, PT, and VL were higher with normal development than with delayed development at early postnatal age, although a significant difference was only observed for the CN. Susceptibility values also increased with age in the longitudinal analysis.
Conclusions
Magnetic susceptibility values in deep gray matter increased with age ≤ 1000 days. The normal development group showed higher susceptibility values than the delayed development group at early postnatal age (PMA ≤ 285 days).
Key Points
• Magnetic susceptibilities in deep gray matter nuclei increased with age (postmenstrual age ≤ 1000 days) in a large number of pediatric patients.
• The normal development group showed higher susceptibility values than the delayed development group in the basal ganglia and ventrolateral thalamic nucleus at early postnatal age (PMA ≤ 285 days).






Similar content being viewed by others
Abbreviations
- CA:
-
Chronological age
- CHARGE syndrome:
-
Coloboma, Heart defects, Atresia choanae, growth Retardation, Genital abnormalities, and Ear abnormalities
- CN:
-
Caudate nucleus
- DARTEL:
-
Diffeomorphic Anatomical Registration Through Exponentiated Lie Algebra
- GA:
-
Gestational age
- GP:
-
Globus pallidus
- KARS:
-
Lysyl-tRNA synthetase
- MNI:
-
Montreal Neurological Institute
- PCYT1A:
-
Phosphate cytidylyltransferase 1A, choline
- PMA:
-
Postmenstrual age
- PT:
-
Putamen
- QSM:
-
Quantitative susceptibility mapping
- VACTERL:
-
Vertebral anomalies, Anorectal malformations, Cardiovascular anomalies, Tracheo-esophageal fistula and Esophageal atresia, Renal anomalies, and Limb defects
- VL:
-
Ventrolateral thalamic nucleus
References
Rogers CE, Lean RE, Wheelock MD, Smyser CD (2018) Aberrant structural and functional connectivity and neurodevelopmental impairment in preterm children. J Neurodev Disord 10:38
Chiarelli AM, Sestieri C, Navarra R, Wise RG, Caulo M (2021) Distinct effects of prematurity on MRI metrics of brain functional connectivity, activity, and structure: univariate and multivariate analyses. Hum Brain Mapp 42:3593–3607
Brody BA, Kinney HC, Kloman AS, Gilles FH (1987) Sequence of central nervous system myelination in human infancy. I. An autopsy study of myelination. J Neuropathol Exp Neurol 46:283–301
Todorich B, Pasquini JM, Garcia CI, Paez PM, Connor JR (2009) Oligodendrocytes and myelination: the role of iron. Glia 57:467–478
Schweser F, Deistung A, Lehr BW, Reichenbach JR (2011) Quantitative imaging of intrinsic magnetic tissue properties using MRI signal phase: an approach to in vivo brain iron metabolism? Neuroimage 54:2789–2807
de Rochefort L, Liu T, Kressler B et al (2010) Quantitative susceptibility map reconstruction from MR phase data using bayesian regularization: validation and application to brain imaging. Magn Reson Med 63:194–206
Li W, Wu B, Liu C (2011) Quantitative susceptibility mapping of human brain reflects spatial variation in tissue composition. Neuroimage 55:1645–1656
Hallgren B, Sourander P (1958) The effect of age on the non-haemin iron in the human brain. J Neurochem 3:41–51
Volpe JJ (2009) Brain injury in premature infants: a complex amalgam of destructive and developmental disturbances. Lancet Neurol 8:110–124
Li W, Wu B, Batrachenko A et al (2014) Differential developmental trajectories of magnetic susceptibility in human brain gray and white matter over the lifespan. Hum Brain Mapp 35:2698–2713
Zhang Y, Shi J, Wei H, Han V, Zhu WZ, Liu C (2019) Neonate and infant brain development from birth to 2 years assessed using MRI-based quantitative susceptibility mapping. Neuroimage 185:349–360
Dubois J, Alison M, Counsell SJ, Hertz-Pannier L, Huppi PS, Benders M (2021) MRI of the neonatal brain: a review of methodological challenges and neuroscientific advances. J Magn Reson Imaging 53:1318–1343
Tortora D, Severino M, Sedlacik J et al (2018) Quantitative susceptibility map analysis in preterm neonates with germinal matrix-intraventricular hemorrhage. J Magn Reson Imaging 48:1199–1207
Tatsuta N, Suzuki K, Sugawara T, Nakai K, Hosokawa T, Satoh H (2013) Comparison of Kyoto Scale of Psychological Development and Bayley Scales of Infant Development second edition among Japanese Infants. J Spec Educ Res 2:17–24
Kono Y, Yonemoto N, Kusuda S et al (2016) Developmental assessment of VLBW infants at 18 months of age: A comparison study between KSPD and Bayley III. Brain Dev 38:377–385
Li W, Avram AV, Wu B, Xiao X, Liu C (2014) Integrated Laplacian-based phase unwrapping and background phase removal for quantitative susceptibility mapping. NMR Biomed 27:219–227
Barkovich AJ (1998) MR of the normal neonatal brain: assessment of deep structures. AJNR Am J Neuroradiol 19:1397–1403
Duff EP, Cunnington R, Egan GF (2007) REX: response exploration for neuroimaging datasets. Neuroinformatics 5:223–234
R Core Team (2021) R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna. https://www.R-project.org/
Bates D, Mächler M, Bolker B, Walker S (2015) Fitting linear mixed-effects models using lme4. J Stat Softw 67(1):1–48. https://doi.org/10.18637/jss.v067.i01
Kuznetsova A, Brockhoff PB, Christensen RHB (2017) lmerTest package: tests in linear mixed effects models. J Stat Softw 82(13):1–26. https://doi.org/10.18637/jss.v082.i13
Zhang Y, Wei H, Cronin MJ, He N, Yan F, Liu C (2018) Longitudinal atlas for normative human brain development and aging over the lifespan using quantitative susceptibility mapping. Neuroimage 171:176–189
Ning N, Liu C, Wu P et al (2019) Spatiotemporal variations of magnetic susceptibility in the deep gray matter nuclei from 1 month to 6 years: a quantitative susceptibility mapping study. J Magn Reson Imaging 49:1600–1609
Siddappa AM, Rao R, Long JD, Widness JA, Georgieff MK (2007) The assessment of newborn iron stores at birth: a review of the literature and standards for ferritin concentrations. Neonatology 92:73–82
Schneider N, Garcia-Rodenas CL (2017) Early nutritional interventions for brain and cognitive development in preterm infants: a review of the literature. Nutrients 9:187
Hasegawa M, Houdou S, Mito T, Takashima S, Asanuma K, Ohno T (1992) Development of myelination in the human fetal and infant cerebrum: a myelin basic protein immunohistochemical study. Brain Dev 14:1–6
Counsell SJ, Maalouf EF, Fletcher AM et al (2002) MR imaging assessment of myelination in the very preterm brain. AJNR Am J Neuroradiol 23:872–881
Takala TI, Makela E, Suominen P et al (2010) Blood cell and iron status analytes of preterm and full-term infants from 20 weeks onwards during the first year of life. Clin Chem Lab Med 48:1295–1301
Thompson RA, Nelson CA (2001) Developmental science and the media. Early brain development. Am Psychol 56:5–15
Wang Y, Wu Y, Li T, Wang X, Zhu C (2019) Iron metabolism and brain development in premature infants. Front Physiol 10:463
Zhang Y, Shi F, Wu G, Wang L, Yap PT, Shen D (2016) Consistent spatial-temporal longitudinal atlas construction for developing infant brains. IEEE Trans Med Imaging 35:2568–2577
Zhang H, Lai C, Liu R et al (2019) Age-specific optimization of T1-weighted brain MRI throughout infancy. Neuroimage 199:387–395
Wang L, Gao Y, Shi F et al (2015) LINKS: learning-based multi-source IntegratioN frameworK for Segmentation of infant brain images. Neuroimage 108:160–172
Li G, Nie J, Wang L et al (2013) Mapping region-specific longitudinal cortical surface expansion from birth to 2 years of age. Cereb Cortex 23:2724–2733
Acknowledgements
We are grateful to Mr. Yuta Urushibata, MSci, Siemens Healthcare K. K., for protocol optimization.
Funding
This work was supported by JSPS KAKENHI Grant Number 22K07746, 19K17266, 21K15826, 21K15623, 21K20834, and the Kyoto University Research Fund for Young Scientists (Start-Up) FY2021.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Yuji Nakamoto.
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was waived by the Institutional Review Board.
Ethical approval
Institutional Review Board approval was obtained. This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by Kyoto University Graduate School and the Faculty of Medicine, Ethics Committee (R3036).
Methodology
• retrospective
• cross-sectional study
• performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
ESM 1
(DOCX 2512 kb)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Otani, S., Fushimi, Y., Iwanaga, K. et al. Evaluation of deep gray matter for early brain development using quantitative susceptibility mapping. Eur Radiol 33, 4488–4499 (2023). https://doi.org/10.1007/s00330-022-09267-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-022-09267-4